Ann Surg Treat Res.
2017 Aug;93(2):88-97. 10.4174/astr.2017.93.2.88.
Meaningful standard of reference for appendiceal perforation: pathology, surgery, or both?
- Affiliations
-
- 1Department of Radiology, Daejin Medical Center, Bundang Jesaeng General Hospital, Seongnam, Korea.
- 2Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. misung70@gmail.com
- 3Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 4Division of Statistics, Medical Research Collaborating Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 6Program in Biomedical Radiation Sciences, Department of Transdisciplinary Studies, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea.
- 7Department of Radiology, Hanyang University Hospital, Seoul, Korea.
- 8Department of Radiology, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea.
- KMID: 2387339
- DOI: http://doi.org/10.4174/astr.2017.93.2.88
Abstract
- PURPOSE
This retrospective study was aimed to determine if appendiceal perforation identified pathologically but not surgically is clinically meaningful.
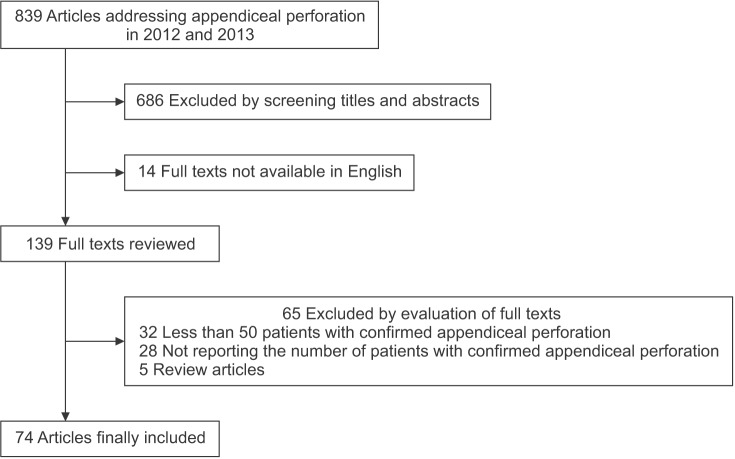
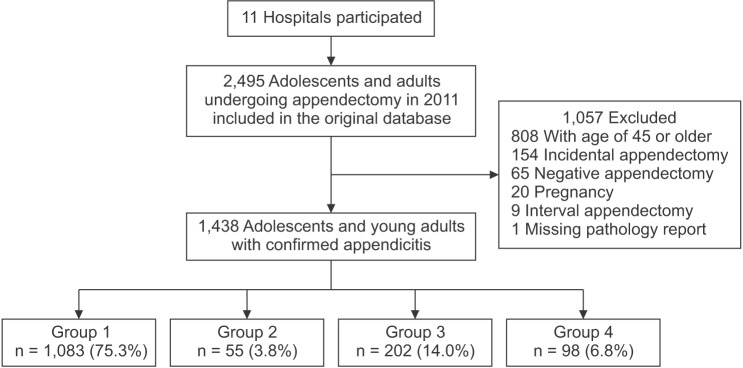
METHODS
The study consists of 2 parts. First, we reviewed 74 studies addressing appendiceal perforation published in 2012 and 2013. Second, in a cross-sectional study, we classified 1,438 adolescents and adults (mean age, 29.3 ± 8.4 years; 785 men) with confirmed appendicitis as "nonperforation" (n = 1,083, group 1), "pathologically-identified perforation" (n = 55, group 2), "surgically-identified perforation" (n = 202, group 3), or "pathologically- and surgically-identified perforation" (n = 98, group 4). The 4 groups were compared for the frequency of laparoscopic appendectomy and the length of hospital stay using multivariable logistic regression analyses.
RESULTS
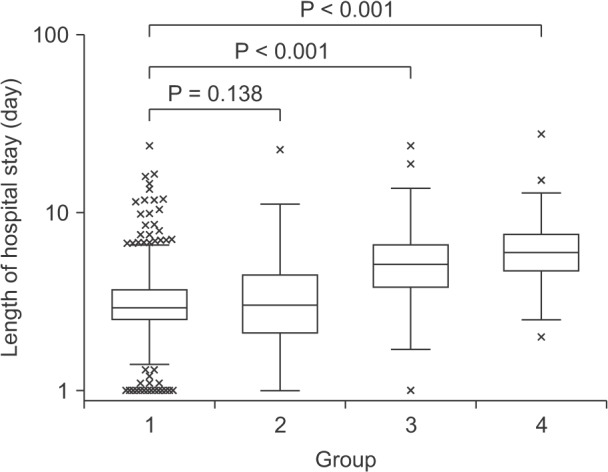
The reference standard for appendiceal perforation was frequently missing or inconsistent in the previous studies. Laparoscopic appendectomies were less frequent in groups 3 (52.5%, P = 0.001) and 4 (65%, P = 0.040) than in group 1 (70.7%), while group 2 (73%, P = 0.125) did not significantly differ from group 1. Median hospital stays were 2.9, 3.0, 5.1, and 6.0 days for groups 1-4, respectively. Prolonged hospital stay (≥3.7 days) was more frequent in groups 3 (77.7%, P < 0.001) and 4 (89%, P < 0.001) than in group 1 (23.4%), while group 2 (35%, P = 0.070) did not significantly differ from group 1.
CONCLUSION
We recommend using surgical rather than pathologic findings as the reference standard for the presence of appendiceal perforation in future investigations.
Keyword
MeSH Terms
Figure
Reference
-
1. Luckmann R. Incidence and case fatality rates for acute appendicitis in California. A population-based study of the effects of age. Am J Epidemiol. 1989; 129:905–918. PMID: 2784936.2. Velanovich V, Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am Surg. 1992; 58:264–269. PMID: 1586087.3. Andersson R, Hugander A, Thulin A, Nystrom PO, Olaison G. Indications for operation in suspected appendicitis and incidence of perforation. BMJ. 1994; 308:107–110. PMID: 8298378.
Article4. Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994; 331:444–449. PMID: 7880234.
Article5. Ponsky TA, Huang ZJ, Kittle K, Eichelberger MR, Gilbert JC, Brody F, et al. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004; 292:1977–1982. PMID: 15507583.
Article6. Salminen P, Paajanen H, Rautio T, Nordstrom P, Aarnio M, Rantanen T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The APPAC Randomized Clinical Trial. JAMA. 2015; 313:2340–2348. PMID: 26080338.7. Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012; 344:e2156. PMID: 22491789.
Article8. Horstmann R, Tiwisina C, Classen C, Palmes D, Gillessen A. Laparoscopic versus open appendectomy: which factors influence the decision between the surgical techniques? Zentralbl Chir. 2005; 130:48–54. PMID: 15717240.9. Gorter RR, Eker HH, Gorter-Stam MA, Abis GS, Acharya A, Ankersmit M, et al. Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc. 2016; 30:4668–4690. PMID: 27660247.
Article10. Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011; 154:789–796. W-291. PMID: 21690593.
Article11. Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000; 215:337–348. PMID: 10796905.
Article12. St Peter SD, Sharp SW, Holcomb GW 3rd, Ostlie DJ. An evidence-based definition for perforated appendicitis derived from a prospective randomized trial. J Pediatr Surg. 2008; 43:2242–2245. PMID: 19040944.13. Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012; 366:1596–1605. PMID: 22533576.
Article14. Ahn S. LOCAT group. LOCAT (low-dose computed tomography for appendicitis trial) comparing clinical outcomes following low- vs standard-dose computed tomography as the first-line imaging test in adolescents and young adults with suspected acute appendicitis: study protocol for a randomized controlled trial. Trials. 2014; 15:28. PMID: 24438500.
Article15. Park JH. LOCAT Group. Diagnostic imaging utilization in cases of acute appendicitis: multi-center experience. J Korean Med Sci. 2014; 29:1308–1316. PMID: 25246752.
Article16. Health Insurance Review & Assessment Service. Hospital survey [Internet]. Wonju: Health Insurance Review & Assessment Service;2014. cited 2015 June 27. Available from: http://www.hira.or.kr/main.do.17. National Health Insurance Service. 2014 Statistics on major surgeries in Korea [Internet]. Wonju: National Health Insurance Service;2015. cited 2016 July 23. Available from: http://www.nhis.or.kr/menu/retriveMenuSet.xx?menuId=F3326.18. Rosai J. Rosai and Ackerman's surgical pathology. 10th ed. St. Louis (MO): Mosby;2011. p. Appendix. p. 714-8.19. Fenoglio-Preiser CM, Noffsinger AE, Stemmermann GN, Lantz PE, Isaacson PG. Gastrointestinal pathology: an atlas and textz. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins;2008. p. Non-neoplastic diseases of the appendix. p. 497-524.20. Andersson MN, Andersson RE. Causes of short-term mortality after appendectomy: a population-based case-controlled study. Ann Surg. 2011; 254:103–107. PMID: 21577090.21. Maa J, Kirkwood KS. The appendix. In : Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston textbook of surgery: the biological basis of modern surgical practice. 19th ed. Philadelphia(PA): Elsevier/Saunders Inc;2012. p. 1279–1293.22. Yeh CC, Wu SC, Liao CC, Su LT, Hsieh CH, Li TC. Laparoscopic appendectomy for acute appendicitis is more favorable for patients with comorbidities, the elderly, and those with complicated appendicitis: a nationwide population-based study. Surg Endosc. 2011; 25:2932–2942. PMID: 21424194.
Article23. Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007; 18:805–835. PMID: 18049195.24. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001; 345:663–668. PMID: 11547721.
Article25. Park CS, Chang MS, Park IA, Kim YI, Choe G. Pathologic analysis of 2159 cases of appendix. Korean J Pathol. 2000; 34:39–49.26. Kim SY, Lee KH, Kim K, Kim TY, Lee HS, Hwang SS, et al. Acute appendicitis in young adults: low- versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology. 2011; 260:437–445. PMID: 21633052.
Article27. Kim MS, Park HW, Park JY, Park HJ, Lee SY, Hong HP, et al. Differentiation of early perforated from nonperforated appendicitis: MDCT findings, MDCT diagnostic performance, and clinical outcome. Abdom Imaging. 2014; 39:459–466. PMID: 24633221.
Article28. Tiwari MM, Reynoso JF, Tsang AW, Oleynikov D. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg. 2011; 254:927–932. PMID: 21804381.
Article29. Barrett ML, Hines AL, Andrews RM. Trends in rates of perforated appendix, 2001-2010. HCUP Statistical Brief #159. July 2013 [Internet]. Rockville (MD): Healthcare Cost and Utilization Project;2017. cited 2015 May 8. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb159.pdf.