Yonsei Med J.
2014 Mar;55(2):410-416.
The Usefulness of the Kurashiki Prehospital Stroke Scale in Identifying Thrombolytic Candidates in Acute Ischemic Stroke
- Affiliations
-
- 1Department of Emergency Medicine, Yonsei University College of Medicine, Seoul, Korea. youjsmd@yuhs.ac
- 2Department of Emergency Medicine, Graduate School of Medicine, Kangwon National University, Chuncheon, Korea.
- 3Department of Research Affairs, Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Emergency Medicine, Changwon Fatima Hospital, Changwon, Korea.
- 5Department of Emergency Medicine, Bundang CHA Hospital, CHA University College of Medicine, Seongnam, Korea.
Abstract
- PURPOSE
The severity of a stroke cannot be described by widely used prehospital stroke scales. We investigated the usefulness of the Kurashiki Prehospital Stroke Scale (KPSS) for assessing the severity of stroke, compared to the National Institutes of Health Stroke Scale (NIHSS), in candidate patients for intravenous or intra-arterial thrombolysis who arrived at the hospital within 6 hours of symptom onset.
MATERIALS AND METHODS
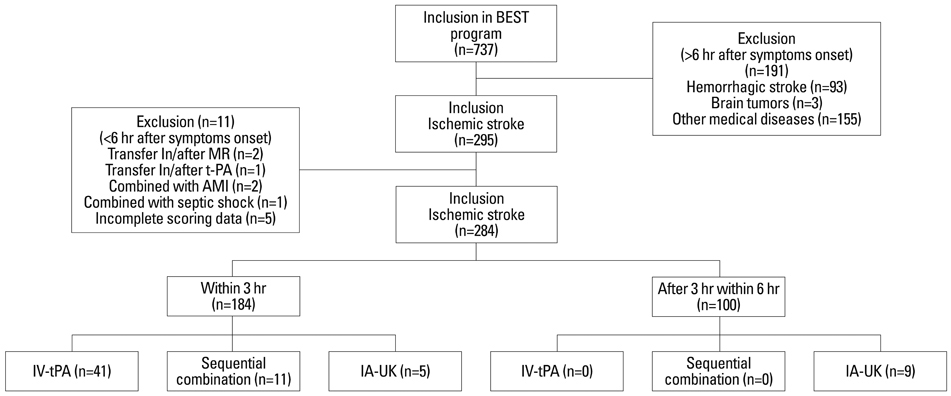
We retrospectively analyzed a prospective registry database of consecutive patients included in the Emergency Stroke Therapy program. In the emergency department, the KPSS was assessed by emergency medical technicians. A cutoff KPSS score was estimated for candidates of thrombolysis by comparing KPSS and NIHSS scores, as well as for patients who actually received thrombolytic therapy. Clinical outcomes were compared between patients around the estimated cut-off. The independent predictors of outcomes were determined using multivariate logistic regression analysis.
RESULTS
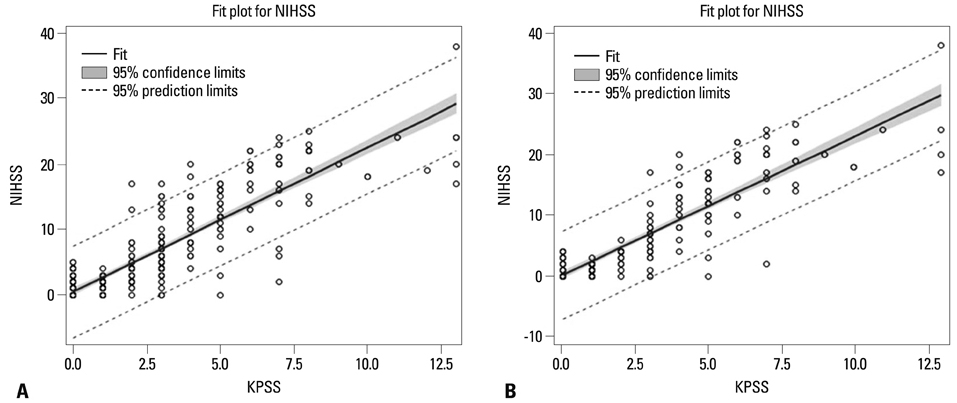
Excellent correlations were demonstrated between KPSS and NIHSS within 6 hours (R=0.869) and 3 hours (R=0.879) of hospital admission. The optimal threshold value was a score of 3 on the KPSS in patients within 3 hours and 6 hours by Youden's methods. Significant associations with a KPSS score > or =3 were revealed for actual intravenous administration of tissue plasminogen activator (IV-tPA) usage [odds ratio (OR) 125.598; 95% confidence interval (CI) 16.443-959.368, p<0.0001] and actual IV-tPA or intra-arterial urokinase (IA-UK) usage (OR 58.733; 95% CI 17.272-199.721, p<0.0001).
CONCLUSION
The KPSS is an effective prehospital stroke scale for identifying candidates for IV-tPA and IA-UK, as indicated by excellent correlation with the NIHSS, in the assessment of stroke severity in acute ischemic stroke.
MeSH Terms
-
Administration, Intravenous
Confidence Intervals
Emergencies
Emergency Medical Services
Emergency Medical Technicians
Emergency Service, Hospital
Humans
Logistic Models
Methods
National Institutes of Health (U.S.)
Prospective Studies
Retrospective Studies
Stroke*
Thrombolytic Therapy
Tissue Plasminogen Activator
Urokinase-Type Plasminogen Activator
Weights and Measures
Tissue Plasminogen Activator
Urokinase-Type Plasminogen Activator
Figure
Reference
-
1. Jung S, Kwon SB, Hwang SH, Noh JW, Lee YK. Ischemic stroke among the patients with end-stage renal disease who were undergoing maintenance dialysis. Yonsei Med J. 2012; 53:894–900.
Article2. Jauch EC, Cucchiara B, Adeoye O, Meurer W, Brice J, Chan YY, et al. Part 11: adult stroke: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122:18 Suppl 3. S818–S828.3. Iguchi Y, Kimura K, Watanabe M, Shibazaki K, Aoki J. Utility of the Kurashiki Prehospital Stroke Scale for hyperacute stroke. Cerebrovasc Dis. 2011; 31:51–56.
Article4. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 2007; 38:1655–1711.
Article5. Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med. 1999; 33:373–378.
Article6. Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000; 31:71–76.7. Nam HS, Han SW, Ahn SH, Lee JY, Choi HY, Park IC, et al. Improved time intervals by implementation of computerized physician order entry-based stroke team approach. Cerebrovasc Dis. 2007; 23:289–293.
Article8. Llanes JN, Kidwell CS, Starkman S, Leary MC, Eckstein M, Saver JL. The Los Angeles Motor Scale (LAMS): a new measure to characterize stroke severity in the field. Prehosp Emerg Care. 2004; 8:46–50.9. Kimura K, Inoue T, Iguchi Y, Shibazaki K. Kurashiki prehospital stroke scale. Cerebrovasc Dis. 2008; 25:189–191.
Article10. Heo JH, Kim YD, Nam HS, Hong KS, Ahn SH, Cho HJ, et al. A computerized in-hospital alert system for thrombolysis in acute stroke. Stroke. 2010; 41:1978–1983.
Article11. Ogawa A, Mori E, Minematsu K, Taki W, Takahashi A, Nemoto S, et al. Randomized trial of intraarterial infusion of urokinase within 6 hours of middle cerebral artery stroke: the middle cerebral artery embolism local fibrinolytic intervention trial (MELT) Japan. Stroke. 2007; 38:2633–2639.
Article12. Lee KY, Kim DI, Kim SH, Lee SI, Chung HW, Shim YW, et al. Sequential combination of intravenous recombinant tissue plasminogen activator and intra-arterial urokinase in acute ischemic stroke. AJNR Am J Neuroradiol. 2004; 25:1470–1475.13. IMS Study Investigators. Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the Interventional Management of Stroke Study. Stroke. 2004; 35:904–911.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- Treatment of Acute Ischemic Stroke: Thrombolysis
- Performance Rate of Thrombolytic Therapy and Acute Prognosis of Hyperacute Ischemic Stroke
- A Case of Hemoperitoneum after Intraarterial Urokinase Infusion for Acute Ischemic Stroke
- Guideline for intra-arterial thrombolysis of hyperacute ischemic stroke patients: Preliminary Report