Ann Lab Med.
2017 Sep;37(5):426-433. 10.3343/alm.2017.37.5.426.
Human Papillomavirus Genotype Distribution Among 18,815 Women in 13 Korean Cities and Relationship With Cervical Cytology Findings
- Affiliations
-
- 1Department of Laboratory Medicine and Health Promotion Research Institute, Korea Association of Health Promotion, Seoul, Korea. cellonah@hanmail.net
- 2MEDIcheck LAB, Korea Association of Health Promotion, Cheongju, Korea.
- KMID: 2383919
- DOI: http://doi.org/10.3343/alm.2017.37.5.426
Abstract
- BACKGROUND
The prevalence and genotype distribution of Human papillomavirus (HPV) infection vary depending on geographical region and the immunity provided by vaccines. This study aimed to clarify the recent prevalence and genotype distribution of HPV according to age and cervical cytology findings in Korea.
METHODS
This study included 18,815 health examinees that underwent cervical cytology and HPV genotyping tests at 16 centers of Korean Association of Health Promotion in 13 cities in Korea, between January 2014 and October 2015. HPV was genotyped by using multiplex PCR (Anyplex II HPV 28, Seegene, Korea), which detects 19 high-risk HPVs (HR-HPV) and nine low-risk HPVs (LR-HPV).
RESULTS
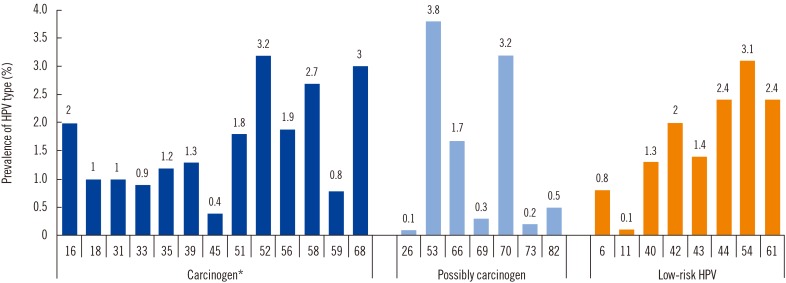
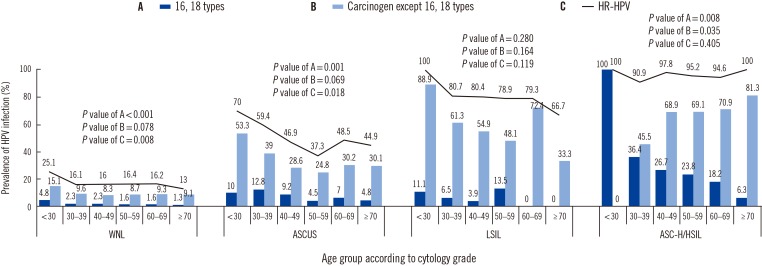
Overall HPV prevalence was 27.8%, with 22.2% HR-HPV and 11.4% LR-HPV. The five most common carcinogens were HPV 52 (3.2%), 58 (2.7%), 16 (2.0%), 56 (1.9%), and 51 (1.8%). The five most common HR-HPVs in normal cytology samples were HPV 53, 68, 70, 52, and 58, while HPV 16, 52, 58, 33, and 31 were prevalent in high grade squamous intraepithelial lesions (HSIL). In atypical squamous cells of undetermined significance (ASCUS), the prevalence of HR-HPV varied with age; it was highest in those aged <30 yr, declining to a minimum at age 50-59 yr, and then increasing in older women (P<0.05).
CONCLUSIONS
The prevalence and distribution of HR-HPV varied with age and cervical cytology findings. This information would be helpful in the development of cervical cancer prevention policies.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Updates on Cancer Epidemiology in Korea, 2018
Sun-Seog Kweon
Chonnam Med J. 2018;54(2):90-100. doi: 10.4068/cmj.2018.54.2.90.
Reference
-
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108. PMID: 25651787.2. National Cancer Center. Annual report of cancer statistics in Korea in 2014. Goyang, Korea: National Cancer Center;2014. p. 20–22.3. Meijer CJ, Snijders PJ, Castle PE. Clinical utility of HPV genotyping. Gynecol Oncol. 2006; 103:12–17. PMID: 16934860.4. Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain J, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. Am J Clin Pathol. 2012; 137:516–542. PMID: 22431528.5. Bernard HU, Burk RD, Chen Z, van Doorslaer K, zur Hausen H, de Villiers EM. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology. 2010; 401:70–79. PMID: 20206957.6. de Sanjosé S, Diaz M, Castellsagué X, Clifford G, Bruni L, Muñoz N, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis. 2007; 7:453–459. PMID: 17597569.7. Bae JH, Lee SJ, Kim CJ, Hur SY, Park YG, Lee WC, et al. Human papillomavirus (HPV) type distribution in Korean women: a meta-analysis. J Microbiol Biotechnol. 2008; 18:788–794. PMID: 18467878.8. Kim MJ, Kim JJ, Kim S. Type-specific prevalence of high-risk human papillomavirus by cervical cytology and age: Data from the health check-ups of 7,014 Korean women. Obstet Gynecol Sci. 2013; 56:110–120. PMID: 24327989.9. Shin HR, Lee DH, Herrero R, Smith JS, Vaccarella S, Hong SH, et al. Prevalence of human papillomavirus infection in women in Busan, South Korea. Int J Cancer. 2003; 103:413–421. PMID: 12471626.10. Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002; 287:2114–2119. PMID: 11966386.11. Schiffman M, Clifford G, Buonaguro FM. Classification of weakly carcinogenic human papillomavirus types: addressing the limits of epidemiology at the borderline. Infect Agent Cancer. 2009; 4:8. PMID: 19486508.12. IARC. Agents classified by the IARC monographs, vol. 1-118. Updated on May 2017. http://monographs.iarc.fr/ENG/Classification/index.php.13. Kim JK, Jeon JS, Lee CH, Kim JW. Prevalence and genotype distribution of human papillomavirus in Cheonan, Korea. J Microbiol Biotechnol. 2014; 24:1143–1147. PMID: 24861343.14. Lee EH, Um TH, Chi HS, Hong YJ, Cha YJ. Prevalence and distribution of human papillomavirus infection in Korean women as determined by restriction fragment mass polymorphism assay. J Korean Med Sci. 2012; 27:1091–1097. PMID: 22969258.15. Rhee JE, Shin MY, Kim CM, Kee HY, Chung JK, Min SK, et al. Prevalence of human papillomavirus infection and genotype distribution among high-risk Korean women for prospecting the strategy of vaccine development. Virol J. 2010; 7:201. PMID: 20738861.16. Mesher D, Panwar K, Thomas SL, Beddows S, Soldan K. Continuing reductions in HPV 16/18 in a population with high coverage of bivalent HPV vaccination in England: an ongoing cross-sectional study. BMJ Open. 2016; 6:e009915.17. Markowitz LE, Hariri S, Lin C, Dunne EF, Steinau M, McQuillan G, et al. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003-2010. J Infect Dis. 2013; 208:385–393. PMID: 23785124.18. Tabrizi SN, Brotherton JM, Kaldor JM, Skinner SR, Cummins E, Liu B, et al. Fall in human papillomavirus prevalence following a national vaccination program. J Infect Dis. 2012; 206:1645–1651. PMID: 23087430.19. Heard I, Tondeur L, Arowas L, Falguières M, Demazoin MC, Favre M. Human papillomavirus types distribution in organised cervical cancer screening in France. PLoS One. 2013; 8:e79372. PMID: 24244490.20. Howell-Jones R, Bailey A, Beddows S, Sargent A, de Silva N, Wilson G, et al. Multi-site study of HPV type-specific prevalence in women with cervical cancer, intraepithelial neoplasia and normal cytology, in England. Br J Cancer. 2010; 103:209–216. PMID: 20628396.21. Bosch FX, Burchell AN, Schiffman M, Giuliano AR, de Sanjose S, Bruni L, et al. Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine. 2008; 26(S10):K1–K16. PMID: 18847553.22. Malagón T, Drolet M, Boily MC, Franco EL, Jit M, Brisson J, et al. Cross-protective efficacy of two human papillomavirus vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012; 12:781–789. PMID: 22920953.23. Wheeler CM, Castellsagué X, Garland SM, Szarewski A, Paavonen J, Naud P, et al. Cross-protective efficacy of HPV-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by non-vaccine oncogenic HPV types: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 2012; 13:100–110. PMID: 22075170.24. Franceschi S, Herrero R, Clifford GM, Snijders PJ, Arslan A, Anh PT, et al. Variations in the age-specific curves of human papillomavirus prevalence in women worldwide. Int J Cancer. 2006; 119:2677–2684. PMID: 16991121.25. Gravitt PE, Rositch AF, Silver MI, Marks MA, Chang K, Burke AE, et al. A cohort effect of the sexual revolution may be masking an increase in human papillomavirus detection at menopause in the United States. J Infect Dis. 2013; 207:272–280. PMID: 23242540.26. Althoff KN, Paul P, Burke AE, Viscidi R, Sangaramoorthy M, Gravitt PE. Correlates of cervicovaginal human papillomavirus detection in perimenopausal women. J Womens Health (Larchmt). 2009; 18:1341–1346. PMID: 19702476.27. Muñoz N, Méndez F, Posso H, Molano M, van den Brule AJ, Ronderos M, et al. Incidence, duration, and determinants of cervical human papillomavirus infection in a cohort of Colombian women with normal cytological results. J Infect Dis. 2004; 190:2077–2087. PMID: 15551205.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Human Papillomavirus Prevalence and Genotype Distribution among HIV-Infected Women in Korea
- Evaluation of clinical usefulness of HPV-16 and HPV-18 genotyping for cervical cancer screening
- Type-specific prevalence of high-risk human papillomavirus by cervical cytology and age: Data from the health check-ups of 7,014 Korean women
- Prevalence of human papillomavirus genotypes and precancerous cervical lesions in a screening population in the Republic of Korea, 2014–2016
- Human Papillomavirus Prevalence and Type Distribution Among 968 Women in South Korea