Ann Rehabil Med.
2017 Feb;41(1):51-57. 10.5535/arm.2017.41.1.51.
Accuracy of Ultrasound-Guided and Non-ultrasound-Guided Botulinum Toxin Injection Into Cadaver Salivary Glands
- Affiliations
-
- 1Department of Rehabilitation Medicine, St. Paul's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. coltrane@catholic.ac.kr
- KMID: 2383677
- DOI: http://doi.org/10.5535/arm.2017.41.1.51
Abstract
OBJECTIVE
To compare the accuracy of ultrasound (US)-guided and non-US-guided botulinum toxin (BTX) injection into the salivary glands (parotid and submandibular glands) of cadavers.
METHODS
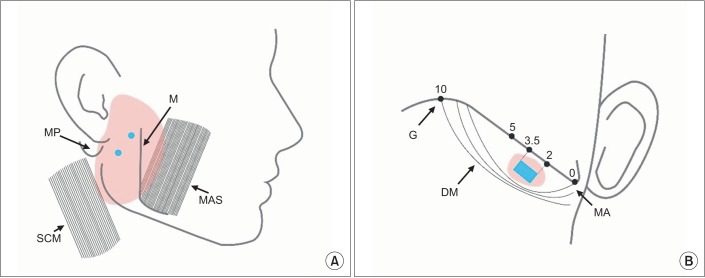
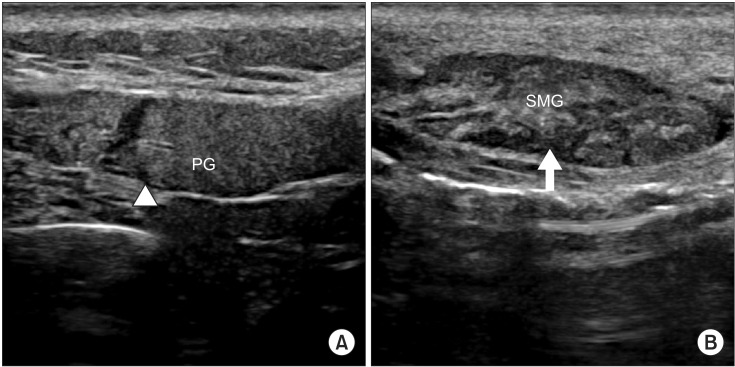
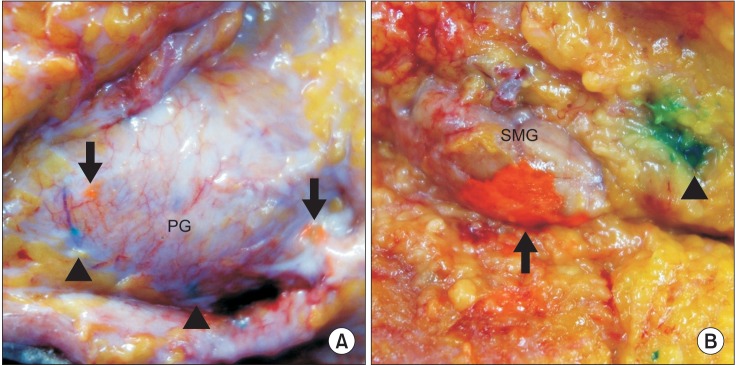
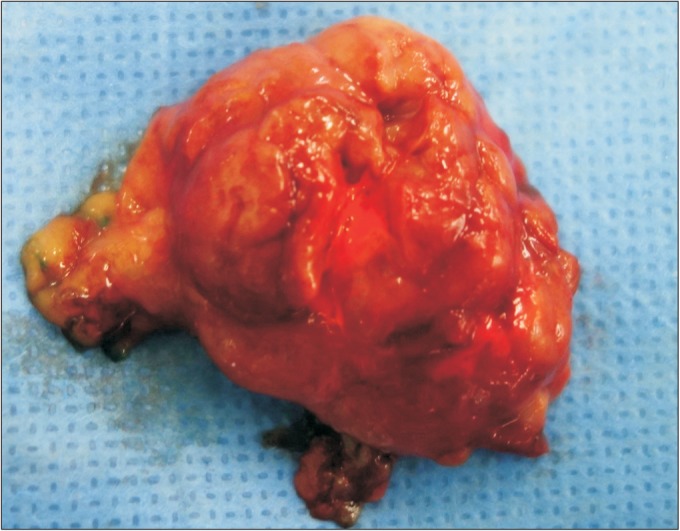
Two rehabilitation physician injected dye into three sites in the salivary glands (two sites in the parotid gland and one site in the submandibular gland) on one side of each cadaver (one was injected on the right side, while the other was injected on the left side), using either a non-US-guided injection procedure based on superficial landmarks or a US-guided procedure. Orange dye was used for the US-guided procedure, and green dye was used for the blind procedure. Two physicians uninvolved with the injection procedures and who were blinded to the method of injection dissected the cadavers to identify whether the dye was accurately injected into each target site.
RESULTS
The accuracies of the blind and US-guided injections into the parotid gland were 79.17% and 95.83%, respectively. In the submandibular gland, the accuracies of the blind and US-guided injections were 50.00% and 91.67%, respectively. The difference in accuracy between the two procedures was statistically significant only in the submandibular gland (p=0.025). There were no significant differences in the accuracy of US-guided and non-US-guided injections between the two physicians for the two sites in the parotid gland (p=0.278 and p=0.146, respectively).
CONCLUSION
US-guided BTX injection into the submandibular gland offers significantly greater accuracy over blind injection. For the treatment of drooling by injecting BTX into the submandibular gland, clinicians should consider using US guidance for improved accuracy.
Keyword
MeSH Terms
Figure
Reference
-
1. Garnock-Jones KP. Glycopyrrolate oral solution: for chronic, severe drooling in pediatric patients with neurologic conditions. Paediatr Drugs. 2012; 14:263–269. PMID: 22646067.2. Jongerius PH, van Hulst K, van den Hoogen FJ, Rotteveel JJ. The treatment of posterior drooling by botulinum toxin in a child with cerebral palsy. J Pediatr Gastroenterol Nutr. 2005; 41:351–353. PMID: 16131993.
Article3. Lakraj AA, Moghimi N, Jabbari B. Sialorrhea: anatomy, pathophysiology and treatment with emphasis on the role of botulinum toxins. Toxins (Basel). 2013; 5:1010–1031. PMID: 23698357.
Article4. Meningaud JP, Pitak-Arnnop P, Chikhani L, Bertrand JC. Drooling of saliva: a review of the etiology and management options. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:48–57. PMID: 16360607.
Article5. Bushara KO. Sialorrhea in amyotrophic lateral sclerosis: a hypothesis of a new treatment: botulinum toxin A injections of the parotid glands. Med Hypotheses. 1997; 48:337–339. PMID: 9160288.6. Sriskandan N, Moody A, Howlett DC. Ultrasound-guided submandibular gland injection of botulinum toxin for hypersalivation in cerebral palsy. Br J Oral Maxillofac Surg. 2010; 48:58–60. PMID: 19371986.
Article7. Dogu O, Apaydin D, Sevim S, Talas DU, Aral M. Ultrasound-guided versus ‘blind’ intraparotid injections of botulinum toxin-A for the treatment of sialorrhoea in patients with Parkinson's disease. Clin Neurol Neurosurg. 2004; 106:93–96. PMID: 15003297.
Article8. Lagalla G, Millevolte M, Capecci M, Provinciali L, Ceravolo MG. Long-lasting benefits of botulinum toxin type B in Parkinson's disease-related drooling. J Neurol. 2009; 256:563–567. PMID: 19401804.
Article9. Lee JH, Lee BN, Kwon SO, Chung RH, Han SH. Anatomical localization of submandibular gland for botulinum toxin injection. Surg Radiol Anat. 2010; 32:945–949. PMID: 20221760.
Article10. Scully C, Limeres J, Gleeson M, Tomas I, Diz P. Drooling. J Oral Pathol Med. 2009; 38:321–327. PMID: 19236564.
Article11. Jongerius PH, Joosten F, Hoogen FJ, Gabreels FJ, Rotteveel JJ. The treatment of drooling by ultrasound-guided intraglandular injections of botulinum toxin type A into the salivary glands. Laryngoscope. 2003; 113:107–111. PMID: 12514392.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of Ultrasound-Guided and Non-guided Botulinum Toxin Injection Into Neck Muscles Involved in Cervical Dystonia: A Cadaveric Study
- Effects of Botulinum Toxin A Injection into Salivary Glands of Patients with Brain Lesion Suffering from Posterior Drooling
- Effect of Botulinum Toxin Type A on Morphology of Salivary Glands in Patients with Cerebral Palsy
- Usefulness of Ultrasound for Carpal Tunnel Syndrome Proven in Meta-Analysis Studies
- Feasibility of Ultrasound Guided Atlanto-occipital Joint Injection