Phase I Dose-Escalation Study of Proton Beam Therapy for Inoperable Hepatocellular Carcinoma
- Affiliations
-
- 1Center for Liver Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea. jwpark@ncc.re.kr
- KMID: 2380388
- DOI: http://doi.org/10.4143/crt.2013.218
Abstract
- PURPOSE
The purpose of this study is to determine the optimal dose of proton beam therapy (PBT) in hepatocellular carcinoma (HCC) patients.
MATERIALS AND METHODS
Inoperable HCC patients who had naive, recurrent, or residual tumor to treatment were considered eligible for PBT. Patients received PBT with 60 GyE in 20 fractions (dose level 1; equivalent dose in 2 Gy fractions [EQD2], 65 GyE10); 66 GyE in 22 fractions (dose level 2; EQD2, 71.5 GyE10); or 72 GyE in 24 fractions (dose level 3; EQD2, 78 GyE10). Dose-limiting toxicity was determined by grade > or = 3 acute toxicity.
RESULTS
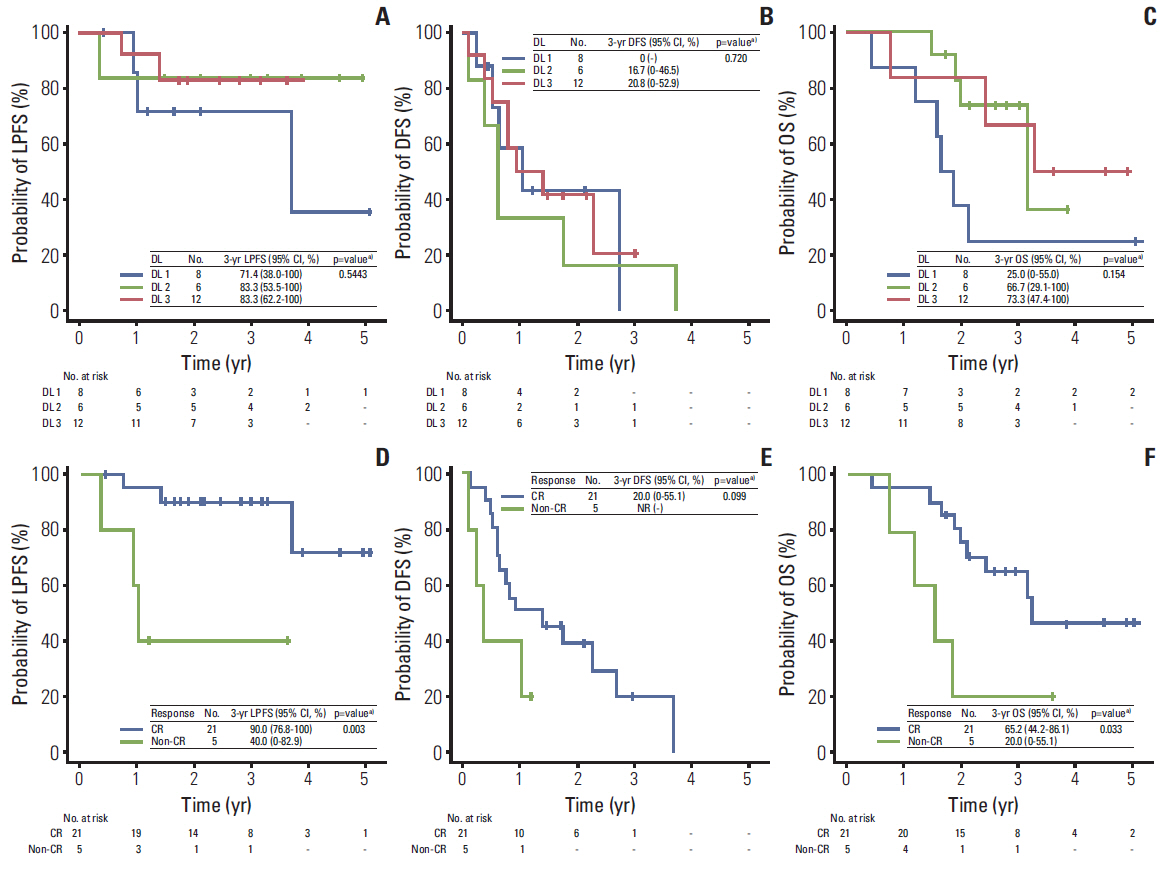
Twenty-seven patients were enrolled; eight, seven, and 12 patients were treated with dose levels 1, 2, and 3, respectively. Overall, treatment was well tolerated, with no dose-limiting toxicities. The complete response (CR) rates of primary tumors after PBT for dose levels 1, 2, and 3 were 62.5% (5/8), 57.1% (4/7), and 100% (12/12), respectively (p=0.039). The 3-and 5-year local progression-free survival (LPFS) rates among 26 patients, excluding one patient who underwent liver transplantation after PBT due to its probable significant effect on disease control, were 79.9% and 63.9%, respectively, and the 3-and 5-year overall survival rates were 56.4% and 42.3%, respectively. The 3-year LPFS rate was significantly higher in patients who achieved CR than in those who did not (90% vs. 40%, p=0.003).
CONCLUSION
PBT is safe and effective and an EQD2 > or = 78 GyE10 should be delivered for achievement of local tumor control.
MeSH Terms
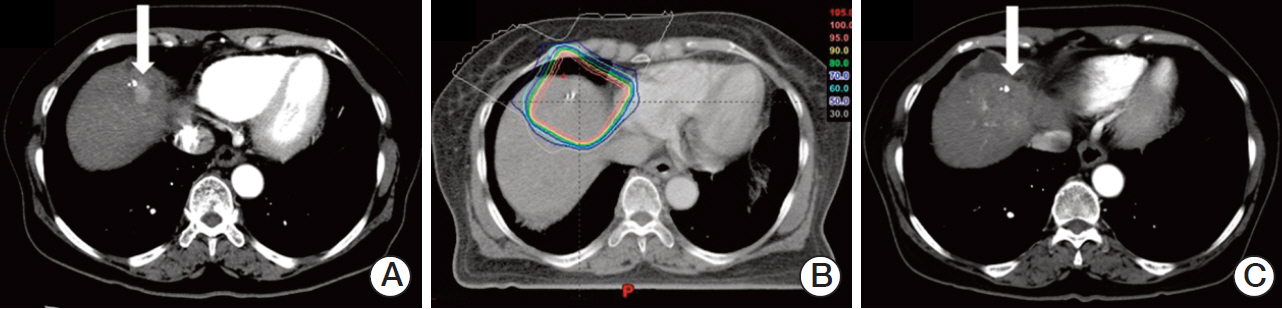
Figure
Cited by 5 articles
-
2018 Korean Liver Cancer Association–National Cancer Center Korea Practice Guidelines for the Management of Hepatocellular Carcinoma
,
Korean J Radiol. 2019;20(7):1042-1113. doi: 10.3348/kjr.2019.0140.Patterns of Proton Beam Therapy Use in Clinical Practice between 2007 and 2019 in Korea
Sung Uk Lee, Kyungmi Yang, Sung Ho Moon, Yang-Gun Suh, Gyu Sang Yoo
Cancer Res Treat. 2021;53(4):935-943. doi: 10.4143/crt.2021.409.2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
J Liver Cancer. 2023;23(1):1-120. doi: 10.17998/jlc.2022.11.07.Current perspectives on radiotherapy in hepatocellular carcinoma management: a comprehensive review
Dowook Kim, Jun-Sang Kim
J Liver Cancer. 2024;24(1):33-46. doi: 10.17998/jlc.2024.02.26.Recent update of proton beam therapy for hepatocellular carcinoma: a systematic review and meta-analysis
Sun Hyun Bae, Won Il Jang, Hanna Rahbek Mortensen, Britta Weber, Mi Sook Kim, Morten Høyer
J Liver Cancer. 2024;24(2):286-302. doi: 10.17998/jlc.2024.06.26.
Reference
-
References
1. Shiina S, Teratani T, Obi S, Sato S, Tateishi R, Fujishima T, et al. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology. 2005; 129:122–30.
Article2. Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma < or =4 cm. Gastroenterology. 2004; 127:1714–23.3. Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002; 35:1164–71.
Article4. Llovet JM, Real MI, Montana X, Planas R, Coll S, Aponte J, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002; 359:1734–9.
Article5. Higuchi T, Kikuchi M, Okazaki M. Hepatocellular carcinoma after transcatheter hepatic arterial embolization: a histopathologic study of 84 resected cases. Cancer. 1994; 73:2259–67.
Article6. Bush DA, Hillebrand DJ, Slater JM, Slater JD. High-dose proton beam radiotherapy of hepatocellular carcinoma: preliminary results of a phase II trial. Gastroenterology. 2004; 127(5 Suppl 1):S189–93.
Article7. Chiba T, Tokuuye K, Matsuzaki Y, Sugahara S, Chuganji Y, Kagei K, et al. Proton beam therapy for hepatocellular carcinoma: a retrospective review of 162 patients. Clin Cancer Res. 2005; 11:3799–805.
Article8. Fukumitsu N, Sugahara S, Nakayama H, Fukuda K, Mizumoto M, Abei M, et al. A prospective study of hypofractionated proton beam therapy for patients with hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2009; 74:831–6.
Article9. Imada H, Kato H, Yasuda S, Yamada S, Yanagi T, Kishimoto R, et al. Comparison of efficacy and toxicity of short-course carbon ion radiotherapy for hepatocellular carcinoma depending on their proximity to the porta hepatis. Radiother Oncol. 2010; 96:231–5.
Article10. Kato H, Tsujii H, Miyamoto T, Mizoe JE, Kamada T, Tsuji H, et al. Results of the first prospective study of carbon ion radiotherapy for hepatocellular carcinoma with liver cirrhosis. Int J Radiat Oncol Biol Phys. 2004; 59:1468–76.
Article11. Kawashima M, Furuse J, Nishio T, Konishi M, Ishii H, Kinoshita T, et al. Phase II study of radiotherapy employing proton beam for hepatocellular carcinoma. J Clin Oncol. 2005; 23:1839–46.
Article12. Komatsu S, Fukumoto T, Demizu Y, Miyawaki D, Terashima K, Sasaki R, et al. Clinical results and risk factors of proton and carbon ion therapy for hepatocellular carcinoma. Cancer. 2011; 117:4890–904.
Article13. Mizumoto M, Tokuuye K, Sugahara S, Nakayama H, Fukumitsu N, Ohara K, et al. Proton beam therapy for hepatocellular carcinoma adjacent to the porta hepatis. Int J Radiat Oncol Biol Phys. 2008; 71:462–7.
Article14. Nakayama H, Sugahara S, Fukuda K, Abei M, Shoda J, Sakurai H, et al. Proton beam therapy for hepatocellular carcinoma located adjacent to the alimentary tract. Int J Radiat Oncol Biol Phys. 2011; 80:992–5.
Article15. Park JW; Korean Liver Cancer Study Group and National Cancer Center. Practice guideline for diagnosis and treatment of hepatocellular carcinoma. Korean J Hepatol. 2004; 10:88–98.16. Kim TH, Kim DY, Park JW, Kim SH, Choi JI, Kim HB, et al. Dose-volumetric parameters predicting radiation-induced hepatic toxicity in unresectable hepatocellular carcinoma patients treated with three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2007; 67:225–31.
Article17. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010; 30:52–60.
Article18. Ohara K, Okumura T, Tsuji H, Min M, Tatsuzaki H, Chiba T, et al. Clearance of parenchymal tumors following radiotherapy: analysis of hepatocellular carcinomas treated by proton beams. Radiother Oncol. 1996; 41:233–6.
Article19. Ueno S, Tanabe G, Nuruki K, Hamanoue M, Komorizono Y, Oketani M, et al. Prognostic performance of the new classification of primary liver cancer of Japan (4th edition) for patients with hepatocellular carcinoma: a validation analysis. Hepatol Res. 2002; 24:395–403.
Article20. Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999; 19:329–38.
Article21. Kawashima M, Kohno R, Nakachi K, Nishio T, Mitsunaga S, Ikeda M, et al. Dose-volume histogram analysis of the safety of proton beam therapy for unresectable hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2011; 79:1479–86.
Article22. Park KW, Park JW, Choi JI, Kim TH, Kim SH, Park HS, et al. Survival analysis of 904 patients with hepatocellular carcinoma in a hepatitis B virus-endemic area. J Gastroenterol Hepatol. 2008; 23:467–73.
Article23. Park KW, Park JW, Kim TH, Choi JI, Kim SH, Park HS, et al. Five-year survival analysis of a cohort of hepatocellular carcinoma patients who treated at the National Cancer Center, Korea. Korean J Hepatol. 2007; 13:530–42.
Article24. Kim YI, Park HC, Lim DH, Park HJ, Kang SW, Park SY, et al. Changes of the liver volume and the Child-Pugh score after high dose hypofractionated radiotherapy in patients with small hepatocellular carcinoma. Radiat Oncol J. 2012; 30:189–96.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current evidence and the potential role of proton beam therapy for hepatocellular carcinoma
- Radiation-induced Myositis after Proton Beam Therapy to Huge Hepatocellular Carcinoma
- Current role of proton beam therapy in patients with hepatocellular carcinoma
- A Case of Hepatocellular Carcinoma Treated by Proton Beam Therapy as 1st Choice
- Proton Beam Therapy