Ann Hepatobiliary Pancreat Surg.
2017 May;21(2):93-95. 10.14701/ahbps.2017.21.2.93.
Distal pancreatectomy with splenorenal shunt to preserve spleen in a cirrhotic patient
- Affiliations
-
- 1Division of General Surgery and Liver Transplantation, San Camillo Hospital, Rome, Italy. gblevisandri@gmail.com
- KMID: 2379108
- DOI: http://doi.org/10.14701/ahbps.2017.21.2.93
Abstract
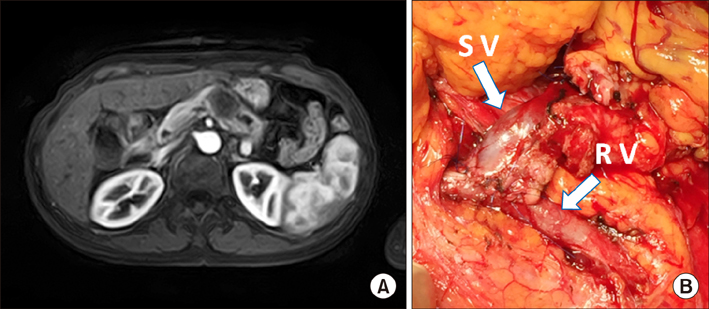
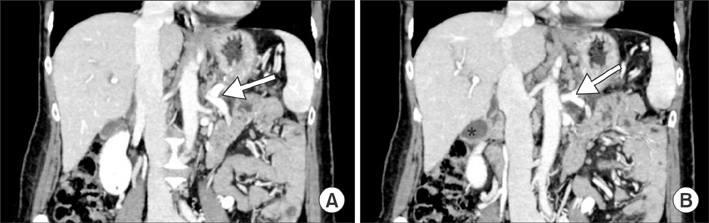
- At pancreatic ductal adenocarcinoma is an aggressive malignancy with a high recurrence rate. Due to its high potentials of local invasion and distant metastasis, surgical resection is the only means for possible long-term survival. Surgical treatment comprises a distal pancreatectomy with or without splenectomy. Surgery has been conventionally contraindicated for patients with cirrhosis and portal vein hepato-biliary hypertension. Splenorenal shunt was first described by Warren and colleagues, to prevent death from bleeding esophageal varices in a patient with a patent portal vein hypertension. A 55-year-old Caucasian woman presented with an incidental pancreatic tumor. In our case, the shunt was necessary to complete the corrective oncological surgery for pancreatic ductal adenocarcinoma. The main difficulty was the presence of portal hypertension due to liver cirrhosis Child A; moreover, preservation of the spleen was mandatory in this patient. We successfully performed a distal pancreatectomy without splenectomy through the help of splenorenal shunt to preserve venous circulation.
MeSH Terms
Figure
Reference
-
1. Zhan Q, Deng X, Weng Y, Jin J, Wu Z, Li H, et al. Outcomes of robotic surgery for pancreatic ductal adenocarcinoma. Chin J Cancer Res. 2015; 27:604–610.2. Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007; 297:267–277.3. Wysocka O, Kulbacka J, Saczko J. Adjuvant, neoadjuvant, and experimental regimens in overcoming pancreatic ductal adenocarcinoma. Prz Gastroenterol. 2016; 11:155–162.4. Regimbeau JM, Rebibo L, Dokmak S, Boher JM, Sauvanet A, Chopin-Laly X, et al. The short- and long-term outcomes of pancreaticoduodenectomy for cancer in child A patients are acceptable: a patient-control study from the Surgical French Association report for pancreatic surgery. J Surg Oncol. 2015; 111:776–783.5. Fuks D, Sabbagh C, Yzet T, Delcenserie R, Chatelain D, Regimbeau JM. Cirrhosis should not be considered as an absolute contraindication for pancreatoduodenectomy. Hepatogastroenterology. 2012; 59:881–883.6. Warren WD, Zeppa R, Fomon JJ. Selective trans-splenic decompression of gastroesophageal varices by distal splenorenal shunt. Ann Surg. 1967; 166:437–455.7. El Nakeeb A, Sultan AM, Salah T, El Hemaly M, Hamdy E, Salem A, et al. Impact of cirrhosis on surgical outcome after pancreaticoduodenectomy. World J Gastroenterol. 2013; 19:7129–7137.8. Warnick P, Mai I, Klein F, Andreou A, Bahra M, Neuhaus P, et al. Safety of pancreatic surgery in patients with simultaneous liver cirrhosis: a single center experience. Pancreatology. 2011; 11:24–29.9. Capussotti L, Ferrero A, Viganò L, Muratore A, Polastri R, Bouzari H. Portal hypertension: contraindication to liver surgery? World J Surg. 2006; 30:992–999.10. Vinet E, Perreault P, Bouchard L, Bernard D, Wassef R, Richard C, et al. Transjugular intrahepatic portosystemic shunt before abdominal surgery in cirrhotic patients: a retrospective, comparative study. Can J Gastroenterol. 2006; 20:401–404.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spleen Preservation in Laparoscopic Distal Pancreatectomy for Solitary Pseudopapillary Tumors Is Oncologic Safe
- Use of caudal pancreatectomy as a novel adjunct procedure to proximal splenorenal shunt in patients with noncirrhotic portal hypertension: A retrospective cohort study
- Spleen-Preserving Distal Pancreatectomy for Blunt Pancreatic Trauma in a Pediatric Patient
- Unconventional shunt surgery for non-cirrhotic portal hypertension in patients not suitable for proximal splenorenal shunt
- Laparoscopic Spleen Preserving Distal Pancreatectomy with the Conservation of the Splenic Artery and the Vein