Ann Hepatobiliary Pancreat Surg.
2022 May;26(2):178-183. 10.14701/ahbps.21-106.
Use of caudal pancreatectomy as a novel adjunct procedure to proximal splenorenal shunt in patients with noncirrhotic portal hypertension: A retrospective cohort study
- Affiliations
-
- 1Department of Surgical Gastroenterology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
- KMID: 2530097
- DOI: http://doi.org/10.14701/ahbps.21-106
Abstract
- Backgrounds/Aims
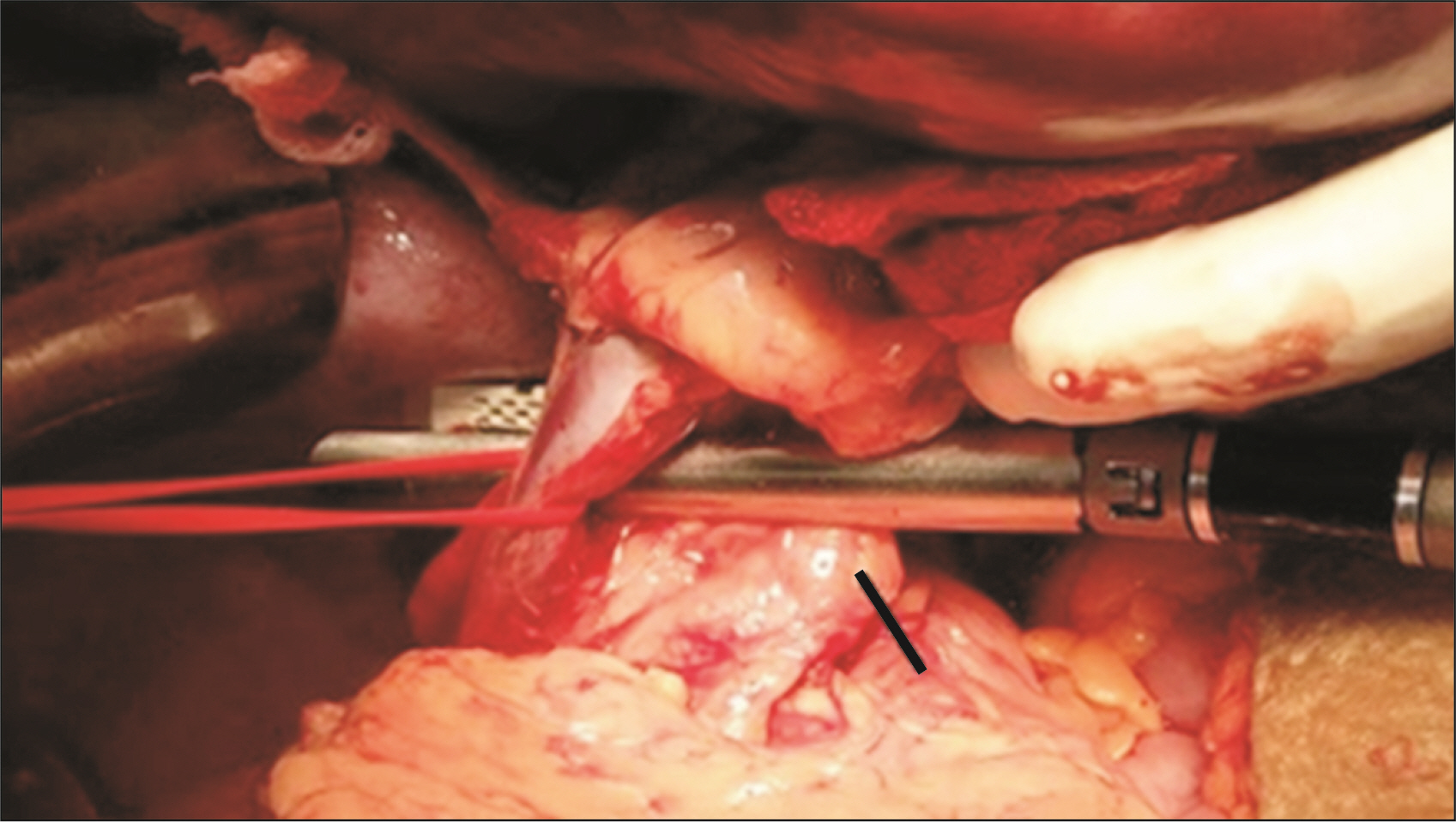
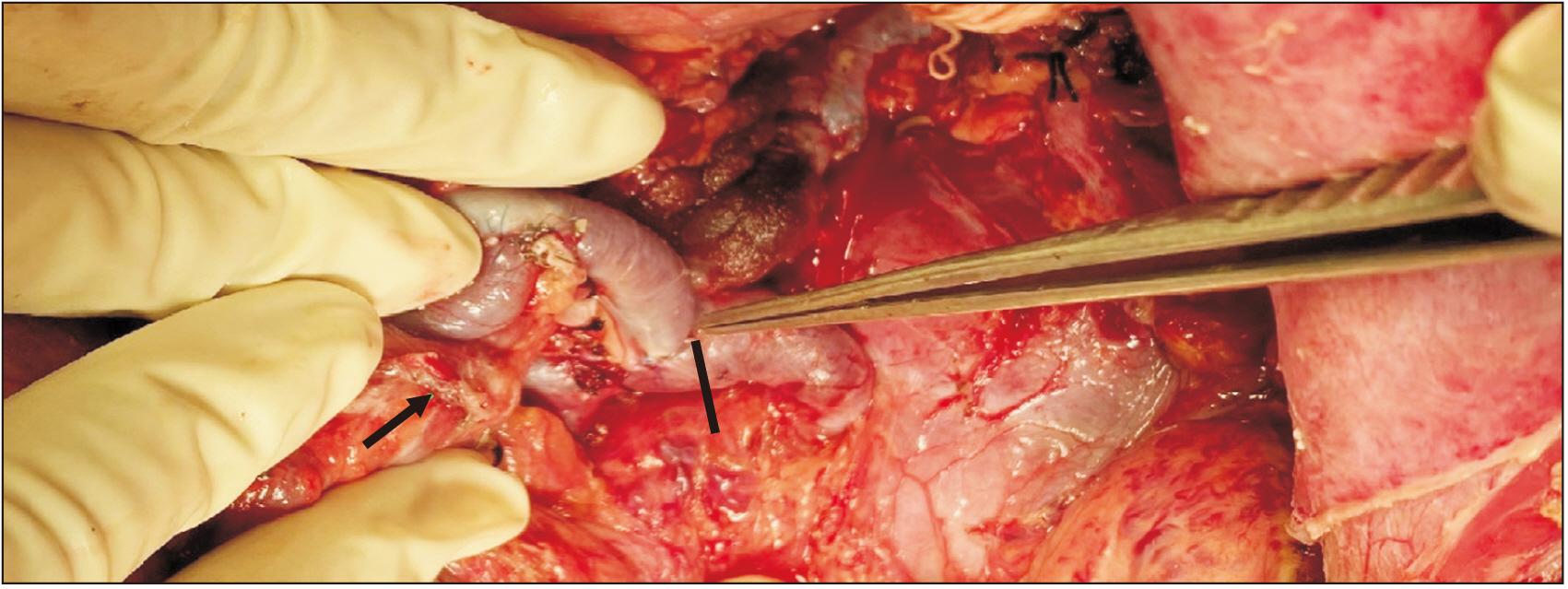
Proximal splenorenal shunt (PSRS) is considered a one-time treatment for noncirrhotic portal hypertension (NCPH) to prevent recurrent upper gastrointestinal (UGI) hemorrhage and long-term complications. Long-term shunt patency is necessary to achieve these. The lie of the shunt is a contributing factor to early shunt thrombosis. We investigated the role of resection of the distal tail of pancreas (caudal pancreatectomy [CP]) in improving the lie of shunt and decreasing shunt thrombosis.
Methods
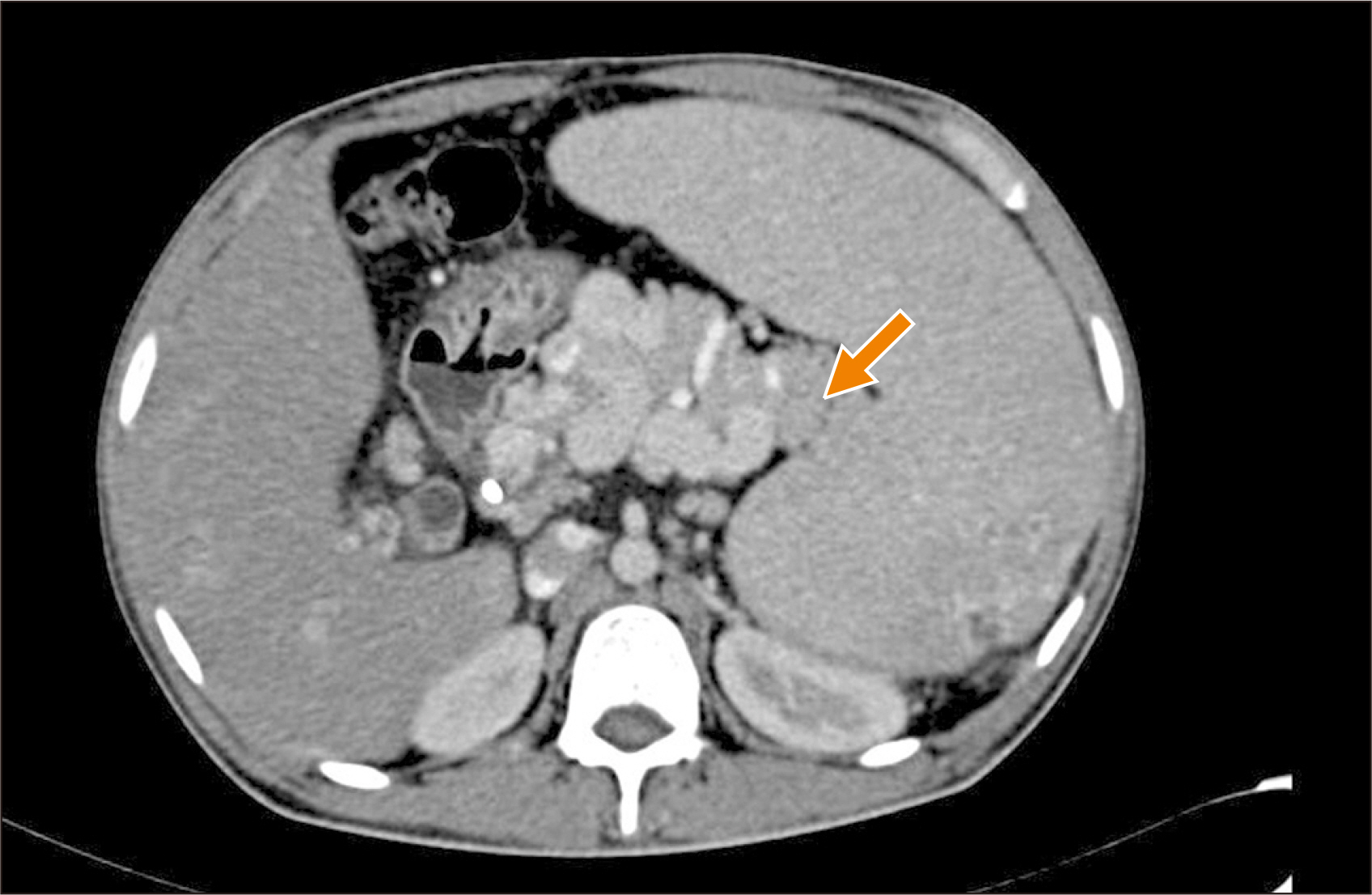
This was a retrospective cohort study of patients with NCPH who underwent PSRS between 2014–2020 in JIPMER, Puducherry, India. CP was performed in patients with a long tail of pancreas, with the tip of pancreatic tail extending up to splenic hilum on preoperative CT. Perioperative parameters and shunt patency rate of patients who underwent PSRS with CP (Group A) were compared with patients undergoing conventional PSRS (Group B). Statistical analysis was performed using the Mann–Whitney U test and χ 2 test.
Results
Eighty four patients with NCPH underwent PSRS (extrahepatic portal vein obstruction = 39; noncirrhotic portal fibrosis = 45). Blood loss was lower (p = 0.002) and post-shunt fall in portal pressure higher (p = 0.002) in Group A. Shunt thrombosis rate was lower (p = 0.04) while rate of complete variceal regression (p = 0.03) and biochemical pancreatic leak (p = 0.01) were higher in Group A.There was no clinically relevant pancreatic fistula in either group.
Conclusions
CP is a safe and useful technique for reducing shunt thrombosis after PSRS in patients with NCPH by improving the lie of shunt.
Keyword
Figure
Cited by 1 articles
-
Surgical outcome of extrahepatic portal venous obstruction: Audit from a tertiary referral centre in Eastern India
Somak Das, Tuhin Subhra Manadal, Suman Das, Jayanta Biswas, Arunesh Gupta, Sreecheta Mukherjee, Sukanta Ray
Ann Hepatobiliary Pancreat Surg. 2023;27(4):350-365. doi: 10.14701/ahbps.23-025.
Reference
-
1. Pal S, Sahni P. 2009; Extrahepatic portal venous obstruction: is the knife irrelevant? Indian J Gastroenterol. 28:198–200. DOI: 10.1007/s12664-009-0078-0. PMID: 20177866.
Article2. Prasad AS, Gupta S, Kohli V, Pande GK, Sahni P, Nundy S. 1994; Proximal splenorenal shunts for extrahepatic portal venous obstruction in children. Ann Surg. 219:193–196. DOI: 10.1097/00000658-199402000-00011. PMID: 8129490. PMCID: PMC1243121.
Article3. Mishra PK, Patil NS, Saluja S, Narang P, Solanki N, Varshney V. 2016; High patency of proximal splenorenal shunt: a myth or reality? - A prospective cohort study. Int J Surg. 27:82–87. DOI: 10.1016/j.ijsu.2015.12.071. PMID: 26804351.
Article4. Gupta S, Venkata Srinivas G, Chandrasekar AS, Kalayarasan R, Pottakkat B. 2019; Splenoadrenal shunt for noncirrhotic portal hypertension. Indian J Surg. 81:28–31. DOI: 10.1007/s12262-017-1706-z.
Article5. Gupta S, Pottakkat B, Verma SK, Kalayarasan R, Chandrasekar AS, Pillai AA. 2020; Pathological abnormalities in splenic vasculature in non-cirrhotic portal hypertension: its relevance in the management of portal hypertension. World J Gastrointest Surg. 12:1–8. DOI: 10.4240/wjgs.v12.i1.1. PMID: 31984119. PMCID: PMC6943091.
Article6. George J, Panwar R, Saluja SS, Sahni P. Mishra PK, editor. 2016. Surgery for portal hypertension. Textbook of surgical gastroenterology. Vol 2:Jaypee Brothers Medical Publishers;New Delhi: p. 1357–1366. DOI: 10.5005/jp/books/12748_125.7. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.
Article8. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.9. Dutta HK, Baruah M. 2015; Management of extrahepatic portal vein obstruction in children: experience in a tertiary care center in Northeast India. J Med Soc. 29:101–105. DOI: 10.4103/0972-4958.163200.
Article10. Bismuth H, Franco D, Alagille D. 1980; Portal diversion for portal hypertension in children. The first ninety patients. Ann Surg. 192:18–24. DOI: 10.1097/00000658-198007000-00003. PMID: 7406558. PMCID: PMC1344799.
Article11. Orloff MJ, Orloff MS, Girard B, Orloff SL. 2002; Bleeding esophagogastric varices from extrahepatic portal hypertension: 40 years' experience with portal-systemic shunt. J Am Coll Surg. 194:717–728. DOI: 10.1016/S1072-7515(02)01170-5. PMID: 12081062.
Article12. Rao KL, Goyal A, Menon P, Thapa BR, Narasimhan KL, Chowdhary SK, et al. 2004; Extrahepatic portal hypertension in children: observations on three surgical procedures. Pediatr Surg Int. 20:679–684. DOI: 10.1007/s00383-004-1272-x. PMID: 15351894.
Article13. Wani AH, Shah OJ, Zargar SA. 2011; Management of variceal hemorrhage in children with extrahepatic portal venous obstruction-shunt surgery versus endoscopic sclerotherapy. Indian J Surg. 73:409–413. DOI: 10.1007/s12262-011-0345-z. PMID: 23204696. PMCID: PMC3236262.
Article14. Sharma N, Bajpai M, Kumar A, Paul S, Jana M. 2014; Portal hypertension: a critical appraisal of shunt procedures with emphasis on distal splenorenal shunt in children. J Indian Assoc Pediatr Surg. 19:80–84. DOI: 10.4103/0971-9261.129599. PMID: 24741210. PMCID: PMC3983772.
Article15. Shah OJ, Robbani I. 2005; A simplified technique of performing splenorenal shunt (Omar's technique). Tex Heart Inst J. 32:549–554. PMID: 16429901. PMCID: PMC1351828.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Distal pancreatectomy with splenorenal shunt to preserve spleen in a cirrhotic patient
- Epidural Analgesia in a Parturient following Splenorenal Shunt Operation for Liver Cirrhosis
- Unconventional shunt surgery for non-cirrhotic portal hypertension in patients not suitable for proximal splenorenal shunt
- Analysis of a Distal Splenorenal Shunt for Treatment of Variceal Bleeding
- Living donor liver transplantation with proximal splenic vein ligation in a pediatric patient with congenital absence of the portal vein