Cancer Res Treat.
2017 Apr;49(2):548-552. 10.4143/crt.2016.110.
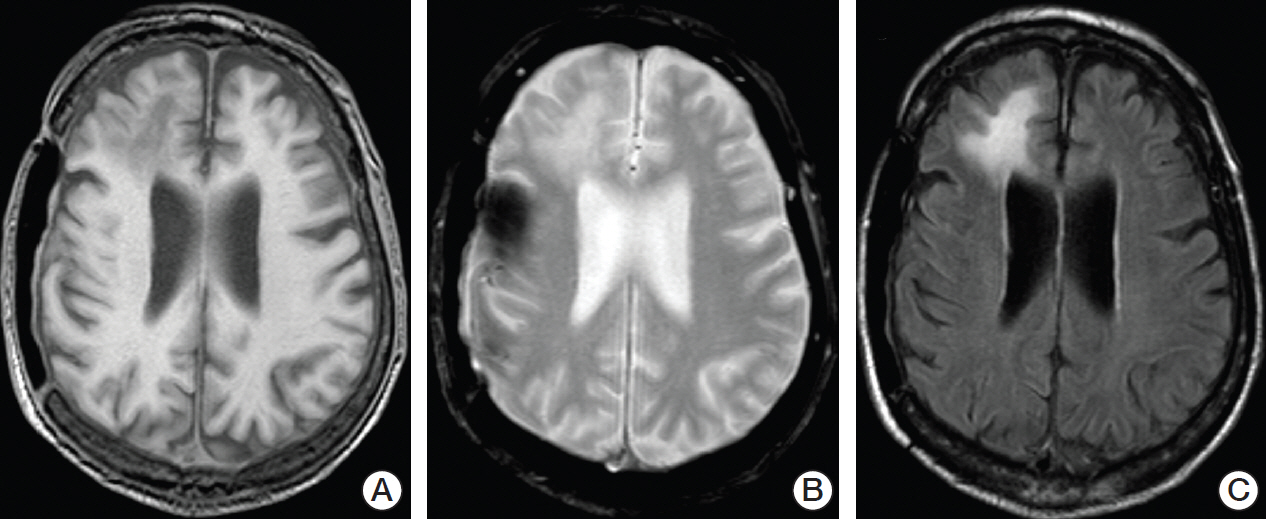
Progressive Multifocal Leukoencephalopathy after Ibrutinib Therapy for Chronic Lymphocytic Leukemia
- Affiliations
-
- 1Department of Medicine A, University Hospital of Münster, Münster, Germany. mathias.lutz@ukmuenster.de
- 2Department of Internal Medicine, Marienhospital Osnabrück, Osnabrück, Germany.
- 3Department of Clinical Radiology, University Hospital of Münster, Münster, Germany.
- 4Department of Neurology, University Hospital of Münster, Münster, Germany.
- 5Department of Translational Oncology, University Hospital of Münster, Münster, Germany.
- 6Cluster of Excellence EXC 1003, Cells in Motion, Münster, Germany.
- KMID: 2378128
- DOI: http://doi.org/10.4143/crt.2016.110
Abstract
- Progressive multifocal leukoencephalopathy (PML) is a devastating neurological disease observed nearly exclusively in immunocompromised patients. Recently, the introduction of monoclonal antibodies significantly inhibiting the immune system such as rituximab has led to an increase in PML cases. Although rituximab-based immunochemotherapy remains the standard of treatment for chronic lymphocytic leukemia (CLL), the importance of Bruton's tyrosine kinase inhibitors such as ibrutinib is steadily increasing. However, long-term experiences regarding possible side effects of these new substances are rare. Here, we report the development of eventually fatal PML possibly associated with ibrutinib therapy for CLL after multiple prior treatment lines, including rituximab. To the best of our knowledge, this is the first study to report such findings. Since the last course of rituximab was applied over 3 years ago, it is conceivable that the strong B cell inhibition by ibrutinib led to PML. With increased awareness of this potential side effect, further clinical studies are certainly warranted to evaluate this possible association.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Ferenczy MW, Marshall LJ, Nelson CD, Atwood WJ, Nath A, Khalili K, et al. Molecular biology, epidemiology, and pathogenesis of progressive multifocal leukoencephalopathy, the JC virus-induced demyelinating disease of the human brain. Clin Microbiol Rev. 2012; 25:471–506.
Article2. Honce JM, Nagae L, Nyberg E. Neuroimaging of natalizumab complications in multiple sclerosis: PML and other associated entities. Mult Scler Int. 2015; 2015:809252.
Article3. Astrom KE, Mancall EL, Richardson EP Jr. Progressive multifocal leuko-encephalopathy: a hitherto unrecognized complication of chronic lymphatic leukaemia and Hodgkin's disease. Brain. 1958; 81:93–111.4. Tavazzi E, Ferrante P, Khalili K. Progressive multifocal leukoencephalopathy: an unexpected complication of modern therapeutic monoclonal antibody therapies. Clin Microbiol Infect. 2011; 17:1776–80.
Article5. Bloomgren G, Richman S, Hotermans C, Subramanyam M, Goelz S, Natarajan A, et al. Risk of natalizumab-associated progressive multifocal leukoencephalopathy. N Engl J Med. 2012; 366:1870–80.
Article6. Carson KR, Evens AM, Richey EA, Habermann TM, Focosi D, Seymour JF, et al. Progressive multifocal leukoencephalopathy after rituximab therapy in HIV-negative patients: a report of 57 cases from the Research on Adverse Drug Events and Reports project. Blood. 2009; 113:4834–40.
Article7. Novero A, Ravella PM, Chen Y, Dous G, Liu D. Ibrutinib for B cell malignancies. Exp Hematol Oncol. 2014; 3:4.
Article8. Tucker DL, Rule SA. A critical appraisal of ibrutinib in the treatment of mantle cell lymphoma and chronic lymphocytic leukemia. Ther Clin Risk Manag. 2015; 11:979–90.9. Epperla N, Medina-Flores R, Mazza JJ, Yale SH. Mirtazapine and mefloquine therapy for non-AIDS-related progressive multifocal leukoencephalopathy. WMJ. 2014; 113:242–5.10. Hall CD, Dafni U, Simpson D, Clifford D, Wetherill PE, Cohen B, et al. Failure of cytarabine in progressive multifocal leukoencephalopathy associated with human immunodeficiency virus infection. AIDS Clinical Trials Group 243 Team. N Engl J Med. 1998; 338:1345–51.11. Marra CM, Rajicic N, Barker DE, Cohen BA, Clifford D, Donovan Post MJ, et al. A pilot study of cidofovir for progressive multifocal leukoencephalopathy in AIDS. AIDS. 2002; 16:1791–7.
Article12. Clifford DB, Nath A, Cinque P, Brew BJ, Zivadinov R, Gorelik L, et al. A study of mefloquine treatment for progressive multifocal leukoencephalopathy: results and exploration of predictors of PML outcomes. J Neurovirol. 2013; 19:351–8.
Article13. Giacomini PS, Rozenberg A, Metz I, Araujo D, Arbour N, Bar-Or A, et al. Maraviroc and JC virus-associated immune reconstitution inflammatory syndrome. N Engl J Med. 2014; 370:486–8.
Article14. Lane MA, Renga V, Pachner AR, Cohen JA. Late occurrence of PML in a patient treated for lymphoma with immunomodulatory chemotherapies, bendamustine, rituximab, and ibritumomab tiuxetan. Case Rep Neurol Med. 2015; 2015:892047.
Article15. Lejniece S, Murovska M, Chapenko S, Breiksa B, Jaunmuktane Z, Feldmane L, et al. Progressive multifocal leukoencephalopathy following fludarabine treatment in a chronic lymphocytic leukemia patient. Exp Oncol. 2011; 33:239–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrent Complex Partial Seizures in a Patient with Progressive Multifocal Leukoencephalopathy
- Hypointense Rim on Susceptibility-Weighted Imaging in a Patient with Progressive Multifocal Leukoencephalopathy
- Safety and efficacy analysis of ibrutinib in 32 patients with CLL and various B-cell lymphomas: real-world data from a single-center study in Turkey
- Progressive Multifocal Leukoencephalopathy Presenting as Viral Encephalitis in a Healthy Adult
- Progressive Multifocal Leukoencephalopathy in a Patient with T Cell Lymphoma of Head and Neck: A Case Report