J Korean Soc Radiol.
2017 May;76(5):358-362. 10.3348/jksr.2017.76.5.358.
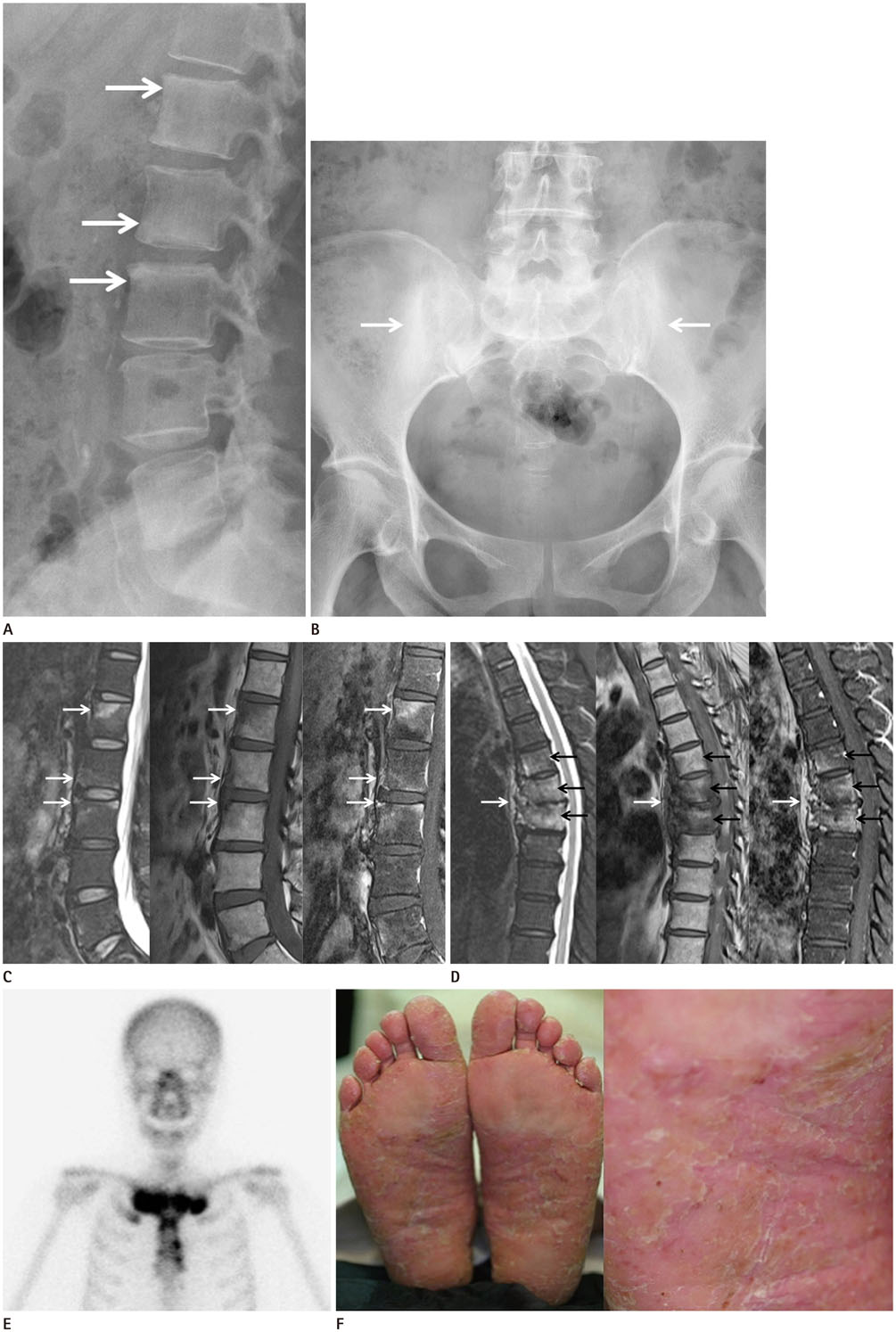
Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis Syndrome: A Case of Spine, Pelvis, and Anterior Chest Wall Involvement, with Overlooked Plantar Pustulosis
- Affiliations
-
- 1Department of Radiology, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. jmpark@catholic.ac.kr
- 2Department of Internal Medicine, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2377040
- DOI: http://doi.org/10.3348/jksr.2017.76.5.358
Abstract
- Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome is an inflammatory clinical condition with aseptic bone lesions and characteristic skin manifestations. A 63-year-old woman presented with vague musculoskeletal symptoms including chronic buttock pain. The clinical work-up revealed multiple spine and osteoarticular involvement. Multilevel bone marrow edema and cortical erosions involving the spine, asymmetric sacroiliitis, and osteosclerosis of the sternoclavicular joint were consistent with a diagnosis of SAPHO syndrome. Considering SAPHO syndrome in the differential diagnosis, subsequent skin inspection revealed plantar pustulosis. Despite the unique feature of accompanying skin and skeletal lesions, skin lesions could be overlooked if not suspected.
MeSH Terms
-
Acne Vulgaris*
Acquired Hyperostosis Syndrome
Bone Marrow
Buttocks
Diagnosis
Diagnosis, Differential
Edema
Female
Humans
Hyperostosis*
Magnetic Resonance Imaging
Middle Aged
Osteitis*
Osteosclerosis
Pelvis*
Sacroiliitis
Skin
Skin Manifestations
Spine*
Spiral Cone-Beam Computed Tomography
Sternoclavicular Joint
Synovitis*
Thoracic Wall*
Thorax*
Figure
Reference
-
1. Benhamou CL, Chamot AM, Kahn MF. Synovitis-acne-pustulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol. 1988; 6:109–112.2. Windom RE, Sanford JP, Ziff M. Acne conglobata and arthritis. Arthritis Rheum. 1961; 4:632–635.3. Depasquale R, Kumar N, Lalam RK, Tins BJ, Tyrrell PN, Singh J, et al. SAPHO: what radiologists should know. Clin Radiol. 2012; 67:195–206.4. Magrey M, Khan MA. New insights into synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome. Curr Rheumatol Rep. 2009; 11:329–333.5. Van Doornum S, Barraclough D, McColl G, Wicks I. SAPHO: rare or just not recognized? Semin Arthritis Rheum. 2000; 30:70–77.6. Colina M, Govoni M, Orzincolo C, Trotta F. Clinical and radiologic evolution of synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome: a single center study of a cohort of 71 subjects. Arthritis Rheum. 2009; 61:813–821.7. Boutin RD, Resnick D. The SAPHO syndrome: an evolving concept for unifying several idiopathic disorders of bone and skin. AJR Am J Roentgenol. 1998; 170:585–591.8. Earwaker JW, Cotten A. SAPHO: syndrome or concept? Imaging findings. Skeletal Radiol. 2003; 32:311–327.9. Hayem G, Bouchaud-Chabot A, Benali K, Roux S, Palazzo E, Silbermann-Hoffman O, et al. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum. 1999; 29:159–171.10. Fu Z, Liu M, Li Z, Fan Y, Zhang J, Zhang X, et al. Is the bullhead sign on bone scintigraphy really common in the patient with SAPHO syndrome? A single-center study of a 16-year experience. Nucl Med Commun. 2016; 37:387–392.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of SAPHO Syndrome
- A Case of Palmoplantar Pustulosis Present in the Daughter of a SAPHO Syndrome Patient
- A Case of SAPHO Syndrome with Hyperostosis of the Ulna
- SAPHO (Synovitis, Acne, Pustulosis, Hyperostosis, Osteitis) Syndrome occurred on the Clavicle: A Case Report
- Infliximab for Treatment of Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis Syndrome: A Case Report