J Korean Soc Transplant.
2017 Mar;31(1):16-24. 10.4285/jkstn.2017.31.1.16.
Kidney Transplantation from Expanded Criteria Donor in Korea: It's Time to Have Our Own Criteria Based on Our Experiences
- Affiliations
-
- 1Division of Transplantation and Vascular Surgery, Yeungnam University Medical Center, Yeungnam University School of Medicine, Daegu, Korea.
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jbparkmd@gmail.com
- KMID: 2375676
- DOI: http://doi.org/10.4285/jkstn.2017.31.1.16
Abstract
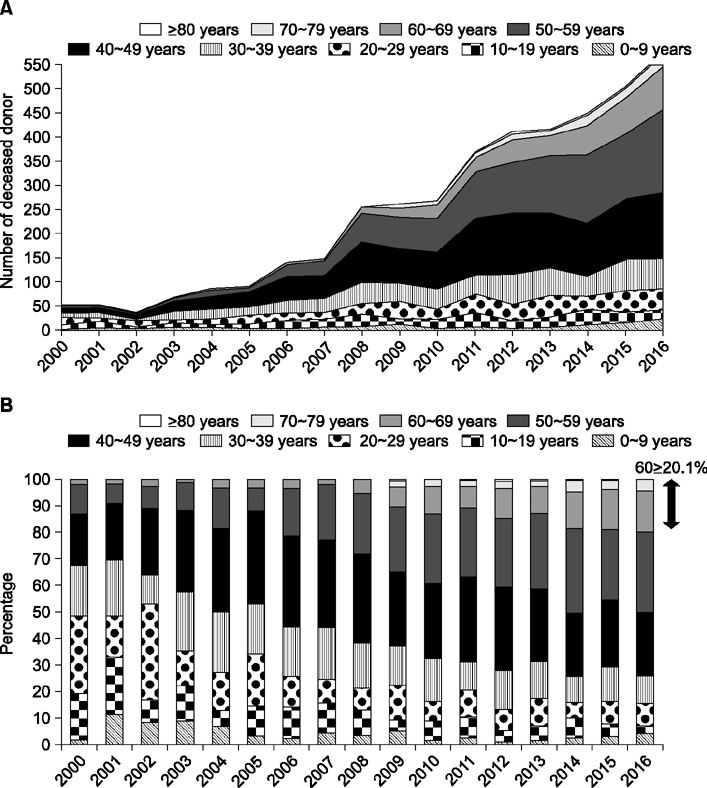
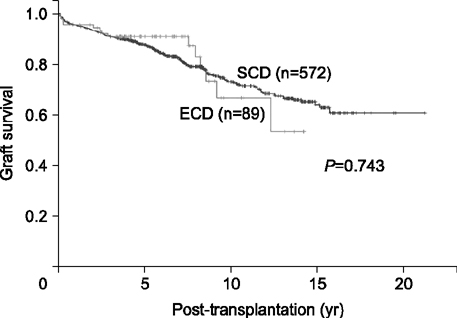
- The disparity between the number of patients awaiting kidney transplantation (KT) on the list and the number of actual number of KT from deceased organ donation has become wider despite the recent increase in the number of donations. Moreover, the proportion of donors aged 60 or more has rapidly increased. KT from expanded criteria donor (ECD) has been not only been necessary, but also inevitable with respect to maximizing the use of this scarce organ resource. However, we still use the "marginal donor criteria" implemented in 2000 when KONOS (Korean Network for Organ Sharing) was established. In the Korean transplantation environment, this "marginal donor criteria" does not have the power to predict graft outcome, and fails to discern grafts with inferior transplant outcomes from successful transplants. As a result, it does not meet the role of the criteria in Korea. Therefore, we should develop our own criteria based on our deceased donor kidney transplantation experience. Here, we review the current status of ECD KT in Korea in context with the progression of the ECD criteria system in UNOS (United Network for Organ Sharing) and present some considerations for the Korean donor criteria system.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical outcomes of the first 300 cases of kidney transplantation: a single-center retrospective cohort study
Hyoung Won Koh, Kyunglim Koo, Chang Sik Shin, Hyung Sub Park, Jong Cheol Jeong, Sejoong Kim, Dong Wan Chae, Jong Jin Oh, Seok-Soo Byun, Taeseung Lee
Korean J Transplant. 2020;34(3):154-166. doi: 10.1371/journal.pone.0208638.
Reference
-
1. Kwak JY, Park CD, Lee KS, Won CK, Kang CM, Park HC, et al. An analysis of 15 cases of cadaveric kidney transplantation. J Korean Soc Transplant. 1993; 7:119–127.2. Korean Network for Organ Sharing (KONOS). 2016 Quarterly Data [Internet]. Seoul: KONOS;2016. cited 2017 Jan 20. Available from: https://www.konos.go.kr/konosis/common/bizlogic.jsp.3. Min SI, Kim SY, Park YJ, Min SK, Kim YS, Ahn C, et al. Trends in deceased organ donation and utilization in Korea: 2000-2009. J Korean Med Sci. 2010; 25:1122–1127.
Article4. ESRD registry committee, Korean Society of Nephrology. Current renal replacement therapy in Korea [Internet]. Seoul: Korean Society of Nephrology;2016. cited 2017 20 Jan. Available from: http://www.ksn.or.kr/rang_board/list.html?code=sinchart.5. Lee SH, Huh KH, Lee HS, Kim HJ, Kim MS, Joo DJ, et al. Waiting time for deceased donor kidney allocation in Korea: A single center experience. J Korean Soc Transplant. 2012; 26:32–37.
Article6. Ojo AO, Hanson JA, Meier-Kriesche H, Okechukwu CN, Wolfe RA, Leichtman AB, et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-listed transplant candidates. J Am Soc Nephrol. 2001; 12:589–597.
Article7. Ministry of Health & Welfare. Korean Network for Oran Sharing. 2016 Business guide on organ transplant management [Internet]. Sejong: Seoul: Ministry of Health & Welfare;Korean Network for Oran Sharing;2016. cited 2017 Jan 20. Available from: https://www.konos.go.kr/konosis/index.jsp.8. Port FK, Bragg-Gresham JL, Metzger RA, Dykstra DM, Gillespie BW, Young EW, et al. Donor characteristics associated with reduced graft survival: an approach to expanding the pool of kidney donors. Transplantation. 2002; 74:1281–1286.
Article9. Merion RM, Ashby VB, Wolfe RA, Distant DA, Hulbert-Shearon TE, Metzger RA, et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA. 2005; 294:2726–2733.
Article10. A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA. 1968; 205:337–340.11. Sanchez-Fructuoso AI, Prats D, Torrente J, Perez-Contin MJ, Fernandez C, Alvarez J, et al. Renal transplantation from non-heart beating donors: a promising alternative to enlarge the donor pool. J Am Soc Nephrol. 2000; 11:350–358.12. Doshi MD, Hunsicker LG. Short- and long-term outcomes with the use of kidneys and livers donated after cardiac death. Am J Transplant. 2007; 7:122–129.
Article13. Locke JE, Segev DL, Warren DS, Dominici F, Simpkins CE, Montgomery RA. Outcomes of kidneys from donors after cardiac death: implications for allocation and preservation. Am J Transplant. 2007; 7:1797–1807.
Article14. Rao PS, Schaubel DE, Guidinger MK, Andreoni KA, Wolfe RA, Merion RM, et al. A comprehensive risk quantification score for deceased donor kidneys: the kidney donor risk index. Transplantation. 2009; 88:231–236.
Article15. Remuzzi G, Grinyo J, Ruggenenti P, Beatini M, Cole EH, Milford EL, et al. Early experience with dual kidney transplantation in adults using expanded donor criteria. Double Kidney Transplant Group (DKG). J Am Soc Nephrol. 1999; 10:2591–2598.
Article16. Pokorna E, Vitko S, Chadimova M, Schuck O, Ekberg H. Proportion of glomerulosclerosis in procurement wedge renal biopsy cannot alone discriminate for acceptance of marginal donors. Transplantation. 2000; 69:36–43.
Article17. Edwards EB, Posner MP, Maluf DG, Kauffman HM. Reasons for non-use of recovered kidneys: the effect of donor glomerulosclerosis and creatinine clearance on graft survival. Transplantation. 2004; 77:1411–1415.
Article18. Sung RS, Christensen LL, Leichtman AB, Greenstein SM, Distant DA, Wynn JJ, et al. Determinants of discard of expanded criteria donor kidneys: impact of biopsy and machine perfusion. Am J Transplant. 2008; 8:783–792.
Article19. HRSA/OPTN. OPTN Policies [Internet]. Richmond, Virginia: Organ Procurement and Transplantation Network;c2015. cited 2017 Jan 20. Available from: https://optn.transplant.hrsa.gov/governance/policies.20. Klair T, Gregg A, Phair J, Kayler LK. Outcomes of adult dual kidney transplants by KDRI in the United States. Am J Transplant. 2013; 13:2433–2440.
Article21. Park UJ, Cho WH, Kim HT, Kim MY, Kim YL, Kim CD, et al. Evaluation of the Korean Network for Organ Sharing expanded donor criteria in deceased donor renal transplantation. J Korean Soc Transplant. 2013; 27:166–173.
Article22. Yang SS, Yang J, Ahn C, Min SI, Ha J, Kim SJ, et al. The need for new donor stratification to predict graft survival in deceased donor kidney transplantation. Yonsei Med J. 2017; 58:626–630.
Article23. Park UJ, Kim MY, Kim HT, Cho WH. Validation of the KDRI in Korean Deceased Donor Kidney Transplantation. J Korean Soc Transplant. 2014; 28:78–82.
Article24. Han M, Jeong JC, Koo TY, Jeon HJ, Kwon HY, Kim YJ, et al. Kidney donor risk index is a good prognostic tool for graft outcomes in deceased donor kidney transplantation with short, cold ischemic time. Clin Transplant. 2014; 28:337–344.
Article25. Hur N, Park H, Lee K, Choi G, Kim JM, Park JB, et al. The long-term outcomes of kidney transplantation from donation after circulatory death during brain death donor evaluation in a single center in Korea. J Korean Soc Transplant. 2015; 29:216–226.
Article26. Yang J, Lee J, Huh KH, Park JB, Cho JH, Lee S, et al. KNOW-KT (KoreaN cohort study for outcome in patients with kidney transplantation: a 9-year longitudinal cohort study): study rationale and methodology. BMC Nephrol. 2014; 15:77.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation and Utilization of Expanded Criteria Dornor
- A Preliminary Study to Revise the Marginal Donor Criteria of KONOS in Deceased Donor Kidney Transplantation
- Primary non-function in a deceased donor kidney transplant even with a Kidney Donor Risk Index less than 1.0: a case report
- Impact of preoperative ultrasonography for predicting the prognosis of deceased donor kidney transplantation
- Validation of the KDRI in Korean Deceased Donor Kidney Transplantation