Blood Res.
2017 Mar;52(1):31-36. 10.5045/br.2017.52.1.31.
Physicians' preferences and perceptions regarding donor selection in allogeneic stem cell transplantation in Korea when a matched domestic donor is not available
- Affiliations
-
- 1National Evidence-based Healthcare Collaborating Agency, Seoul, Korea. go01@snu.ac.kr
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- KMID: 2375201
- DOI: http://doi.org/10.5045/br.2017.52.1.31
Abstract
- BACKGROUND
A number of alternative donor options exist for patients who fail to find domestic HLA-matched donors for allogeneic hematopoietic stem cell transplantation (allo-HSCT). We assessed physicians' perspectives on allo-HSCT donor selection when a matched domestic donor is not available.
METHODS
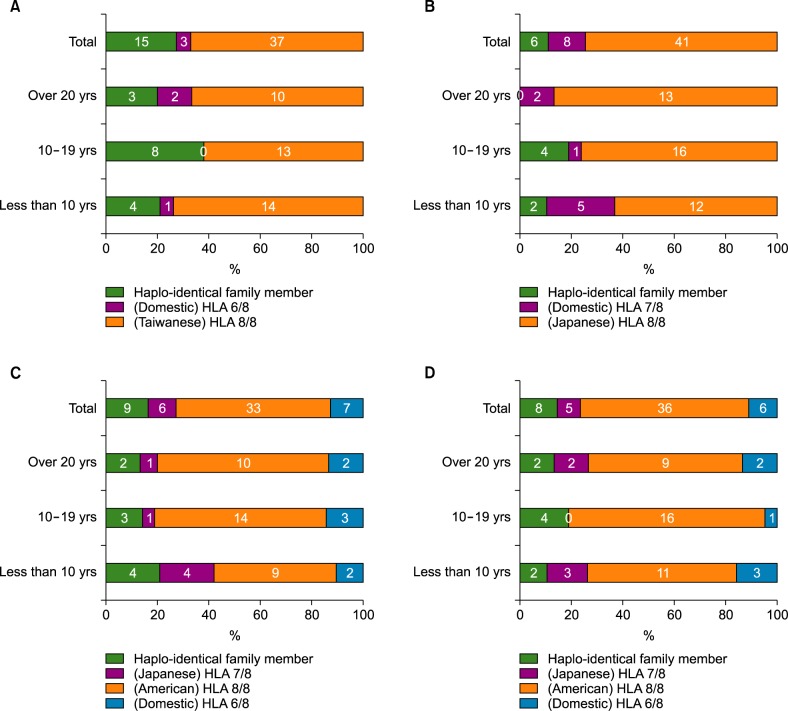
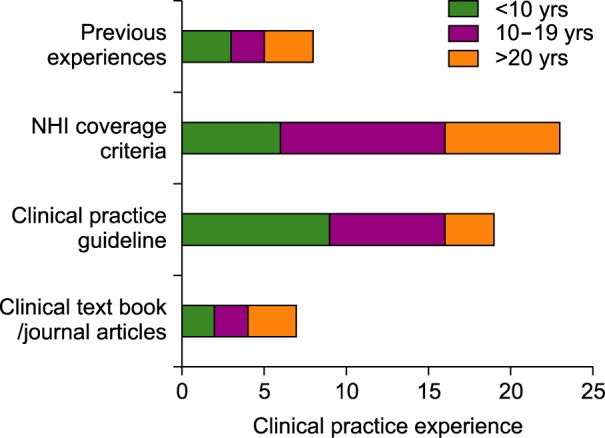
We administered a questionnaire survey to 55 hematologists (response rate: 28%) who attended the annual spring conference of the Korean Society of Haematology in 2015. The questionnaire contained four clinical allo-HSCT scenarios and the respondents were asked to choose the most preferred donor among the given options.
RESULTS
In all four scenarios, the hematologists preferred a matched international donor over partially mismatched unrelated domestic or haplo-matched family donors. The numbers of hematologists who chose a matched international donor (HLA 8/8) in cases of acute myeloid leukemia, chronic myeloid leukemia, acute lymphoblastic leukemia, and aplastic anemia were 37 (67.3%), 41 (74.6%), 33 (60.0%), and 36 (65.5%), respectively. The important factors that affected donor selection included "expecting better clinical outcomes (40.5%)" and "lower risk of side effects (23.4%)." The majority of participants (80%) responded that allo-HSCT guidelines for donor selection customized for the Korean setting are necessary.
CONCLUSION
Although hematologists still prefer perfectly matched foreign donors when a fully matched domestic allo-HSCT donor is not available, we confirmed that there was variation in their responses. For evidence-based clinical practice, it is necessary to provide further comparative clinical evidence on allo-HSCT from haplo-matched family donors and fully matched unrelated international donors.
MeSH Terms
Figure
Reference
-
1. Krishnamurti L, Abel S, Maiers M, Flesch S. Availability of unrelated donors for hematopoietic stem cell transplantation for hemoglobinopathies. Bone Marrow Transplant. 2003; 31:547–550. PMID: 12692619.
Article2. Parmar S, de Lima M. Hematopoietic stem cell transplantation for myelodysplastic syndrome. Biol Blood Marrow Transplant. 2010; 16(Suppl 1):S37–S44. PMID: 19857589.
Article3. Armand P, Antin JH. Allogeneic stem cell transplantation for aplastic anemia. Biol Blood Marrow Transplant. 2007; 13:505–516. PMID: 17448909.
Article4. Mahmoud HK, Elhaddad AM, Fahmy OA, et al. Allogeneic hematopoietic stem cell transplantation for non-malignant hematological disorders. J Adv Res. 2015; 6:449–458. PMID: 26257943.
Article5. Spitzer TR. Haploidentical stem cell transplantation: the always present but overlooked donor. Hematology Am Soc Hematol Educ Program. 2005; 2005:390–395.
Article6. Powles RL, Morgenstern GR, Kay HE, et al. Mismatched family donors for bone-marrow transplantation as treatment for acute leukaemia. Lancet. 1983; 1:612–615. PMID: 6131300.
Article7. Beatty PG, Clift RA, Mickelson EM, et al. Marrow transplantation from related donors other than HLA-identical siblings. N Engl J Med. 1985; 313:765–771. PMID: 3897863.
Article8. Velickovic ZM, Carter JM. Feasibility of finding an unrelated bone marrow donor on international registries for New Zealand patients. Bone Marrow Transplant. 1999; 23:291–294. PMID: 10084262.
Article9. Kanakry CG, Fuchs EJ, Luznik L. Modern approaches to HLA-haploidentical blood or marrow transplantation. Nat Rev Clin Oncol. 2016; 13:132. PMID: 26718103.
Article10. Wang Y, Liu QF, Xu LP, et al. Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood. 2015; 125:3956–3962. PMID: 25940714.
Article11. Lu DP, Dong L, Wu T, et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood. 2006; 107:3065–3073. PMID: 16380454.
Article12. Wang Y, Liu DH, Xu LP, et al. Superior graft-versus-leukemia effect associated with transplantation of haploidentical compared with HLA-identical sibling donor grafts for high-risk acute leukemia: an historic comparison. Biol Blood Marrow Transplant. 2011; 17:821–830. PMID: 20831895.
Article13. Koh Y, Shin S, Moon J, et al. Comparing outcome of unrelated allogeneic transplantation according to donor's nationality. Seoul, Korea: Natioanl Evidnece-based Healthcare Collaborating Agency;2016. Accessed July 5, 2016. at http://www.neca.re.kr/center/researcher/report_list.jsp?boardNo=GA.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful engraftment after infusion of multiple low doses of CD34+ cells from a poorly matched sibling donor in a patient with severe aplastic anemia
- Recent advances in haploidentical hematopoietic stem cell transplantation using ex vivo T cell-depleted graft in children and adolescents
- Donor Selection, Management, and Procurement for Lung Transplantation
- Optimal Selection of Cord Blood for Hematopoietic Stem Cell Transplantation
- Clinical Allogeneic and Autologous Islet Cell Transplantation: Update