Ann Surg Treat Res.
2017 Apr;92(4):208-213. 10.4174/astr.2017.92.4.208.
Combined spinal-epidural anesthesia in laparoscopic appendectomy: a prospective feasibility study
- Affiliations
-
- 1Department of Anesthesiology and Reanimation, Haseki Training and Research Hospital, Istanbul, Turkey. drsinanuzman@yahoo.com
- 2Department of General Surgery, Lutfiye Nuri Burat State Hospital, Istanbul, Turkey.
- 3Department of Anesthesiology and Reanimation, Lütfiye Nuri Burat State Hospital, Istanbul, Turkey.
- 4Department of General Surgery, Haseki Training and Research Hospital, Istanbul, Turkey.
- KMID: 2374686
- DOI: http://doi.org/10.4174/astr.2017.92.4.208
Abstract
- PURPOSE
Laparoscopic appendectomy (LA) is routinely performed under general, not regional anesthesia. This study assessed the feasibility, efficacy, and side effects of combined spinal-epidural anesthesia (CSEA) in LA.
METHODS
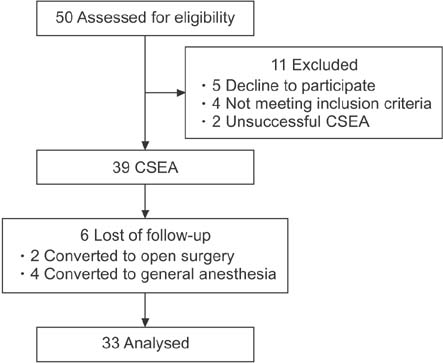
Thirty-three American Society of Anesthesiologist (ASA) physical status classification grade I patients underwent LA under CSEA. CSEA was performed using the needle-through-needle technique at the L₃-L₄ interspace. Preoperative and postoperative adverse events related to CSEA, patient satisfaction, and postoperative pain levels were recorded.
RESULTS
LA under CSEA was performed successfully in 33 patients (84.6%). Peroperatively, right shoulder pain was observed in 8 patients (24.1%), abdominal discomfort in 6 (18.2%), anxiety in 5 (15.2%), hypotension in 2 (6.1%) and nausea-vomiting in 1 (3%). In the first 24 hours after LA, headache, urinary retention, right shoulder pain, and postoperative nausea/vomiting (PONV) occurred in 18.1%, 12.1%, 9.1%, and 0% of patients, respectively. In the first 6 hours postoperation, no patients had operation-site pain that required analgesic treatment. Thirty-one patients (94%) evaluated their satisfaction with the procedure as good or moderate.
CONCLUSION
CSEA is an efficient and suitable anesthesia technique in LA for ASA physical status classification grade I healthy patients. CSEA is associated with good postoperative pain control and the absence of PONV and intubation-associated complications.
MeSH Terms
Figure
Reference
-
1. Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res. 2012; 175:185–190.2. Lee JH, Park YS, Choi JS. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J Epidemiol. 2010; 20:97–105.3. Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT, et al. Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide Inpatient Sample (NIS), 2006-2008. J Gastrointest Surg. 2011; 15:2226–2231.4. Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, et al. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004; 239:43–52.5. Minutolo V, Licciardello A, Di Stefano B, Arena M, Arena G, Antonacci V. Outcomes and cost analysis of laparoscopic versus open appendectomy for treatment of acute appendicitis: 4-years experience in a district hospital. BMC Surg. 2014; 14:14.6. Jaschinski T, Mosch C, Eikermann M, Neugebauer EA. Laparoscopic versus open appendectomy in patients with suspected appendicitis: a systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015; 15:48.7. Wittgen CM, Andrus CH, Fitzgerald SD, Baudendistel LJ, Dahms TE, Kaminski DL. Analysis of the hemodynamic and ventilatory effects of laparoscopic cholecystectomy. Arch Surg. 1991; 126:997–1000.8. Tzovaras G, Fafoulakis F, Pratsas K, Georgopoulou S, Stamatiou G, Hatzitheofilou C. Spinal vs general anesthesia for laparoscopic cholecystectomy: interim analysis of a controlled randomized trial. Arch Surg. 2008; 143:497–501.9. Tiwari S, Chauhan A, Chaterjee P, Alam MT. Laparoscopic cholecystectomy under spinal anaesthesia: a prospective, randomised study. J Minim Access Surg. 2013; 9:65–71.10. Lal P, Philips P, Saxena KN, Kajla RK, Chander J, Ramteke VK. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair under epidural anesthesia: a detailed evaluation. Surg Endosc. 2007; 21:595–601.11. Jun GW, Kim MS, Yang HJ, Sung TY, Park DH, Cho CK, et al. Laparoscopic appendectomy under spinal anesthesia with dexmedetomidine infusion. Korean J Anesthesiol. 2014; 67:246–251.12. Mane RS, Patil MC, Kedareshvara KS, Sanikop CS. Combined spinal epidural anesthesia for laparoscopic appendectomy in adults: a case series. Saudi J Anaesth. 2012; 6:27–30.13. Brull R, Macfarlane AJ, Chan WV. Spinal, epidural and caudal anesthesia. In : Miller RD, Cohen NH, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL, editors. Miller's Anesthesia. 8th ed. Philadelphia (PA): Elsevier Saunders;2015. p. 1684–1720.14. Hartmann B, Junger A, Klasen J, Benson M, Jost A, Banzhaf A, et al. The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection. Anesth Analg. 2002; 94:1521–1529.15. Gutt CN, Oniu T, Mehrabi A, Schemmer P, Kashfi A, Kraus T, et al. Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg. 2004; 21:95–105.16. Dexter SP, Vucevic M, Gibson J, McMahon MJ. Hemodynamic consequences of high- and low-pressure capnoperitoneum during laparoscopic cholecystectomy. Surg Endosc. 1999; 13:376–381.17. Cunningham AJ. Anesthetic implications of laparoscopic surgery. Yale J Biol Med. 1998; 71:551–578.18. Kazama T, Ikeda K, Kato T, Kikura M. Carbon dioxide output in laparoscopic cholecystectomy. Br J Anaesth. 1996; 76:530–535.19. Imbelloni LE. Spinal anesthesia for laparoscopic cholecystectomy: Thoracic vs. Lumbar Technique. Saudi J Anaesth. 2014; 8:477–483.20. Sinha R, Gurwara AK, Gupta SC. Laparoscopic surgery using spinal anesthesia. JSLS. 2008; 12:133–138.21. Jabbari A, Alijanpour E, Mir M, Bani Hashem N, Rabiea SM, Rupani MA. Post spinal puncture headache, an old problem and new concepts: review of articles about predisposing factors. Caspian J Intern Med. 2013; 4:595–602.22. Lee SJ, Lee JN. The effect of perioperative esmolol infusion on the postoperative nausea, vomiting and pain after laparoscopic appendectomy. Korean J Anesthesiol. 2010; 59:179–184.23. do Amaral PC, Filho Ede M, Galvao TD, Junior EE, de Magalhaes Neto GE, Mascarenhas F, et al. Factors leading to long-term hospitalization after laparoscopic appendectomy. JSLS. 2006; 10:355–358.24. Van Wijk RM, Watts RW, Ledowski T, Trochsler M, Moran JL, Arenas GW. Deep neuromuscular block reduces intra-abdominal pressure requirements during laparoscopic cholecystectomy: a prospective observational study. Acta Anaesthesiol Scand. 2015; 59:434–440.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic appendectomy under spinal anesthesia with dexmedetomidine infusion
- Laparoscopic cholecystectomy under epidural anesthesia: a clinical feasibility study
- Pneumocephalus Developed during Epidural Anesthesia for Combined Spinal-Epidural Anesthesia
- Motor Weakness on Lower Extremities after the Combined Spinal-epidural Anesthesia and Analgesia: A case report
- Effect of Loss of Epidural Negative Pressure on Spinal Sensory Blokade Level of Spinal Anesthesia