Yonsei Med J.
2016 Sep;57(5):1063-1069. 10.3349/ymj.2016.57.5.1063.
Dyspnea as a Prognostic Factor in Patients with Non-Small Cell Lung Cancer
- Affiliations
-
- 1Division of Pulmonary, Critical Care and Sleep Medicine, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. mdlee@catholic.ac.kr
- KMID: 2374149
- DOI: http://doi.org/10.3349/ymj.2016.57.5.1063
Abstract
- PURPOSE
To investigate associations between dyspnea and clinical outcomes in patients with non-small cell lung cancer (NSCLC).
MATERIALS AND METHODS
From 2001 to 2014, we retrospectively reviewed the prospective lung cancer database of St. Paul's Hospital at the Catholic University of Korea. We enrolled patients with NSCLC and evaluated symptoms of dyspnea using modified Medical Research Council (mMRC) scores. Also, we estimated pulmonary functions and analyzed survival data.
RESULTS
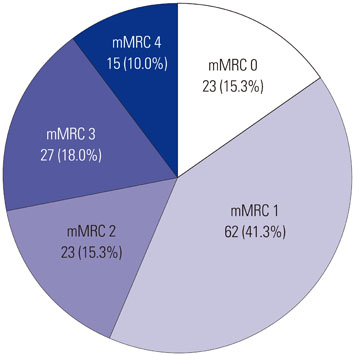
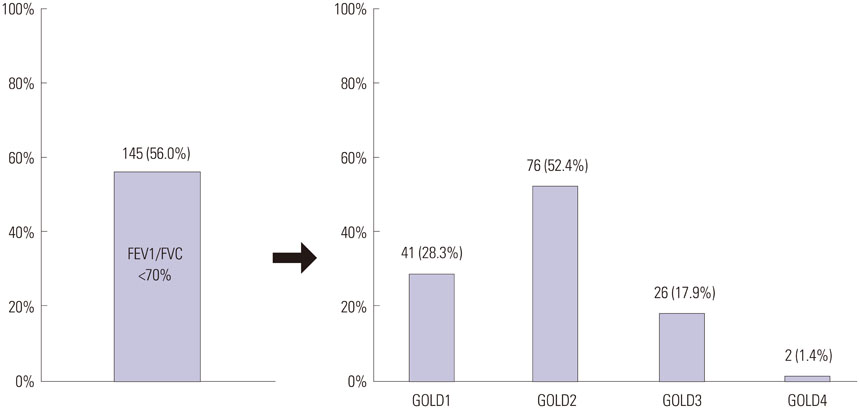
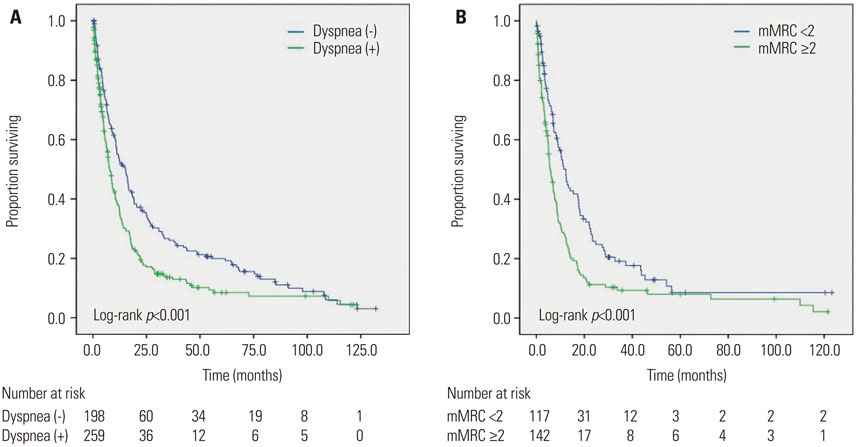
In total, 457 NSCLC patients were enrolled, and 259 (56.7%) had dyspnea. Among those with dyspnea and whose mMRC scores were available (109 patients had no mMRC score), 85 (56.6%) patients had an mMRC score <2, while 65 (43.3%) had an mMRC score ≥2. Significant decreased pulmonary functions were observed in patients with dyspnea. In multivariate analysis, aging, poor performance status, advanced stage, low forced expiratory volume in 1 second (%), and an mMRC score ≥2 were found to be significant prognostic factors for patient survival.
CONCLUSION
Dyspnea could be a significant prognostic factor in patients with NSCLC.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
Article2. Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013; 14:1165–1174.
Article3. National Lung Screening Trial Research Team. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395–409.
Article4. Walters S, Maringe C, Coleman MP, Peake MD, Butler J, Young N, et al. Lung cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK: a population-based study, 2004-2007. Thorax. 2013; 68:551–564.
Article5. Carlson LE, Waller A, Groff SL, Bultz BD. Screening for distress, the sixth vital sign, in lung cancer patients: effects on pain, fatigue, and common problems--secondary outcomes of a randomized controlled trial. Psychooncology. 2013; 22:1880–1888.
Article6. Blanchon F, Grivaux M, Asselain B, Lebas FX, Orlando JP, Piquet J, et al. 4-year mortality in patients with non-small-cell lung cancer: development and validation of a prognostic index. Lancet Oncol. 2006; 7:829–836.
Article7. Vermaelen K, Brusselle G. Exposing a deadly alliance: novel insights into the biological links between COPD and lung cancer. Pulm Pharmacol Ther. 2013; 26:544–554.
Article8. Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J. 2009; 34:380–386.
Article9. Sarna L, Evangelista L, Tashkin D, Padilla G, Holmes C, Brecht ML, et al. Impact of respiratory symptoms and pulmonary function on quality of life of long-term survivors of non-small cell lung cancer. Chest. 2004; 125:439–445.
Article10. Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the Functional Assessment of Cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer. 1995; 12:199–220.
Article11. Thongprasert S, Duffield E, Saijo N, Wu YL, Yang JC, Chu DT, et al. Health-related quality-of-life in a randomized phase III first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients from Asia with advanced NSCLC (IPASS). J Thorac Oncol. 2011; 6:1872–1880.
Article12. Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002; 121:1434–1440.
Article13. Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013; 187:347–365.
Article14. Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001; 27:85–96.15. Charpidou AG, Gkiozos I, Tsimpoukis S, Apostolaki D, Dilana KD, Karapanagiotou EM, et al. Therapy-induced toxicity of the lungs: an overview. Anticancer Res. 2009; 29:631–639.16. De Ruysscher D, Dehing C, Yu S, Wanders R, Ollers M, Dingemans AM, et al. Dyspnea evolution after high-dose radiotherapy in patients with non-small cell lung cancer. Radiother Oncol. 2009; 91:353–359.
Article17. Foroulis CN, Lioulias AG, Papakonstantinou C. Simple laboratory parameters which can determine the clinical state of patients after pneumonectomy for lung cancer. J Thorac Oncol. 2009; 4:55–61.
Article18. Feinstein MB, Krebs P, Coups EJ, Park BJ, Steingart RM, Burkhalter J, et al. Current dyspnea among long-term survivors of early-stage non-small cell lung cancer. J Thorac Oncol. 2010; 5:1221–1226.
Article19. Denehy L, Hornsby WE, Herndon JE 2nd, Thomas S, Ready NE, Granger CL, et al. Prognostic validation of the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index in inoperable non-small-cell lung cancer. J Thorac Oncol. 2013; 8:1545–1550.
Article20. Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004; 350:1005–1012.
Article21. Hashimoto N, Matsuzaki A, Okada Y, Imai N, Iwano S, Wakai K, et al. Clinical impact of prevalence and severity of COPD on the decision-making process for therapeutic management of lung cancer patients. BMC Pulm Med. 2014; 14:14.
Article22. Zhang J, Zhou JB, Lin XF, Wang Q, Bai CX, Hong QY. Prevalence of undiagnosed and undertreated chronic obstructive pulmonary disease in lung cancer population. Respirology. 2013; 18:297–302.
Article23. O'Donnell DE, Guenette JA, Maltais F, Webb KA. Decline of resting inspiratory capacity in COPD: the impact on breathing pattern, dyspnea, and ventilatory capacity during exercise. Chest. 2012; 141:753–762.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Spontaneous Regression of Small Cell Lung Cancer
- The Relationship between (the) Loss of Blood Group Antigen A in Cancer Tissue and Survival Time in the Antigen A Positive Non-Small Cell Lung Cancer
- The Prognostic Role of Vascular Endothelial Growth Factor (VEGF) Expression and Angiogenesis in Curatively Resected Non-Small Cell Lung Cancer
- Cutaneous Metastasis from Small Cell Lung Cancer Expressing Thyroid Transcription Factor-1
- Ovarian Metastasis from Non-Small Cell Lung Cancer Responding to Erlotinib