Yonsei Med J.
2016 May;57(3):626-634. 10.3349/ymj.2016.57.3.626.
Outcomes before and after the Implementation of a Critical Pathway for Patients with Acute Aortic Disease
- Affiliations
-
- 1Department of Emergency Medicine, Yonsei University College of Medicine, Seoul, Korea. boringzzz@yuhs.ac
- 2Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Emergency Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 4Division of Cardiovascular Surgery, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Yonsei University Health System, Seoul, Korea.
- 5Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea.
- KMID: 2374081
- DOI: http://doi.org/10.3349/ymj.2016.57.3.626
Abstract
- PURPOSE
Acute aortic diseases, such as aortic dissection and aortic aneurysm, can be life-threatening vascular conditions. In this study, we compared outcomes before and after the implementation of a critical pathway (CP) for patients with acute aortic disease at the emergency department (ED).
MATERIALS AND METHODS
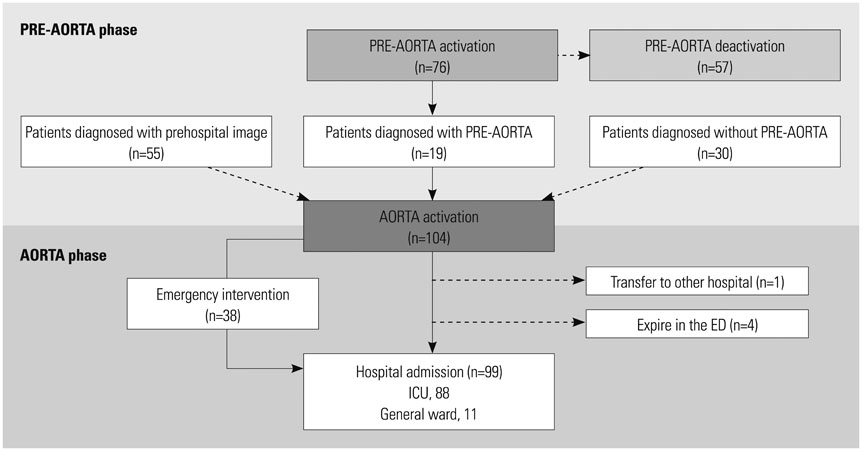
This was a retrospective observational cohort study. The CP was composed of two phases: PRE-AORTA for early diagnosis and AORTA for prompt treatment. We compared patients who were diagnosed with acute aortic disease between pre-period (January 2010 to December 2011) and post-period (July 2012 to June 2014).
RESULTS
Ninety-four and 104 patients were diagnosed with acute aortic disease in the pre- and post-periods, respectively. After the implementation of the CP, 38.7% of acute aortic disease cases were diagnosed via PRE-AORTA. The door-to-CT time was reduced more in PRE-AORTA-activated patients [71.0 (61.0, 115.0) min vs. 113.0 (56.0, 170.5) min; p=0.026]. During the post-period, more patients received emergency intervention than during the pre-period (22.3% vs. 36.5%; p=0.029). Time until emergency intervention was reduced in patients, who visited the ED directly, from 378.0 (302.0, 489.0) min in the pre-period to 200.0 (170.0, 299.0) min in the post-period (p=0.001). The number of patients who died in the ED declined from 11 to 4 from the pre-period to the post-period. Hospital mortality decreased from 26.6% to 14.4% in the post-period (p=0.033).
CONCLUSION
After the implementation of a CP for patients with acute aortic disease, more patients received emergency intervention within a shorter time, resulting in improved hospital mortality.
MeSH Terms
-
Acute Disease
Adult
Aged
Aneurysm, Dissecting/diagnosis/mortality/*surgery
Aorta
Aortic Aneurysm/diagnosis/mortality/*surgery
Aortic Diseases/diagnosis/mortality/*surgery
*Critical Pathways
Emergency Service, Hospital/*organization & administration
Female
Hospital Mortality
Humans
Male
Middle Aged
Outcome and Process Assessment (Health Care)
Postoperative Complications/mortality
Republic of Korea/epidemiology
Retrospective Studies
Time Factors
Treatment Outcome
Vascular Surgical Procedures/*methods
Figure
Reference
-
1. Hansen MS, Nogareda GJ, Hutchison SJ. Frequency of and inappropriate treatment of misdiagnosis of acute aortic dissection. Am J Cardiol. 2007; 99:852–856.
Article2. Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000; 283:897–903.
Article3. Sullivan PR, Wolfson AB, Leckey RD, Burke JL. Diagnosis of acute thoracic aortic dissection in the emergency department. Am J Emerg Med. 2000; 18:46–50.
Article4. Chua M, Ibrahim I, Neo X, Sorokin V, Shen L, Ooi SB. Acute aortic dissection in the ED: risk factors and predictors for missed diagnosis. Am J Emerg Med. 2012; 30:1622–1626.
Article5. Leitman IM, Suzuki K, Wengrofsky AJ, Menashe E, Poplawski M, Woo KM, et al. Early recognition of acute thoracic aortic dissection and aneurysm. World J Emerg Surg. 2013; 8:47.
Article6. Rapezzi C, Longhi S, Graziosi M, Biagini E, Terzi F, Cooke RM, et al. Risk factors for diagnostic delay in acute aortic dissection. Am J Cardiol. 2008; 102:1399–1406.
Article7. Nienaber CA, Powell JT. Management of acute aortic syndromes. Eur Heart J. 2012; 33:26–35b.
Article8. Davies MG, Younes HK, Harris PW, Masud F, Croft BA, Reardon MJ, et al. Outcomes before and after initiation of an acute aortic treatment center. J Vasc Surg. 2010; 52:1478–1485.
Article9. Bounoua F, Schuster R, Grewal P, Waxman K, Cisek P. Ruptured abdominal aortic aneurysm: does trauma center designation affect outcome? Ann Vasc Surg. 2007; 21:133–136.
Article10. Hirst AE Jr, Johns VJ Jr, Kime SW Jr. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore). 1958; 37:217–279.11. Steinberg BA, Jollis JG, Winkler A, Granger C, Newby LK. Treatment pathways and quality improvement for patients with acute myocardial infarction at a tertiary care center. Crit Pathw Cardiol. 2012; 11:77–80.
Article12. De Luca A, Toni D, Lauria L, Sacchetti ML, Giorgi Rossi P, Ferri M, et al. An emergency clinical pathway for stroke patients--results of a cluster randomised trial (isrctn41456865). BMC Health Serv Res. 2009; 9:14.13. Jones AE, Shapiro NI, Roshon M. Implementing early goal-directed therapy in the emergency setting: the challenges and experiences of translating research innovations into clinical reality in academic and community settings. Acad Emerg Med. 2007; 14:1072–1078.
Article14. Grau JB, Kuschner CE, Ferrari G, Wilson SR, Brizzio ME, Zapolanski A, et al. Effects of a protocol-based management of type A aortic dissections. J Surg Res. 2015; 197:265–269.
Article15. von Kodolitsch Y, Schwartz AG, Nienaber CA. Clinical prediction of acute aortic dissection. Arch Intern Med. 2000; 160:2977–2982.
Article16. Klompas M. Does this patient have an acute thoracic aortic dissection? JAMA. 2002; 287:2262–2272.
Article17. Azhar B, Patel SR, Holt PJ, Hinchliffe RJ, Thompson MM, Karthikesalingam A. Misdiagnosis of ruptured abdominal aortic aneurysm: systematic review and meta-analysis. J Endovasc Ther. 2014; 21:568–575.
Article18. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010; 121:e266–e369.19. Rogers AM, Hermann LK, Booher AM, Nienaber CA, Williams DM, Kazerooni EA, et al. Sensitivity of the aortic dissection detection risk score, a novel guideline-based tool for identification of acute aortic dissection at initial presentation: results from the international registry of acute aortic dissection. Circulation. 2011; 123:2213–2218.
Article20. Asha SE, Miers JW. A systematic review and meta-analysis of D-dimer as a rule-out test for suspected acute aortic dissection. Ann Emerg Med. 2015; 66:368–378.
Article21. Yoshimuta T, Yokoyama H, Okajima T, Tanaka H, Toyoda K, Nagatsuka K, et al. Impact of elevated D-dimer on diagnosis of acute aortic dissection with isolated neurological symptoms in ischemic stroke. Circ J. 2015; 79:1841–1845.
Article22. Nazerian P, Morello F, Vanni S, Bono A, Castelli M, Forno D, et al. Combined use of aortic dissection detection risk score and D-dimer in the diagnostic workup of suspected acute aortic dissection. Int J Cardiol. 2014; 175:78–82.
Article23. Dueck AD, Kucey DS, Johnston KW, Alter D, Laupacis A. Survival after ruptured abdominal aortic aneurysm: effect of patient, surgeon, and hospital factors. J Vasc Surg. 2004; 39:1253–1260.
Article24. Utter GH, Maier RV, Rivara FP, Nathens AB. Outcomes after ruptured abdominal aortic aneurysms: the "halo effect" of trauma center designation. J Am Coll Surg. 2006; 203:498–505.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implementation of a Critical Pathway for Patients with Acute Cholecystitis
- Implementation of a Critical Pathway to the Dizzy Patients in the Emergency Center
- Retrospective Assessment of the Implementation of Critical Pathway in Stroke Patients in a Single University Hospital
- Neurovascular Complications of Acute Aortic Syndrome
- Implementation and Outcomes of a Critical Pathway for Lumbar Laminectomy or Microdiscectomy