Korean J Ophthalmol.
2016 Dec;30(6):434-442. 10.3341/kjo.2016.30.6.434.
Effectiveness of Toric Orthokeratology in the Treatment of Patients with Combined Myopia and Astigmatism
- Affiliations
-
- 1Department of Ophthalmology, The Catholic University of Korea College of Medicine, Seoul, Korea. githen@hanmail.net
- 2Department of Ophthalmology, Myunggok Medical Research Institute, Konyang University College of Medicine, Daejeon, Korea.
- KMID: 2374001
- DOI: http://doi.org/10.3341/kjo.2016.30.6.434
Abstract
- PURPOSE
The purpose of this multi-institute, single-group clinical trial was to evaluate the effectiveness and safety of toric orthokeratology lenses for the treatment of patients with combined myopia and astigmatism.
METHODS
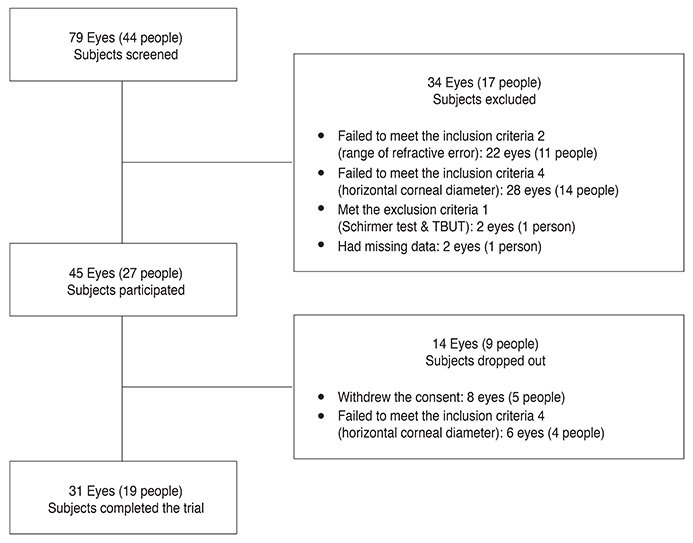
A total of 44 patients were included in this clinical trial. The patients ranged in age from 7 to 49 years, with myopia of -0.75 to -6.0 diopters (D) and astigmatism of 1.25 to 4.0 D. After excluding 21 subjects, 23 subjects (39 eyes) were analyzed after toric orthokeratology lens use. The subjects underwent ophthalmologic examination after 1 day and 1, 2, 3, and 4 weeks of wearing overnight toric orthokeratology lenses.
RESULTS
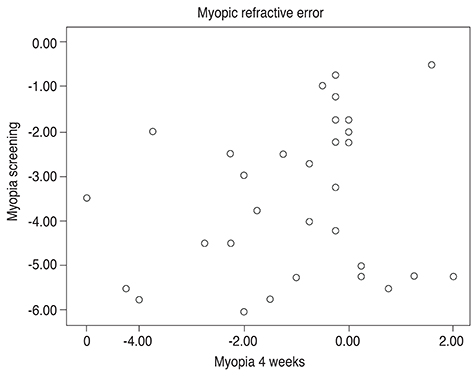
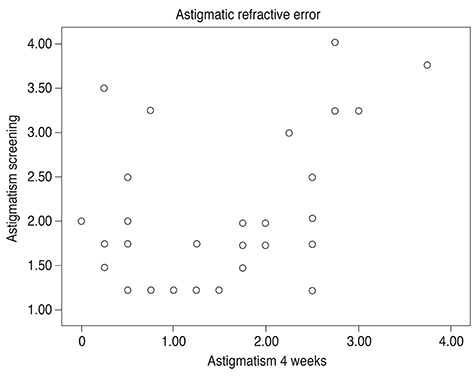
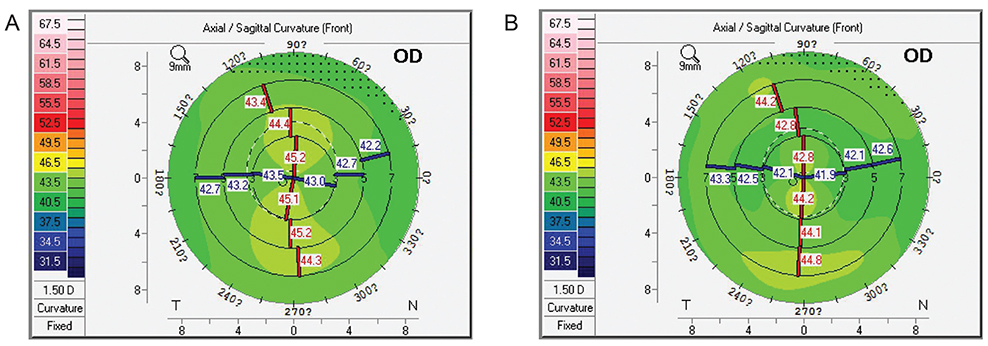
A total of 19 subjects (31 eyes) completed the trial after five subjects (eight eyes) dropped out. In the patients who completed the study by wearing lenses for 4 weeks, the myopic refractive error decreased significantly by 2.60 ± 2.21 D (p < 0.001), from -3.65 ± 1.62 to -1.05 ± 1.64 D. The astigmatic refractive error were also significantly decreased by 0.63 ± 0.98 D (p = 0.001), from 2.07 ± 0.83 to 1.44 ± 0.99 D. The mean uncorrected and corrected visual acuities before wearing the lenses were 2.14 ± 0.80 logarithm of the logMAR (logMAR) and 0.05 ± 0.13 logMAR, respectively, which changed to 0.12 ± 0.30 logarithm of the logMAR (p < 0.001) and 0.01 ± 0.04 logMAR (p = 0.156) after 4 weeks. No serious adverse reactions were reported during the clinical trial.
CONCLUSIONS
Our results suggest that toric orthokeratology is an effective and safe treatment for correcting visual acuity in patients with combined myopia and astigmatism.
MeSH Terms
Figure
Reference
-
1. Davidorf JM, Zaldivar R, Oscherow S. Results and complications of laser in situ keratomileusis by experienced surgeons. J Refract Surg. 1998; 14:114–122.2. Ahn JY, Kwon JW, Lee SM, et al. Comparison of the flap complication rate between microkeratomes for LASIK. J Korean Ophthalmol Soc. 2008; 49:1425–1430.3. Walline JJ, Rah MJ, Jones LA. The Children's Overnight Orthokeratology Investigation (COOKI) pilot study. Optom Vis Sci. 2004; 81:407–413.4. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005; 30:71–80.5. Lui WO, Edwards MH, Cho P. Contact lenses in myopia reduction: from orthofocus to accelerated orthokeratology. Cont Lens Anterior Eye. 2000; 23:68–76.6. Brennan NA, Efron N, Holden BA. Oxygen permeability of hard gas permeable contact lens materials. Clin Exp Optom. 1986; 69:82–89.7. Nichols JJ, Marsich MM, Nguyen M, et al. Overnight orthokeratology. Optom Vis Sci. 2000; 77:252–259.8. Yoon KC, Mun GH, Kim SD, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008-2009. Korean J Ophthalmol. 2011; 25:421–433.9. Chen CC, Cheung SW, Cho P. Toric orthokeratology for highly astigmatic children. Optom Vis Sci. 2012; 89:849–855.10. Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE study). Invest Ophthalmol Vis Sci. 2013; 54:6510–6517.11. Efron N, Pritchard N, Brandon K, et al. A survey of the use of grading scales for contact lens complications in optometric practice. Clin Exp Optom. 2011; 94:193–199.12. Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Invest Ophthalmol Vis Sci. 2011; 52:2170–2174.13. Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012; 53:7077–7085.14. Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012; 53:3913–3919.15. Downie LE, Lowe R. Corneal reshaping influences myopic prescription stability (CRIMPS): an analysis of the effect of orthokeratology on childhood myopic refractive stability. Eye Contact Lens. 2013; 39:303–310.16. Swarbrick HA, Alharbi A, Watt K, et al. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology. 2015; 122:620–630.17. Jee DH, Hong ME, Kim MS. The efficacy and safety of Ortho-K LK lens. J Korean Ophthalmol Soc. 2003; 44:706–711.18. Lee WH, Park YK, Seo JM, Shin JH. The inhibitory effect of myopic and astigmatic progression by orthokeratology lens. J Korean Ophthalmol Soc. 2011; 52:1269–1274.19. Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom. 2002; 85:284–293.20. Chang JW, Choi TH, Lee HB. The efficacy and safety of reverse geometry lenses. J Korean Ophthalmol Soc. 2004; 45:908–912.21. Lui WO, Edwards MH. Orthokeratology in low myopia. Part 1: efficacy and predictability. Cont Lens Anterior Eye. 2000; 23:77–89.22. Jayakumar J, Swarbrick HA. The effect of age on shortterm orthokeratology. Optom Vis Sci. 2005; 82:505–511.23. Maseedupally V, Gifford P, Lum E, Swarbrick H. Central and paracentral corneal curvature changes during orthokeratology. Optom Vis Sci. 2013; 90:1249–1258.24. Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutierrez-Ortega R. Factors preventing myopia progression with orthokeratology correction. Optom Vis Sci. 2013; 90:1225–1236.25. Lian Y, Shen M, Huang S, et al. Corneal reshaping and wavefront aberrations during overnight orthokeratology. Eye Contact Lens. 2014; 40:161–168.26. Li F, Jiang ZX, Hao P, Li X. A meta-analysis of central corneal thickness changes with overnight orthokeratology. Eye Contact Lens. 2016; 42:141–146.27. Shin DB, Yang KM, Lee SB, et al. Effect of reverse geometry lens on correction of moderate-degree myopia and cornea. J Korean Ophthalmol Soc. 2003; 44:1748–1756.28. Chang SW, Hu FR, Lin LL. Effects of contact lenses on corneal endothelium: a morphological and functional study. Ophthalmologica. 2001; 215:197–203.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Toric Orthokeratology Lenses in Patients with Limbus to Limbus Corneal Astigmatism
- Correction of Limbus-to-Limbus Corneal Astigmatism with Toric Orthokeratology Lenses
- Effect of Toric Orthokeratology Lenses on Patients with More Than 1.5 Diopter of Corneal Astigmatism
- Prescription and effect of orthokeratology lenses
- Rotational Stability after Toric Implantable Collamer Lens Implantation