J Gastric Cancer.
2015 Jun;15(2):105-112. 10.5230/jgc.2015.15.2.105.
Unaided Stapling Technique for Pure Single-Incision Distal Gastrectomy in Early Gastric Cancer: Unaided Delta-Shaped Anastomosis and Uncut Roux-en-Y Anastomosis
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. hkyang@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2372357
- DOI: http://doi.org/10.5230/jgc.2015.15.2.105
Abstract
- PURPOSE
Intracorporeal anastomosis is the most difficult procedure during pure single-incision distal gastrectomy (SIDG) that affects its generalization. We introduced unaided delta-shaped anastomosis (uDelta), a novel anastomosis technique, for gastroduodenostomy after pure SIDG, and compared the results with those of previously reported Roux-en-Y anastomosis (RY).
MATERIALS AND METHODS
Between March 2014 and March 2015, SIDG with D1+ lymph node dissection was performed for early gastric cancer through a 2.5-cm transumbilical incision without any additional port. uDelta was performed by the operator alone, without any intracorporeal assistance.
RESULTS
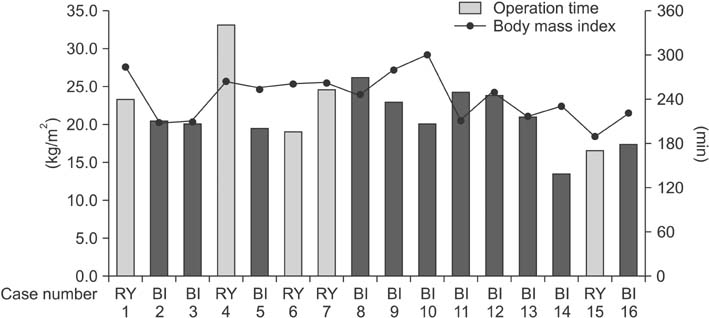
uDelta was performed on 11 patents, and uncut RY was performed on 5-patients without open or multiport conversion. R0 resection was performed in all cases. No significant differences were observed in mean age and body mass index between patients who underwent uDelta or RY. Mean operation times were 214.5+/-36.2 minutes for uDelta and 240.8+/-65.9 minutes for RY, which was not significantly different. Reconstruction time for uDelta was shorter than that for RY, with marginal statistical significance (26.1+/-8.3 minutes vs. 38.0+/-9.1 minutes, P=0.05). There were no intraoperative transfusions, 30-day mortality, or anastomosis-related complications in either group. Average length of hospital stay was 8.2+/-1.9 days in the uDelta group and 7.2+/-0.8 days in the RY group (P=0.320).
CONCLUSIONS
After carefully considering indications, uDelta can be a feasible and can be a reproducible reconstruction method after SIDG in early gastric cancer.
MeSH Terms
Figure
Cited by 1 articles
-
Intracorporeal modified delta-shaped gastroduodenostomy during 2-port distal gastrectomy: technical aspects and short-term outcomes
Sejin Lee, Jeong Ho Song, Sung Hyun Park, Minah Cho, Yoo Min Kim, Woo Jin Hyung, Hyoung-Il Kim
Ann Surg Treat Res. 2023;105(3):172-177. doi: 10.4174/astr.2023.105.3.172.
Reference
-
1. Yang HK, Suh YS, Lee HJ. Minimally invasive approaches for gastric cancer-Korean experience. J Surg Oncol. 2013; 107:277–281.2. Oh SY, Kwon S, Lee KG, Suh YS, Choe HN, Kong SH, et al. Outcomes of minimally invasive surgery for early gastric cancer are comparable with those for open surgery: analysis of 1,013 minimally invasive surgeries at a single institution. Surg Endosc. 2014; 28:789–795.3. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report: a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010; 251:417–420.4. Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P. Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc. 2012; 26:1205–1213.5. Frutos MD, Abrisqueta J, Lujan J, Abellan I, Parrilla P. Randomized prospective study to compare laparoscopic appendectomy versus umbilical single-incision appendectomy. Ann Surg. 2013; 257:413–418.6. Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nishida T. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc. 2011; 25:2400–2404.7. Omori T, Tanaka K, Tori M, Ueshima S, Akamatsu H, Nishida T. Intracorporeal circular-stapled Billroth I anastomosis in single-incision laparoscopic distal gastrectomy. Surg Endosc. 2012; 26:1490–1494.8. Ahn SH, Son SY, Lee CM, Jung do H, Park do J, Kim HH. Intracorporeal uncut Roux-en-Y gastrojejunostomy reconstruction in pure single-incision laparoscopic distal gastrectomy for early gastric cancer: unaided stapling closure. J Am Coll Surg. 2014; 218:e17–e21.9. Ahn SH, Son SY, Jung do H, Park do J, Kim HH. Pure single-port laparoscopic distal gastrectomy for early gastric cancer: comparative study with multi-port laparoscopic distal gastrectomy. J Am Coll Surg. 2014; 219:933–943.10. Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011; 11:69–77.11. Lee HJ, Shiraishi N, Kim HH, Hiki N, Uyama I, Choi SH, et al. Standard of practice on laparoscopic gastric cancer surgery in Korea and Japan: experts' survey. Asian J Endosc Surg. 2012; 5:5–11.12. Kanaya S, Gomi T, Momoi H, Tamaki N, Isobe H, Katayama T, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg. 2002; 195:284–287.13. Okabe H, Obama K, Tsunoda S, Tanaka E, Sakai Y. Advantage of completely laparoscopic gastrectomy with linear stapled reconstruction: a long-term follow-up study. Ann Surg. 2014; 259:109–116.14. Park do J, Lee JH, Ahn SH, Eng AK, Kim HH. Single-port laparoscopic distal gastrectomy with D1+β lymph node dissection for gastric cancers: report of 2 cases. Surg Laparosc Endosc Percutan Tech. 2012; 22:e214–e216.15. Omori T, Masuzawa T, Akamatsu H, Nishida T. A simple and safe method for Billroth I reconstruction in single-incision laparoscopic gastrectomy using a novel intracorporeal triangular anastomotic technique. J Gastrointest Surg. 2014; 18:613–636.16. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.17. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer;2009.18. Ozdemir BA, Thomas RL, Soon Y. Single-port laparoscopic subtotal gastrectomy with DIα lymphadenectomy. Surg Innov. 2011; 18:NP1–NP4.19. Kong J, Wu SD, Su Y. Translumenal single-incision laparoscopy radical gastrectomy with D2 lymph node dissection for early gastric cancer: primary experience with less invasive surgery in China. J Laparoendosc Adv Surg Tech A. 2013; 23:141–145.20. Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S, et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011; 14:365–371.21. Kitagami H, Morimoto M, Nozawa M, Nakamura K, Tanimura S, Murakawa K, et al. Evaluation of the delta-shaped anastomosis in laparoscopic distal gastrectomy: midterm results of a comparison with Roux-en-Y anastomosis. Surg Endosc. 2014; 28:2137–2144.22. Kim MC, Kim W, Kim HH, Ryu SW, Ryu SY, Song KY, et al. Korean Laparoscopic Gastrointestinal Surgery Study (KLASS) Group. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale Korean multicenter study. Ann Surg Oncol. 2008; 15:2692–2700.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Uncut Roux-en-Y Reconstruction after Laparoscopic Distal Gastrectomy Can Be a Favorable Method in Terms of Gastritis, Bile Reflux, and Gastric Residue
- Esophagojejunal Anastomosis after Laparoscopic Total Gastrectomy for Gastric Cancer: Circular versus Linear Stapling
- Convenience of Adding a Needle Grasper in Single-Incision Laparoscopic Distal Gastrectomy With Billroth I Anastomosis for Clinical Early Gastric Cancer
- A Peterson's hernia and subsequent small bowel volvulus: surgical reconstruction utilizing transverse colon as a new Roux-en-Y limb - 1 case
- Pancreatoduodenectomy with uncut-Roux-en-Y reconstruction in patients with previous radical gastrectomy