Prevalence and Risk Factors of Urticaria With a Focus on Chronic Urticaria in Children
- Affiliations
-
- 1Department of Pediatrics, Bundang CHA Medical Center, CHA University School of Medicine, Seongnam, Korea. drmesh@gmail.com
- 2CHA University School of Medicine, Seongnam, Korea.
- 3Department of Allergy & Clinical Immunology, Bundang CHA Medical Center, CHA University School of Medicine, Seongnam, Korea.
- 4Department of Dermatology, Bundang CHA Medical Center, CHA University School of Medicine, Seongnam, Korea.
- 5Department of Pediatrics, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea.
- 6Department of Pediatrics, CHA Gumi Medical Center, CHA University School of Medicine, Gumi, Korea.
- KMID: 2371721
- DOI: http://doi.org/10.4168/aair.2017.9.3.212
Abstract
- PURPOSE
Limited data is available on the prevalence and risk factors of acute and chronic urticaria in children. Our purpose was to determine the prevalence and identify the risk factors of acute and chronic urticaria in Korean children.
METHODS
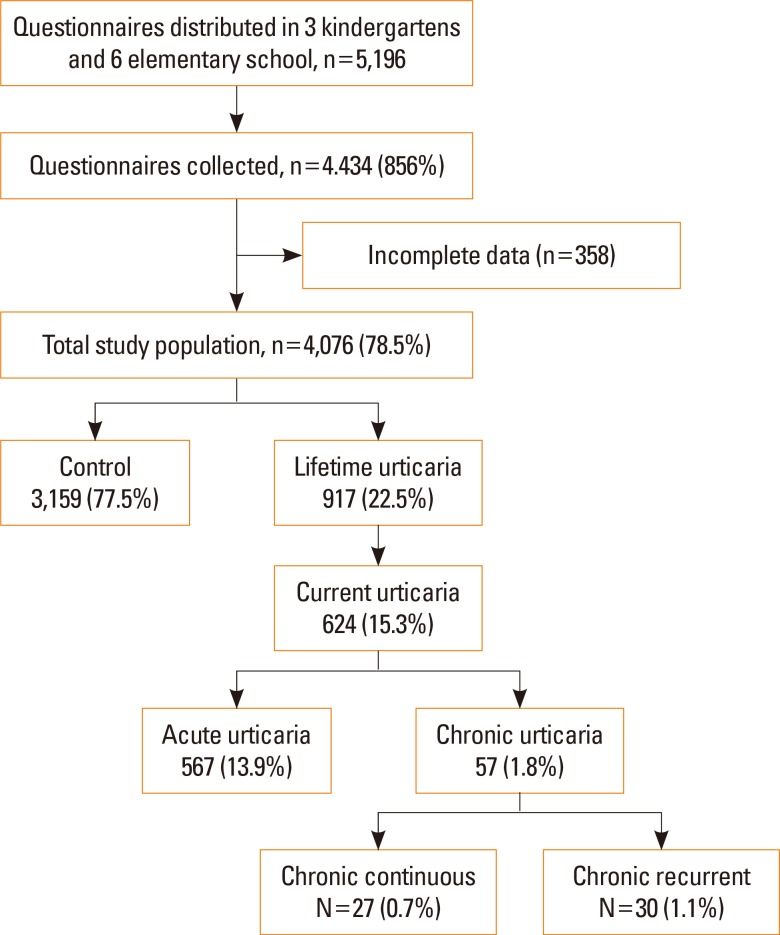
This population-based study examined 4,076 children (age 4 to 13 years) who were enrolled in the 2015 prospective Seongnam Atopy Project (SAP 2015) in Korea. The parents completed an urticaria questionnaire that included questions regarding the duration, severity, and triggering factors of urticaria. Blood sampling (n=464) was performed to measure vitamin D, total eosinophil count (TEC), and total IgE levels, and skin prick tests (n=503) were done.
RESULTS
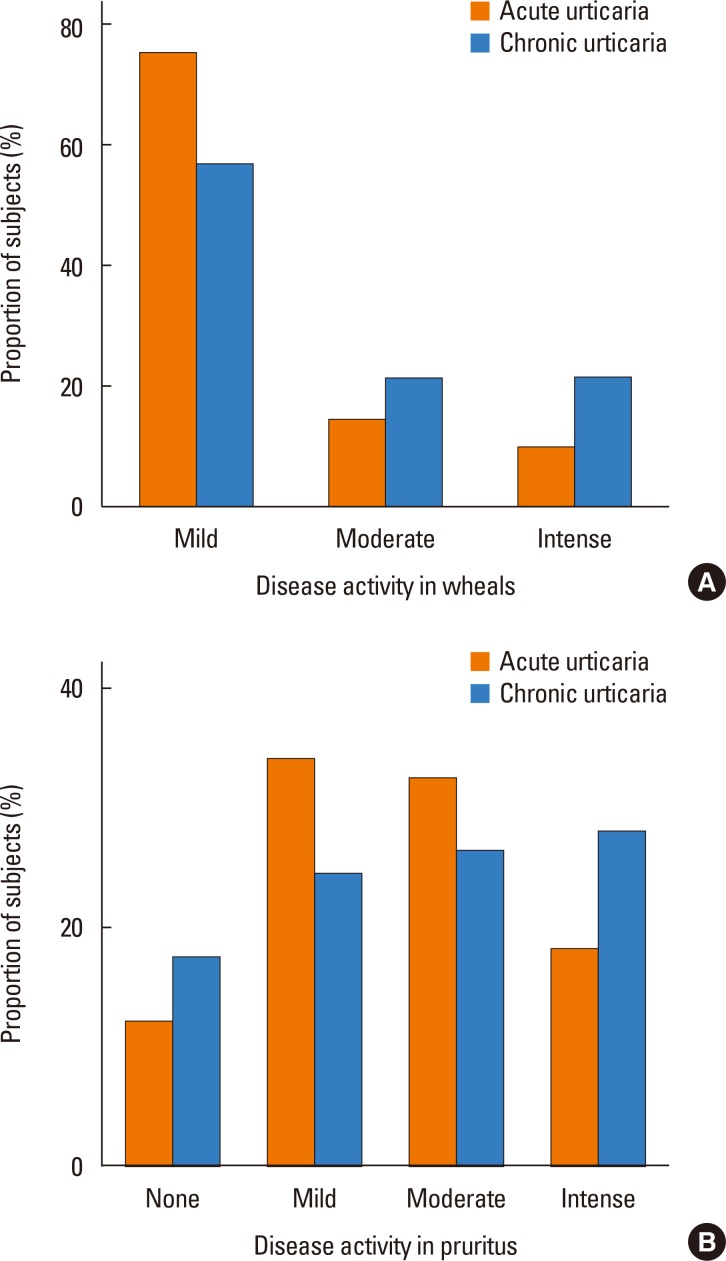
The prevalences of the life-time, acute, and chronic urticaria were 22.5%, 13.9%, and 1.8% (chronic continuous urticaria, 0.7%; and chronic recurrent urticaria, 1.1%), respectively. Acute urticaria was significantly associated with allergic diseases and parental history of allergy (P<0.001), but chronic urticaria was not associated with these clinical factors. There was no significant difference in the 25-hydroxyvitamin D level between subjects with chronic urticaria and controls (P=0.124). Chronic continuous urticaria was associated with living in a new residence (aOR=2.38, 95% CI=1.02-5.54, P=0.044) and belonging to a family with a high income (aOR=4.24, 95% CI=1.24-14.56, P=0.022).
CONCLUSIONS
A total of 1.8% of children were found to have chronic urticaria. Living in a new residence and belonging to a family with a high income increased the risk of chronic continuous urticaria.
MeSH Terms
Figure
Cited by 6 articles
-
Updated treatment guideline of chronic spontaneous urticaria
Joo Young Roh
J Korean Med Assoc. 2019;62(1):37-46. doi: 10.5124/jkma.2019.62.1.37.Economic Burden of the Inadequate Management of Allergic Rhinitis and Urticaria in Asian Countries Based on the GA2LEN Model
Kanokvalai Kulthanan, Supinda Chusakul, Marysia Tiongco Recto, Ma. Teresita Gabriel, Derrick Chen-Wee Aw, Narayanan Prepageran, Alson Wong, Jern Lin Leong, Henry Foong, Vo Thanh Quang, Torsten Zuberbier
Allergy Asthma Immunol Res. 2018;10(4):370-378. doi: 10.4168/aair.2018.10.4.370.Serum Periostin Is Negatively Correlated With Exposure to Formaldehyde and Volatile Organic Compounds in Children
Dong Keon Yon, Jaewoo An, Eun Kyo Ha, Hye Mi Jee, Kenji Izuhara, Junya Ono, Young-Ho Jung, Kyung Suk Lee, Youn Ho Sheen, Heysung Baek, Man Yong Han
Allergy Asthma Immunol Res. 2018;10(6):716-721. doi: 10.4168/aair.2018.10.6.716.Clinical Course of Chronic Spontaneous Urticaria in the Korean Adult Population
Yoon Seob Kim, Sang Hyun Park, Kyungdo Han, Ji Hyun Lee, Nack In Kim, Joo Young Roh, Seong Jun Seo, Hae Jun Song, Min-Geol Lee, Jee Ho Choi, Young Min Park
Allergy Asthma Immunol Res. 2018;10(1):83-87. doi: 10.4168/aair.2018.10.1.83.Epidemiology of Chronic Urticaria in Korea Using the Korean Health Insurance Database, 2010-2014
Nami Lee, Jeong-Dong Lee, Hyun-Young Lee, Dae Ryong Kang, Young-Min Ye
Allergy Asthma Immunol Res. 2017;9(5):438-445. doi: 10.4168/aair.2017.9.5.438.Associations Between Phthalate, Eosinophil, and Aeroallergen Sensitization in Schoolchildren
Jeongsik Yi, Ho-Sang Shin, Man Yong Han, Hee Jin Choi, Mi Seon Lee, Myongsoon Sung
J Korean Med Sci. 2023;38(45):e391. doi: 10.3346/jkms.2023.38.e391.
Reference
-
1. Brüske I, Standl M, Weidinger S, Klümper C, Hoffmann B, Schaaf B, et al. Epidemiology of urticaria in infants and young children in Germany--results from the German LISAplus and GINIplus Birth Cohort Studies. Pediatr Allergy Immunol. 2014; 25:36–42. PMID: 24236825.2. Zuberbier T, Balke M, Worm M, Edenharter G, Maurer M. Epidemiology of urticaria: a representative cross-sectional population survey. Clin Exp Dermatol. 2010; 35:869–873. PMID: 20456386.
Article3. Bernstein JA, Lang DM, Khan DA, Craig T, Dreyfus D, Hsieh F, et al. The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014; 133:1270–1277. PMID: 24766875.
Article5. Church MK, Weller K, Stock P, Maurer M. Chronic spontaneous urticaria in children: itching for insight. Pediatr Allergy Immunol. 2011; 22:1–8. PMID: 21261741.
Article6. Gaig P, Olona M, Muñoz Lejarazu D, Caballero MT, Domínguez FJ, Echechipia S, et al. Epidemiology of urticaria in Spain. J Investig Allergol Clin Immunol. 2004; 14:214–220.8. Khakoo G, Sofianou-Katsoulis A, Perkin MR, Lack G. Clinical features and natural history of physical urticaria in children. Pediatr Allergy Immunol. 2008; 19:363–366. PMID: 18167159.
Article9. Hamel-Teillac D. Chronic urticaria in children. Ann Dermatol Venereol. 2003; 130 Spec No 1:1S69–1S72. PMID: 12843811.10. Tuchinda M, Srimaruta N, Habanananda S, Vareenil J, Assatherawatts A. Urticaria in Thai children. Asian Pac J Allergy Immunol. 1986; 4:41–45. PMID: 2873823.11. Konstantinou GN, Papadopoulos NG, Tavladaki T, Tsekoura T, Tsilimigaki A, Grattan CE. Childhood acute urticaria in northern and southern Europe shows a similar epidemiological pattern and significant meteorological influences. Pediatr Allergy Immunol. 2011; 22:36–42. PMID: 21261743.
Article12. Ehlers I, Niggemann B, Binder C, Zuberbier T. Role of nonallergic hypersensitivity reactions in children with chronic urticaria. Allergy. 1998; 53:1074–1077. PMID: 9860240.
Article13. Du Toit G, Prescott R, Lawrence P, Johar A, Brown G, Weinberg EG, et al. Autoantibodies to the high-affinity IgE receptor in children with chronic urticaria. Ann Allergy Asthma Immunol. 2006; 96:341–344. PMID: 16498857.
Article14. Kulthanan K, Jiamton S, Gorvanich T, Pinkaew S. Autologous serum skin test in chronic idiopathic urticaria: prevalence, correlation and clinical implications. Asian Pac J Allergy Immunol. 2006; 24:201–206. PMID: 17348242.15. Thorp WA, Goldner W, Meza J, Poole JA. Reduced vitamin D levels in adult subjects with chronic urticaria. J Allergy Clin Immunol. 2010; 126:413. PMID: 20621341.
Article16. Woo YR, Jung KE, Koo DW, Lee JS. Vitamin D as a marker for disease severity in chronic urticaria and its possible role in pathogenesis. Ann Dermatol. 2015; 27:423–430. PMID: 26273159.
Article17. Oguz Topal I, Kocaturk E, Gungor S, Durmuscan M, Sucu V, Yıldırmak S. Does replacement of vitamin D reduce the symptom scores and improve quality of life in patients with chronic urticaria? J Dermatolog Treat. 2016; 27:163–166. PMID: 26295454.
Article18. Boonpiyathad T, Pradubpongsa P, Sangasapaviriya A. Vitamin D supplements improve urticaria symptoms and quality of life in chronic spontaneous urticaria patients: a prospective case-control study. Dermatoendocrinol. 2014; 6:e29727. PMID: 25346784.
Article19. Maurer M, Weller K, Bindslev-Jensen C, Giménez-Arnau A, Bousquet PJ, Bousquet J, et al. Unmet clinical needs in chronic spontaneous urticaria. A GA(2)LEN task force report. Allergy. 2011; 66:317–330. PMID: 21083565.20. Ferrer M. Epidemiology, healthcare, resources, use and clinical features of different types of urticaria. Alergológica 2005. J Investig Allergol Clin Immunol. 2009; 19(Suppl 2):21–26.21. Kjaer HF, Eller E, Høst A, Andersen KE, Bindslev-Jensen C. The prevalence of allergic diseases in an unselected group of 6-year-old children. The DARC birth cohort study. Pediatr Allergy Immunol. 2008; 19:737–745. PMID: 18318699.
Article22. Powell RJ, Du Toit GL, Siddique N, Leech SC, Dixon TA, Clark AT, et al. BSACI guidelines for the management of chronic urticaria and angio-oedema. Clin Exp Allergy. 2007; 37:631–650. PMID: 17456211.
Article23. Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau A, et al. EAACI/GA(2)LEN/EDF/WAO guideline: definition, classification and diagnosis of urticaria. Allergy. 2009; 64:1417–1426. PMID: 19772512.24. Mortureux P, Léauté-Labrèze C, Legrain-Lifermann V, Lamireau T, Sarlangue J, Taïeb A. Acute urticaria in infancy and early childhood: a prospective study. Arch Dermatol. 1998; 134:319–323. PMID: 9521030.25. Sackesen C, Sekerel BE, Orhan F, Kocabas CN, Tuncer A, Adalioglu G. The etiology of different forms of urticaria in childhood. Pediatr Dermatol. 2004; 21:102–108. PMID: 15078346.
Article26. Zuberbier T, Greaves MW, Juhlin L, Kobza-Black A, Maurer D, Stingl G, et al. Definition, classification, and routine diagnosis of urticaria: a consensus report. J Investig Dermatol Symp Proc. 2001; 6:123–127.27. Grattan CE, Humphreys F. British Association of Dermatologists Therapy Guidelines and Audit Subcommittee. Guidelines for evaluation and management of urticaria in adults and children. Br J Dermatol. 2007; 157:1116–1123. PMID: 18021095.
Article28. Zazzali JL, Broder MS, Chang E, Chiu MW, Hogan DJ. Cost, utilization, and patterns of medication use associated with chronic idiopathic urticaria. Ann Allergy Asthma Immunol. 2012; 108:98–102. PMID: 22289728.
Article29. Chang KL, Yang YH, Yu HH, Lee JH, Wang LC, Chiang BL. Analysis of serum total IgE, specific IgE and eosinophils in children with acute and chronic urticaria. J Microbiol Immunol Infect. 2013; 46:53–58. PMID: 22560476.
Article30. Looker AC, Dawson-Hughes B, Calvo MS, Gunter EW, Sahyoun NR. Serum 25-hydroxyvitamin D status of adolescents and adults in two seasonal subpopulations from NHANES III. Bone. 2002; 30:771–777. PMID: 11996918.
Article31. Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, et al. Vitamin D insufficiency in Korea--a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab. 2011; 96:643–651. PMID: 21190984.
Article32. Visitsunthorn N, Tuchinda M, Vichyanond P. Cold urticaria in Thai children: comparison between cyproheptadine and ketotifen in the treatment. Asian Pac J Allergy Immunol. 1995; 13:29–35. PMID: 7488341.33. Park DW, Kim SH, Moon JY, Song JS, Choi J, Kwak HJ, et al. The effect of low-VOC, water-based paint on aggravation of allergic disease in school children. Indoor Air. 2016; Forthcoming.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dermographism ( III ): Dermographism in Acute and Chronic Urticaria
- Chronic urticaria in children
- Allergen sensitization and vitamin D status in young Korean children with urticaria
- A Study on Clinical and Etiological Aspects of Chronic Urticaria by Questionnaire
- Two Cases of Cefotiam-induced Contact Urticaria Syndrome