Allergy Asthma Respir Dis.
2014 Sep;2(4):236-242. 10.4168/aard.2014.2.4.236.
Chronic urticaria in children
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jyu3922@gmail.com
- KMID: 2262390
- DOI: http://doi.org/10.4168/aard.2014.2.4.236
Abstract
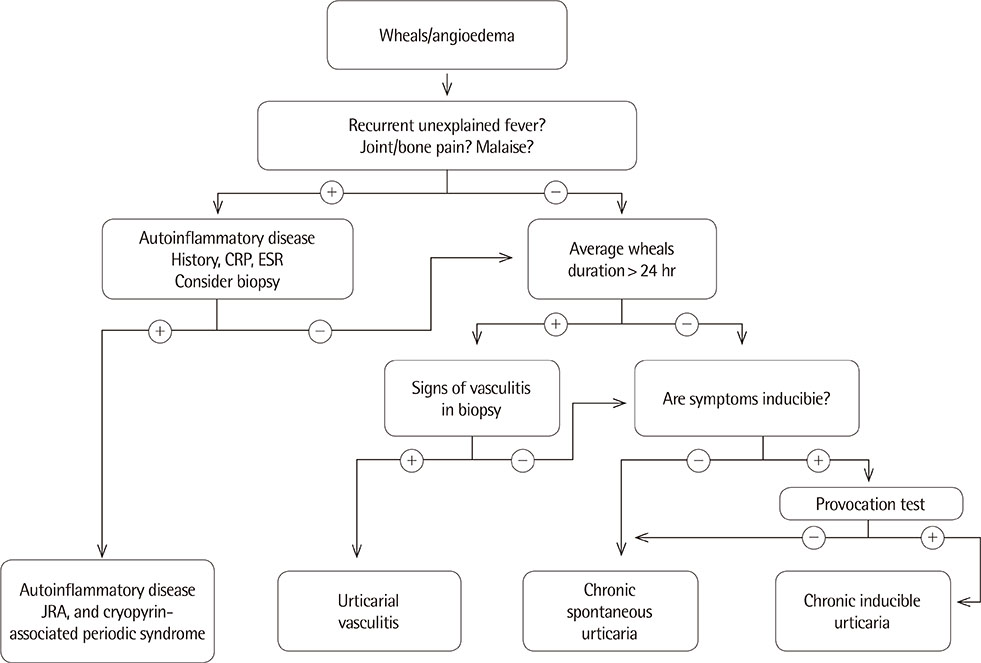
- Although it is difficult to find a cause of chronic urticaria in children, previous studies have been identified some triggers, such as autoimmunity, physical stimuli, food and its additives, and infection. History taking and physical examination remain the best tool for identifying an underlying cause of urticaria. First investigations include a complete blood count with differential, erythrocyte sedimentation rate, and C-reactive protein in children with chronic urticaria. If physical stimuli are suspected as triggers of chronic urticaria, appropriate provocation tests can be performed. Although the frequency of autoimmune urticaria was relatively high compared to the other causes in children with chronic urticaria, it is not easy to apply routine use of autologous serum skin tests to clinical practice. Additional extensive laboratory investigations are not required in the majority of cases. Second-generation H1-antihistamines are the mainstay of treatment from current guidelines in children with chronic urticaria, and dosage can be increased if the standard dose is not effective. Data on chronic urticaria in children are scarce, and causes have been considered to be similar to those in adults. Therefore, diagnostic approaches and treatment principles of chronic urticaria in children have been derived from extrapolating data in adults. In the future, comparative studies for the causes of chronic urticaria between children and adults, and therapeutic modalities for refractory cases will be needed.
MeSH Terms
Figure
Cited by 1 articles
-
Factors associated with the treatment of chronic spontaneous urticaria in children
Sun-Young Cho, Yun-Chang Choi, Byoung-Gwon Kim, Jin-A Jung
Allergy Asthma Respir Dis. 2017;5(4):211-216. doi: 10.4168/aard.2017.5.4.211.
Reference
-
1. Zitelli KB, Cordoro KM. Evidence-based evaluation and management of chronic urticaria in children. Pediatr Dermatol. 2011; 28:629–639.
Article2. Volonakis M, Katsarou-Katsari A, Stratigos J. Etiologic factors in childhood chronic urticaria. Ann Allergy. 1992; 69:61–65.3. Zuberbier T, Aberer W, Asero R, Bindslev-Jensen C, Brzoza Z, Canonica GW, et al. The EAACI/GA(2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy. 2014; 69:868–887.4. Marrouche N, Grattan C. Childhood urticaria. Curr Opin Allergy Clin Immunol. 2012; 12:485–490.
Article5. Leech S, Grattan C, Lloyd K, Deacock S, Williams L, Langford A, et al. The RCPCH care pathway for children with urticaria, angio-oedema or mastocytosis: an evidence and consensus based national approach. Arch Dis Child. 2011; 96:Suppl 2. i34–i37.
Article6. Kaplan AP. Clinical practice: chronic urticaria and angioedema. N Engl J Med. 2002; 346:175–179.7. Sahiner UM, Civelek E, Tuncer A, Yavuz ST, Karabulut E, Sackesen C, et al. Chronic urticaria: etiology and natural course in children. Int Arch Allergy Immunol. 2011; 156:224–230.
Article8. Jirapongsananuruk O, Pongpreuksa S, Sangacharoenkit P, Visitsunthorn N, Vichyanond P. Identification of the etiologies of chronic urticaria in children: a prospective study of 94 patients. Pediatr Allergy Immunol. 2010; 21:508–514.
Article9. Du Toit G, Prescott R, Lawrence P, Johar A, Brown G, Weinberg EG, et al. Autoantibodies to the high-affinity IgE receptor in children with chronic urticaria. Ann Allergy Asthma Immunol. 2006; 96:341–344.
Article10. Brunetti L, Francavilla R, Miniello VL, Platzer MH, Rizzi D, Lospalluti ML, et al. High prevalence of autoimmune urticaria in children with chronic urticaria. J Allergy Clin Immunol. 2004; 114:922–927.
Article11. Metz M, Gimenez-Arnau A, Borzova E, Grattan CE, Magerl M, Maurer M. Frequency and clinical implications of skin autoreactivity to serum versus plasma in patients with chronic urticaria. J Allergy Clin Immunol. 2009; 123:705–706.
Article12. Kilic G, Guler N, Suleyman A, Tamay Z. Chronic urticaria and autoimmunity in children. Pediatr Allergy Immunol. 2010; 21:837–842.
Article13. Konstantinou GN, Papadopoulos NG, Tavladaki T, Tsekoura T, Tsilimigaki A, Grattan CE. Childhood acute urticaria in northern and southern Europe shows a similar epidemiological pattern and significant meteorological influences. Pediatr Allergy Immunol. 2011; 22(1 Pt 1):36–42.
Article14. Harris A, Twarog FJ, Geha RS. Chronic urticaria in childhood: natural course and etiology. Ann Allergy. 1983; 51(2 Pt 1):161–165.15. Magerl M, Pisarevskaja D, Scheufele R, Zuberbier T, Maurer M. Effects of a pseudoallergen-free diet on chronic spontaneous urticaria: a prospective trial. Allergy. 2010; 65:78–83.
Article16. Ehlers I, Niggemann B, Binder C, Zuberbier T. Role of nonallergic hypersensitivity reactions in children with chronic urticaria. Allergy. 1998; 53:1074–1077.
Article17. de Martino M, Peruzzi M, Galli L, Lega L, Zammarchi E, Vierucci A. Food-additive intolerance and its correlation with atopy in children with recurrent or intermittent urticaria-angioedema. Pediatr Allergy Immunol. 1992; 3:33–38.
Article18. Caffarelli C, Cuomo B, Cardinale F, Barberi S, Dascola CP, Agostinis F, et al. Aetiological factors associated with chronic urticaria in children: a systematic review. Acta Derm Venereol. 2013; 93:268–272.
Article19. Reese I, Zuberbier T, Bunselmeyer B, Erdmann S, Henzgen M, Fuchs T, et al. Diagnostic approach for suspected pseudoallergic reaction to food ingredients. J Dtsch Dermatol Ges. 2009; 7:70–77.
Article20. Liu TH, Lin YR, Yang KC, Tsai YG, Fu YC, Wu TK, et al. Significant factors associated with severity and outcome of an initial episode of acute urticaria in children. Pediatr Allergy Immunol. 2010; 21:1043–1051.
Article21. Church MK, Weller K, Stock P, Maurer M. Chronic spontaneous urticaria in children: itching for insight. Pediatr Allergy Immunol. 2011; 22(1 Pt 1):1–8.
Article22. Schuller DE, Elvey SM. Acute urticaria associated with streptococcal infection. Pediatrics. 1980; 65:592–596.
Article23. Kano Y, Mitsuyama Y, Hirahara K, Shiohara T. Mycoplasma pneumoniae infection-induced erythema nodosum, anaphylactoid purpura, and acute urticaria in 3 people in a single family. J Am Acad Dermatol. 2007; 57:2 Suppl. S33–S35.
Article24. Sackesen C, Sekerel BE, Orhan F, Kocabas CN, Tuncer A, Adalioglu G. The etiology of different forms of urticaria in childhood. Pediatr Dermatol. 2004; 21:102–108.
Article25. Powell RJ, Du Toit GL, Siddique N, Leech SC, Dixon TA, Clark AT, et al. BSACI guidelines for the management of chronic urticaria and angiooedema. Clin Exp Allergy. 2007; 37:631–650.
Article26. Wustlich S, Brehler R, Luger TA, Pohle T, Domschke W, Foerster E. Helicobacter pylori as a possible bacterial focus of chronic urticaria. Dermatology. 1999; 198:130–132.
Article27. Schnyder B, Helbling A, Pichler WJ. Chronic idiopathic urticaria: natural course and association with Helicobacter pylori infection. Int Arch Allergy Immunol. 1999; 119:60–63.
Article28. Valsecchi R, Pigatto P. Chronic urticaria and Helicobacter pylori. Acta Derm Venereol. 1998; 78:440–442.
Article29. Tebbe B, Geilen CC, Schulzke JD, Bojarski C, Radenhausen M, Orfanos CE. Helicobacter pylori infection and chronic urticaria. J Am Acad Dermatol. 1996; 34:685–686.
Article30. Bretag AH, Archer RS, Atkinson HM, Woods WH. Circadian urticaria: another campylobacter association. Lancet. 1984; 1:954.
Article31. Akelma AZ, Cizmeci MN, Mete E, Tufan N, Bozkurt B. A neglected cause for chronic spontaneous urticaria in children: Helicobacter pylori. Allergol Immunopathol (Madr). 2014; 03. 20. [Epub]. http://dx.doi.org/10.1016/j.aller.2013.12.001.
Article32. Caubet JC, Kaiser L, Lemaître B, Fellay B, Gervaix A, Eigenmann PA. The role of penicillin in benign skin rashes in childhood: a prospective study based on drug rechallenge. J Allergy Clin Immunol. 2011; 127:218–222.
Article33. Levy Y, Segal N, Weintrob N, Danon YL. Chronic urticaria: association with thyroid autoimmunity. Arch Dis Child. 2003; 88:517–519.
Article34. Heymann WR. Chronic urticaria and angioedema associated with thyroid autoimmunity: review and therapeutic implications. J Am Acad Dermatol. 1999; 40(2 Pt 1):229–232.
Article35. Zauli D, Deleonardi G, Foderaro S, Grassi A, Bortolotti R, Ballardini G, et al. Thyroid autoimmunity in chronic urticaria. Allergy Asthma Proc. 2001; 22:93–95.
Article36. Leznoff A, Josse RG, Denburg J, Dolovich J. Association of chronic urticaria and angioedema with thyroid autoimmunity. Arch Dermatol. 1983; 119:636–640.
Article37. Dalal I, Levine A, Somekh E, Mizrahi A, Hanukoglu A. Chronic urticaria in children: expanding the "autoimmune kaleidoscope". Pediatrics. 2000; 106:1139–1141.
Article38. Magerl M, Borzova E, Gimenez-Arnau A, Grattan CE, Lawlor F, Mathelier-Fusade P, et al. The definition and diagnostic testing of physical and cholinergic urticarias--EAACI/GA2LEN/EDF/UNEV consensus panel recommendations. Allergy. 2009; 64:1715–1721.
Article39. Khakoo G, Sofianou-Katsoulis A, Perkin MR, Lack G. Clinical features and natural history of physical urticaria in children. Pediatr Allergy Immunol. 2008; 19:363–366.
Article40. Alangari AA, Twarog FJ, Shih MC, Schneider LC. Clinical features and anaphylaxis in children with cold urticaria. Pediatrics. 2004; 113:e313–e317.
Article41. Pite H, Wedi B, Borrego LM, Kapp A, Raap U. Management of childhood urticaria: current knowledge and practical recommendations. Acta Derm Venereol. 2013; 93:500–508.
Article42. Najib U, Sheikh J. The spectrum of chronic urticaria. Allergy Asthma Proc. 2009; 30:1–10.
Article43. Mathes EF, Gilliam AE. A four-year-old boy with fever, rash, and arthritis. Semin Cutan Med Surg. 2007; 26:179–187.
Article44. Thomas P, Perkin MR, Rayner N, Cox H, Fox AT, Leech S, et al. The investigation of chronic urticaria in childhood: which investigations are being performed and which are recommended? Clin Exp Allergy. 2008; 38:1061–1062.
Article45. Church MK, Maurer M, Simons FE, Bindslev-Jensen C, van Cauwenberge P, Bousquet J, et al. Risk of first-generation H(1)-antihistamines: a GA(2)LEN position paper. Allergy. 2010; 65:459–466.
Article46. Fedorowicz Z, van Zuuren EJ, Hu N. Histamine H2-receptor antagonists for urticaria. Cochrane Database Syst Rev. 2012; 3:CD008596.
Article47. Nettis E, Colanardi MC, Paradiso MT, Ferrannini A. Desloratadine in combination with montelukast in the treatment of chronic urticaria: a randomized, double-blind, placebo-controlled study. Clin Exp Allergy. 2004; 34:1401–1407.
Article48. Wan KS. Efficacy of leukotriene receptor antagonist with an anti-H1 receptor antagonist for treatment of chronic idiopathic urticaria. J Dermatolog Treat. 2009; 20:194–197.
Article49. Doshi DR, Weinberger MM. Experience with cyclosporine in children with chronic idiopathic urticaria. Pediatr Dermatol. 2009; 26:409–413.
Article50. Saini S, Rosen KE, Hsieh HJ, Wong DA, Conner E, Kaplan A, et al. A randomized, placebo-controlled, dose-ranging study of single-dose omalizumab in patients with H1-antihistamine-refractory chronic idiopathic urticaria. J Allergy Clin Immunol. 2011; 128:567–573.e1.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dermographism ( III ): Dermographism in Acute and Chronic Urticaria
- A Study on Clinical and Etiological Aspects of Chronic Urticaria by Questionnaire
- Approaches to the diagnosis and management of chronic urticaria in children
- Allergen sensitization and vitamin D status in young Korean children with urticaria
- Elevated Circulating ICAM-1 and Eosinophil Cationic Protein in Children with Chronic Urticaria