Ann Rehabil Med.
2016 Dec;40(6):1144-1148. 10.5535/arm.2016.40.6.1144.
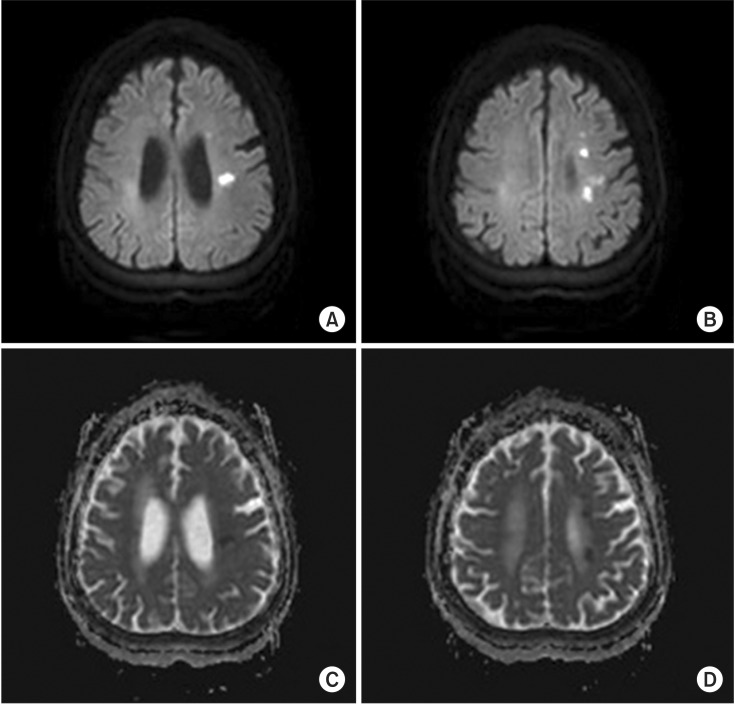
Acute Cerebral Infarction as a Rare Thrombotic Event in Myelodysplastic Syndrome: A Case Report
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. rehabit@inje.ac.kr
- KMID: 2371350
- DOI: http://doi.org/10.5535/arm.2016.40.6.1144
Abstract
- Myelodysplastic syndrome (MDS) is a bone marrow failure syndrome characterized by cytopenia that results in high risks of infection and bleeding. However, there are few reports of cerebral infarction in MDS. We reported a 72-year-old female with MDS who developed acute cerebral infarction. Clinical history of the patient revealed no definite risk factors for stroke except diabetes mellitus and dyslipidemia that was well controlled. This case represented the rare occurrence of arterial thrombosis causing acute cerebral infarction in MDS, which may be due to complex chromosomal abnormality and inflammatory processes.
Keyword
MeSH Terms
Figure
Reference
-
1. Bennett JM, Kouides PA, Forman SJ. The myelodysplastic syndromes: morphology, risk assessment, and clinical management (2002). Int J Hematol. 2002; 76(Suppl 2):228–238. PMID: 12430930.
Article2. Yang X, Brandenburg NA, Freeman J, Salomon ML, Zeldis JB, Knight RD, et al. Venous thromboembolism in myelodysplastic syndrome patients receiving lenalidomide: results from postmarketing surveillance and data mining techniques. Clin Drug Investig. 2009; 29:161–171.3. Smith SW, Sato M, Gore SD, Baer MR, Ke X, McNally D, et al. Erythropoiesis-stimulating agents are not associated with increased risk of thrombosis in patients with myelodysplastic syndromes. Haematologica. 2012; 97:15–20. PMID: 22102702.
Article4. DailyMed. VIDAZA: azacitidine injection, powder, lyophilized, for solution [Internet]. Maryland: US National Library of Medicine;c2016. cited 2016 Nov 12. Available from: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=3495a71a-cc04-4776-851f-f185956f32af.5. American Diabetes Association. Older adults. Diabetes Care. 2016; 39(Suppl 1):S81–S85. PMID: 26696686.6. D'Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke. 1994; 25:40–43. PMID: 8266381.7. Kimura S, Kuroda J, Akaogi T, Hayashi H, Kobayashi Y, Kondo M. Trisomy 8 involved in myelodysplastic syndromes as a risk factor for intestinal ulcers and thrombosis: Behcet's syndrome. Leuk Lymphoma. 2001; 42:115–121. PMID: 11699198.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guillain-Barre Syndrome Following Acute Cerebral Infarction
- Isolated Splenic Infarction in a Girl with Systemic Lupus Erythematosus
- Sweet's Syndrome with Myelodysplastic Syndrome Progressing to Acute Myelogenous Leukemia
- A Case of Thrombotic Thrombocytopenic Purpura associated with Clopidogrel in a Patient with Acute Cerebral Infarction
- Opalski Syndrome Presenting as Sensorimotor Deficits Ipsilateral to Cerebral Infarction