Ann Dermatol.
2016 Dec;28(6):733-739. 10.5021/ad.2016.28.6.733.
Efficacy and Safety of Cream Containing Climbazole/Piroctone Olamine for Facial Seborrheic Dermatitis: A Single-Center, Open-Label Split-Face Clinical Study
- Affiliations
-
- 1Department of Dermatology, Konkuk University School of Medicine, Seoul, Korea. 20050078@kuh.ac.kr
- 2Department of Systems Biotechnology, Chung-Ang University, Anseong, Korea.
- 3Research Institute of Medical Science, Konkuk University, Seoul, Korea.
- KMID: 2368124
- DOI: http://doi.org/10.5021/ad.2016.28.6.733
Abstract
- BACKGROUND
Seborrheic dermatitis (SD) is a multifactorial disease; Malassezia species play an important role in its pathogenesis.
OBJECTIVE
We aimed to determine whether a cream containing climbazole/piroctone olamine (C/P cream), antifungal agents with expected efficacy against Malassezia species, could improve SD symptoms.
METHODS
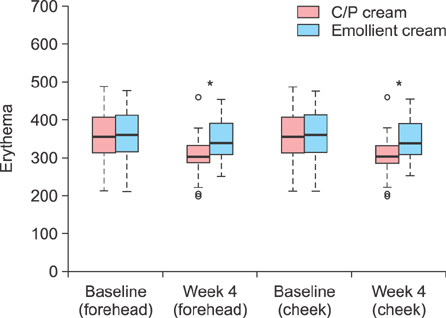
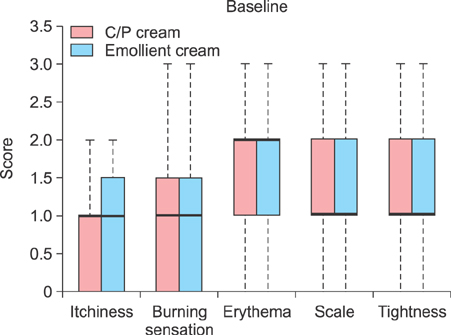
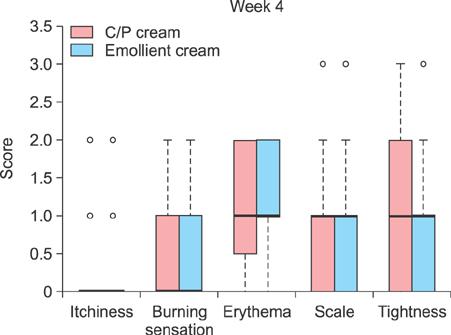
We instructed 24 patients with mild-to-moderate SD to apply the C/P cream and emollient cream on the right and left sides of the face, respectively, every morning and evening for 4 weeks. The casual sebum level (measured with Sebumeter®; Courage & Khazaka Electronic GmbH, Germany) and the extent of erythema (measured with Mexameter®; Courage & Khazaka Electronic GmbH) on the face were measured at baseline and after 4 weeks. The minimal inhibitory concentration (MIC) was determined to demonstrate the antifungal activity of the C/P cream.
RESULTS
The casual sebum level and erythema were measured at week 4, and the median values demonstrated a quantitative improvement on the C/P cream-treated right side of the face compared to the emollient cream-treated left side. For the C/P cream, the MICs were 0.625, 5, 0.625, and 2.5 mg/ml for Malassezia restricta, M. globosa, M. sympodialis, and M. slooffiae, respectively.
CONCLUSION
Based on the reduced casual sebum level and extent of erythema, the antifungal activity of C/P cream against Malassezia species seems useful for the treatment of mild to moderate SD.
MeSH Terms
Figure
Cited by 1 articles
-
Pharmacologic treatment of seborrheic dermatitis
Min Seok Hur, Yang Won Lee
J Korean Med Assoc. 2017;60(5):409-416. doi: 10.5124/jkma.2017.60.5.409.
Reference
-
1. Gupta AK, Bluhm R. Seborrheic dermatitis. J Eur Acad Dermatol Venereol. 2004; 18:13–26.
Article2. Elewski BE. Safe and effective treatment of seborrheic dermatitis. Cutis. 2009; 83:333–338.3. Gupta AK, Bluhm R, Cooper EA, Summerbell RC, Batra R. Seborrheic dermatitis. Dermatol Clin. 2003; 21:401–412.
Article4. Alizadeh N, Monadi Nori H, Golchi J, Eshkevari SS, Kazemnejad E, Darjani A. Comparison the efficacy of fluconazole and terbinafine in patients with moderate to severe seborrheic dermatitis. Dermatol Res Pract. 2014; 2014:705402.
Article5. Kastarinen H, Okokon EO, Verbeek JH. Topical antiinflammatory agents for seborrheic dermatitis of the face or scalp: summary of a Cochrane Review. JAMA Dermatol. 2015; 151:221–222.
Article6. Shemer A, Kaplan B, Nathansohn N, Grunwald MH, Amichai B, Trau H. Treatment of moderate to severe facial seborrheic dermatitis with itraconazole: an open noncomparative study. Isr Med Assoc J. 2008; 10:417–418.7. Del Rosso JQ. Adult seborrheic dermatitis: a status report on practical topical management. J Clin Aesthet Dermatol. 2011; 4:32–38.8. Schmidt-Rose T, Braren S, Fölster H, Hillemann T, Oltrogge B, Philipp P, et al. Efficacy of a piroctone olamine/climbazol shampoo in comparison with a zinc pyrithione shampoo in subjects with moderate to severe dandruff. Int J Cosmet Sci. 2011; 33:276–282.
Article9. Barac A, Pekmezovic M, Milobratovic D, Otasevic-Tasic S, Radunovic M, Arsic Arsenijevic V. Presence, species distribution, and density of Malassezia yeast in patients with seborrhoeic dermatitis-a community-based case-control study and review of literature. Mycoses. 2015; 58:69–75.
Article10. Leeming JP, Notman FH. Improved methods for isolation and enumeration of Malassezia furfur from human skin. J Clin Microbiol. 1987; 25:2017–2019.
Article11. Sugita T, Tajima M, Ito T, Saito M, Tsuboi R, Nishikawa A. Antifungal activities of tacrolimus and azole agents against the eleven currently accepted Malassezia species. J Clin Microbiol. 2005; 43:2824–2829.
Article12. Dessinioti C, Katsambas A. Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies. Clin Dermatol. 2013; 31:343–351.13. Heng MC, Henderson CL, Barker DC, Haberfelde G. Correlation of Pityosporum ovale density with clinical severity of seborrheic dermatitis as assessed by a simplified technique. J Am Acad Dermatol. 1990; 23:82–86.
Article14. Schwartz RA, Janusz CA, Janniger CK. Seborrheic dermatitis: an overview. Am Fam Physician. 2006; 74:125–130.15. Schwartz JR, Messenger AG, Tosti A, Todd G, Hordinsky M, Hay RJ, et al. A comprehensive pathophysiology of dandruff and seborrheic dermatitis-towards a more precise definition of scalp health. Acta Derm Venereol. 2013; 93:131–137.
Article16. Van den Bossche H, Willemsens G, Cools W, Cornelissen F, Lauwers WF, van Cutsem JM. In vitro and in vivo effects of the antimycotic drug ketoconazole on sterol synthesis. Antimicrob Agents Chemother. 1980; 17:922–928.
Article17. Joly V, Bolard J, Yeni P. In vitro models for studying toxicity of antifungal agents. Antimicrob Agents Chemother. 1992; 36:1799–1804.
Article18. Kim Y, Alpmann P, Blaum-Feder S, Krämer S, Endo T, Lu D, et al. Increased in vivo efficacy of lenalidomide by addition of piroctone olamine. In Vivo. 2011; 25:99–103.19. Scrivener Y, Cribier B. Pathogenesis of seborrheic dermatitis. Ann Dermatol Venereol. 2004; 131:119–122.20. Tsukahara M, Nishino T, Furuhashi I, Inoue H, Sato T, Matsumoto H. Synthesis and inhibitory effect of novel glycyrrhetinic acid derivatives on IL-1 beta-induced prostaglandin E(2) production in normal human dermal fibroblasts. Chem Pharm Bull (Tokyo). 2005; 53:1103–1110.
Article21. Schmidt A, Rühl-Hörster B. In vitro susceptibility of Malassezia furfur against azole compounds. Mycoses. 1996; 39:309–312.22. Schmidt A. In vitro activity of climbazole, clotrimazole and silver-sulphadiazine against isolates of Malassezia pachydermatis. Zentralbl Veterinarmed B. 1997; 44:193–197.
Article23. Prabhamanju M, Gokul Shankar S, Babu K, Ranjith MS. Herbal vs. chemical actives as antidandruff ingredients-which are more effective in the management of dandruff?-an overview. Egypt Dermatol Online J. 2009; 5:8.24. Gokulshankar S, Ranjith MS, Sumithira , Ranganathan S, Manuel F, Mohanty BK. Factors determining the antidandruff effect of climbazole in a shampoo formulation. J Appl Cosmetol. 2011; 29:135–140.25. Crespo Erchiga V, Ojeda Martos AA, Vera Casaño A, Crespo Erchiga A, Sánchez Fajardo F. Isolation and identification of Malassezia spp. In pytiriasis versicolor, seborrheic dermatitis and healthy skin. Rev Iberoam Micol. 1999; 16:S16–S21.26. Sandström Falk MH, Tengvall Linder M, Johansson C, Bartosik J, Bäck O, Särnhult T, et al. The prevalence of Malassezia yeasts in patients with atopic dermatitis, seborrhoeic dermatitis and healthy controls. Acta Derm Venereol. 2005; 85:17–23.
Article27. Gupta AK, Kohli Y, Summerbell RC, Faergemann J. Quantitative culture of Malassezia species from different body sites of individuals with or without dermatoses. Med Mycol. 2001; 39:243–251.
Article28. Tajima M, Sugita T, Nishikawa A, Tsuboi R. Molecular analysis of Malassezia microflora in seborrheic dermatitis patients: comparison with other diseases and healthy subjects. J Invest Dermatol. 2008; 128:345–351.
Article29. Patiño-Uzcátegui A, Amado Y, Cepero de García M, Chaves D, Tabima J, Motta A, et al. Virulence gene expression in Malassezia spp from individuals with seborrheic dermatitis. J Invest Dermatol. 2011; 131:2134–2136.
Article30. Lee YW, Byun HJ, Kim BJ, Kim DH, Lim YY, Lee JW, et al. Distribution of malassezia species on the scalp in korean seborrheic dermatitis patients. Ann Dermatol. 2011; 23:156–161.
Article31. Oh BH, Lee YW, Choe YB, Ahn KJ. Epidemiologic study of Malassezia yeasts in seborrheic dermatitis patients by the analysis of 26S rDNA PCR-RFLP. Ann Dermatol. 2010; 22:149–155.
Article32. Ro BI, Dawson TL. The role of sebaceous gland activity and scalp microfloral metabolism in the etiology of seborrheic dermatitis and dandruff. J Investig Dermatol Symp Proc. 2005; 10:194–197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Facial Seborrheic Dermatitis with Pimecrolimus Cream 1%: An Open-Label Clinical Study in Korean Patients
- Clinical and Biochemical Assessment of New-formula Shampoo for Scalp Seborrheic Dermatitis
- Tacrolimus ointment: An Open study for Effects on Severe Facial Atopic Dermatitis in Korean
- Malassezia Species Cultured From the Lesions of Seborrheic Dermatitis
- Pityrosporum(Malassezia) Related Diseases Especially Seborrheic Dermatitis