Ann Dermatol.
2016 Dec;28(6):725-732. 10.5021/ad.2016.28.6.725.
Awareness of Atopic Dermatitis and Attitudes toward Different Types of Medical Institutions for Its Treatment among Adult Patients and the Parents of Pediatric Patients: A Survey of 500 Participants
- Affiliations
-
- 1Department of Dermatology, Konkuk University School of Medicine, Seoul, Korea. 20050078@kuh.ac.kr
- 2Department of Dermatology, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea.
- 3Department of Dermatology, Kyung Hee University College of Medicine, Seoul, Korea.
- 4Department of Dermatology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 5Department of Dermatology, Pusan National University School of Medicine, Busan, Korea.
- 6Department of Dermatology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 7Department of Dermatology, Korea University College of Medicine, Seoul, Korea.
- 8Department of Dermatology, Chungnam National University College of Medicine, Daejeon, Korea.
- 9Research Institute of Medical Science, Konkuk University, Seoul, Korea.
- 10Department of Dermatology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 11Department of Dermatology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2368123
- DOI: http://doi.org/10.5021/ad.2016.28.6.725
Abstract
- BACKGROUND
Physicians can play a crucial role in the knowledge that patients have about a disease and its prognosis. Recently, patients with atopic dermatitis (AD) are increasingly turning from western medicine to oriental herbal medicine. However, their awareness of AD and attitude toward Western medicine and oriental herbal medicine clinics are scarcely reported.
OBJECTIVE
The aim of this study was to determine the understanding of AD among patients and their parents and to identify their awareness of and attitude toward Western medicine and oriental herbal medicine as treatments for AD.
METHODS
An online questionnaire was administered to 500 consenting respondents with AD (age, 16~49 years) and parents of children with AD (age, 0~15 years).
RESULTS
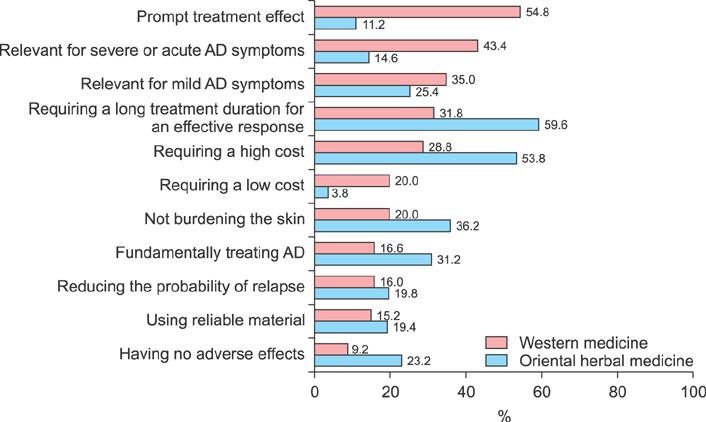
The mean percentage of correct answers to questions about AD was 52.54%. A parental history of AD was independently associated with higher respondent's knowledge about the disease and its treatment. The satisfaction with treatment outcomes was highest among patients treated at private clinic of dermatology specialists (49.4%), while lowest among those treated at oriental herbal medicine clinics (38.4%). Many participants were aware that oriental herbal medicine requires a longer treatment period for a cure and does not burden the skin, while steroid phobia was seen in most of participants.
CONCLUSION
Physicians need to educate AD patients and their parents about the disease and its treatment. Misconceptions for Western medicine and oriental herbal medicine among AD patients and parents should be corrected to improve their prognosis.
MeSH Terms
Figure
Reference
-
1. Bieber T. Atopic dermatitis. N Engl J Med. 2008; 358:1483–1494.
Article2. Ellis CN, Mancini AJ, Paller AS, Simpson EL, Eichenfield LF. Understanding and managing atopic dermatitis in adult patients. Semin Cutan Med Surg. 2012; 31:3 Suppl. S18–S22.
Article3. Margolis JS, Abuabara K, Bilker W, Hoffstad O, Margolis DJ. Persistence of mild to moderate atopic dermatitis. JAMA Dermatol. 2014; 150:593–600.
Article4. Shin JY, Kim DW, Park CW, Seo SJ, Park YL, Lee JR, et al. An educational program that contributes to improved patient and parental understanding of atopic dermatitis. Ann Dermatol. 2014; 26:66–72.
Article5. Annesi-Maesano I, Mourad C, Daures JP, Kalaboka S, Godard P. Time trends in prevalence and severity of childhood asthma and allergies from 1995 to 2002 in France. Allergy. 2009; 64:798–800.
Article6. Eichenfield LF, Hanifin JM, Beck LA, Lemanske RF Jr, Sampson HA, Weiss ST, et al. Atopic dermatitis and asthma: parallels in the evolution of treatment. Pediatrics. 2003; 111:608–616.
Article7. Foley P, Zuo Y, Plunkett A, Marks R. The frequency of common skin conditions in preschool-age children in Australia: atopic dermatitis. Arch Dermatol. 2001; 137:293–300.8. Wittkowski A, Richards HL, Griffiths CE, Main CJ. The impact of psychological and clinical factors on quality of life in individuals with atopic dermatitis. J Psychosom Res. 2004; 57:195–200.
Article9. Sánchez-Pérez J, Daudén-Tello E, Mora AM, Lara Surinyac N. Impact of atopic dermatitis on health-related quality of life in Spanish children and adults: the PSEDA study. Actas Dermosifiliogr. 2013; 104:44–52.
Article10. Kemp AS. Atopic eczema: its social and financial costs. J Paediatr Child Health. 1999; 35:229–231.
Article11. Cork MJ, Britton J, Butler L, Young S, Murphy R, Keohane SG. Comparison of parent knowledge, therapy utilization and severity of atopic eczema before and after explanation and demonstration of topical therapies by a specialist dermatology nurse. Br J Dermatol. 2003; 149:582–589.
Article12. Ben-Gashir MA, Seed PT, Hay RJ. Quality of life and disease severity are correlated in children with atopic dermatitis. Br J Dermatol. 2004; 150:284–290.
Article13. Armstrong AW, Kim RH, Idriss NZ, Larsen LN, Lio PA. Online video improves clinical outcomes in adults with atopic dermatitis: a randomized controlled trial. J Am Acad Dermatol. 2011; 64:502–507.
Article14. Moore EJ, Williams A, Manias E, Varigos G, Donath S. Eczema workshops reduce severity of childhood atopic eczema. Australas J Dermatol. 2009; 50:100–106.
Article15. Kim JE, Lee YB, Lee JH, Kim HS, Lee KH, Park YM, et al. Disease awareness and management behavior of patients with atopic dermatitis: a questionnaire survey of 313 patients. Ann Dermatol. 2015; 27:40–47.
Article16. Raffin D, Giraudeau B, Samimi M, Machet L, Pourrat X, Maruani A. Corticosteroid phobia among pharmacists regarding atopic dermatitis in children: a national french survey. Acta Derm Venereol. 2016; 96:177–180.
Article17. van Oosterhout M, Janmohamed SR, Spierings M, Hiddinga J, de Waard-van der Spek FB, Oranje AP. Correlation between Objective SCORAD and Three-Item Severity Score used by physicians and Objective PO-SCORAD used by parents/patients in children with atopic dermatitis. Dermatology. 2015; 230:105–112.
Article18. Kim DH, Li K, Seo SJ, Jo SJ, Yim HW, Kim CM, et al. A survey on understanding of atopic dermatitis among Korean patients. Korean J Dermatol. 2012; 50:201–211.19. Kwon HJ, Kim YJ, Park SB, Yu DS, Kim JW. Study of atopic dermatitis information on the internet in Korea. Korean J Dermatol. 2006; 44:137–140.20. Yoo JH, Sohn AR. Evaluation of obesity health information internet sites in Korea. Korea Sport Res. 2004; 15:249–258.21. Kupfer J, Gieler U, Diepgen TL, Fartasch M, Lob-Corzilius T, Ring J, et al. Structured education program improves the coping with atopic dermatitis in children and their parents-a multicenter, randomized controlled trial. J Psychosom Res. 2010; 68:353–358.
Article22. Ricci G, Bendandi B, Aiazzi R, Patrizi A, Masi M. Three years of Italian experience of an educational program for parents of young children affected by atopic dermatitis: improving knowledge produces lower anxiety levels in parents of children with atopic dermatitis. Pediatr Dermatol. 2009; 26:1–5.
Article23. Schmitt J, von Kobyletzki L, Svensson A, Apfelbacher C. Efficacy and tolerability of proactive treatment with topical corticosteroids and calcineurin inhibitors for atopic eczema: systematic review and meta-analysis of randomized controlled trials. Br J Dermatol. 2011; 164:415–428.
Article24. Kim C, Park KY, Ahn S, Kim DH, Li K, Kim DW, et al. Economic impact of atopic dermatitis in Korean patients. Ann Dermatol. 2015; 27:298–305.
Article25. Mancini AJ, Kaulback K, Chamlin SL. The socioeconomic impact of atopic dermatitis in the United States: a systematic review. Pediatr Dermatol. 2008; 25:1–6.
Article26. OECD. Health spending (indicator) [Internet]. OECD;2015. cited 2015 Dec 23. Available from: https://data.oecd.org/healthres/health-spending.htm.27. Aubert-Wastiaux H, Moret L, Le Rhun A, Fontenoy AM, Nguyen JM, Leux C, et al. Topical corticosteroid phobia in atopic dermatitis: a study of its nature, origins and frequency. Br J Dermatol. 2011; 165:808–814.
Article28. Hoare C, Li Wan Po A, Williams H. Systematic review of treatments for atopic eczema. Health Technol Assess. 2000; 4:1–191.
Article29. Furue M, Terao H, Rikihisa W, Urabe K, Kinukawa N, Nose Y, et al. Clinical dose and adverse effects of topical steroids in daily management of atopic dermatitis. Br J Dermatol. 2003; 148:128–133.
Article30. McHenry PM, Williams HC, Bingham EA. Management of atopic eczema. Joint Workshop of the British Association of Dermatologists and the Research Unit of the Royal College of Physicians of London. BMJ. 1995; 310:843–847.31. Berth-Jones J, Damstra RJ, Golsch S, Livden JK, Van Hooteghem O, Allegra F, et al. Twice weekly fluticasone propionate added to emollient maintenance treatment to reduce risk of relapse in atopic dermatitis: randomised, double blind, parallel group study. BMJ. 2003; 326:1367.
Article32. Tan HY, Zhang AL, Chen D, Xue CC, Lenon GB. Chinese herbal medicine for atopic dermatitis: a systematic review. J Am Acad Dermatol. 2013; 69:295–304.33. Chin HW, Jang HS, Jang BS, Jo JH, Kim MB, Oh CK, et al. A study on utilization of alternative medicine for patients with atopic dermatitis. Korean J Dermatol. 2005; 43:903–911.34. Stalder JF, Barbarot S, Wollenberg A, Holm EA, De Raeve L, Seidenari S, et al. Patient-Oriented SCORAD (PO-SCORAD): a new self-assessment scale in atopic dermatitis validated in Europe. Allergy. 2011; 66:1114–1121.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Disease Awareness and Management Behavior of Patients with Atopic Dermatitis: A Questionnaire Survey of 313 Patients
- The KAPARD guidelines for atopic dermatitis in children and adolescents: Part II. Systemic treatment, novel therapeutics, and adjuvant therapy
- A Study on the Use of Complementary Alternative Medicine in Children with Atopic Dermatitis
- Home Nursing and Quality of Life in Parents of Children with Atopic Dermatitis
- A Diagnostic Questionnaire for the Epidemiologic Studies of Childhood and Adult Atopic Dermatitis in Korea