Ann Surg Treat Res.
2017 Feb;92(2):73-81. 10.4174/astr.2017.92.2.73.
The 13-year experience of performing pancreaticoduodenectomy in a mid-volume municipal hospital
- Affiliations
-
- 1Department of Surgery, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea. ahndori68@naver.com
- KMID: 2367919
- DOI: http://doi.org/10.4174/astr.2017.92.2.73
Abstract
- PURPOSE
Pancreaticoduodenectomy (PD) is a complex surgery associated with high morbidity, mortality, and cost. Municipal hospitals have their important role in the public health and welfare system. The purpose of this study was to identify the feasibility as well as the cost-effectiveness of performing PD in a mid-volume municipal hospital based on 13 years of experience with PD.
METHODS
From March 2003 to November 2015, 183 patients underwent PD at Seoul Metropolitan Government - Seoul National University Boramae Medical Center.. Retrospectively collected data were analyzed, with a particular focus on complications. Hospital costs were analyzed and compared with a national database, with patients divided into 2 groups on the basis of medical insurance status.
RESULTS
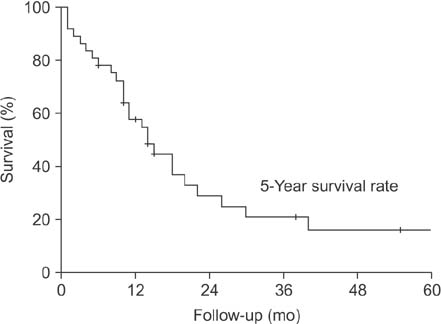
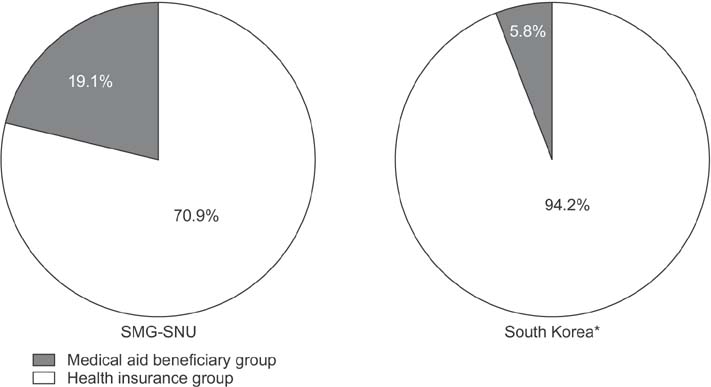
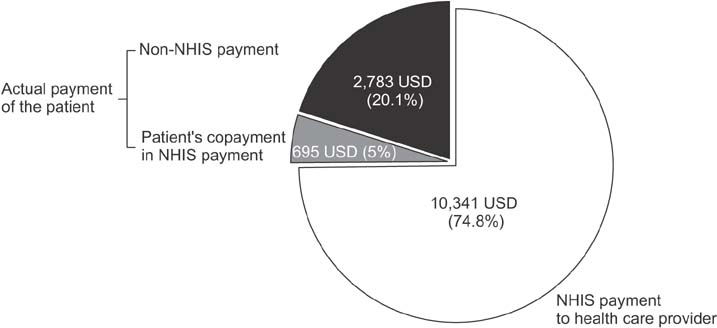
The percentage of medical aid was significantly higher than the average in Korean hospitals. (19.1% vs. 5.8%, P = 0.002). Complications occurred in 88 patients (44.3%). Postoperative pancreatic fistula (POPF) occurred in 113 cases (61.7%), but the clinically relevant POPF was 24.6% (grade B: 23.5% and grade C: 1.1%). The median hospital stay after surgery was 20 days (range, 6-137 days). In-hospital mortality was 3.8% (n = 7), with pulmonary complications being the leading cause. During the study period, improvements were observed in POPF rate, operation time, and hospital stay. The mean total hospital cost was 13,819 United States dollar (USD) per patient, and the mean reimbursement from the National Health Insurance Service (NHIS) to health care providers was 10,341 USD (74.8%). The patient copayment portion of the NHIS payment was 5%.
CONCLUSION
Performing PD in a mid-volume municipal hospital is feasible, with comparable results and cost-effectiveness.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
One hundred sixty pancreaticoduodenectomies for periampullary cancers in a growing-volume setting: a single-institution and a single-surgeon's experience
Seong-Hwan Chang
Ann Surg Treat Res. 2019;97(3):130-135. doi: 10.4174/astr.2019.97.3.130.
Reference
-
1. Kim CG, Jo S, Kim JS. Impact of surgical volume on nationwide hospital mortality after pancreaticoduodenectomy. World J Gastroenterol. 2012; 18:4175–4181.2. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.3. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.4. Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007; 142:761–768.5. Moon HJ, Jang KT, Heo JS, Choi SH, Joh JW, Kim YI. A result of surgical treatment for ductal adenocarcinoma of the head of the pancreas. Korean J Gastroenterol. 2003; 42:156–163.6. Lee KB, Min BW, Song TJ, Suh SO, Kim YC, Choi SY. Prognosis for periampullary cancers after pancreaticoduodenectomy. J Korean Surg Soc. 2003; 64:236–242.7. Cho JY, Han HS, Yoon YS, Hwang DW, Jung K, Kim YK. Postoperative complications influence prognosis and recurrence patterns in periampullary cancer. World J Surg. 2013; 37:2234–2241.8. Hoem D, Viste A. Improving survival following surgery for pancreatic ductal adenocarcinoma-- a ten-year experience. Eur J Surg Oncol. 2012; 38:245–251.9. Chamberlain RS, Gupta C, Paragi P. In defense of the whipple: an argument for aggressive surgical management of pancreatic cancer. Oncologist. 2009; 14:586–590.10. Brown EG, Yang A, Canter RJ, Bold RJ. Outcomes of pancreaticoduodenectomy: where should we focus our efforts on improving outcomes? JAMA Surg. 2014; 149:694–699.11. Aziz AM, Abbas A, Gad H, Al-Saif OH, Leung K, Meshikhes AW. Pancreaticoduodenectomy in a tertiary referral center in Saudi Arabia: a retrospective case series. J Egypt Natl Canc Inst. 2012; 24:47–54.12. Yoshioka R, Yasunaga H, Hasegawa K, Horiguchi H, Fushimi K, Aoki T, et al. Impact of hospital volume on hospital mortality, length of stay and total costs after pancreaticoduodenectomy. Br J Surg. 2014; 101:523–529.13. Kim WS, Choi DW, Choi SH, Heo JS, Kim MJ, Song SC, et al. Clinical validation of the ISGPF classification and the risk factors of pancreatic fistula formation following duct-to-mucosa pancreaticojejunostomy by one surgeon at a single center. J Gastrointest Surg. 2011; 15:2187–2192.14. Topal B, Van de Sande S, Fieuws S, Penninckx F. Effect of centralization of pancreaticoduodenectomy on nationwide hospital mortality and length of stay. Br J Surg. 2007; 94:1377–1381.15. Teh SH, Diggs BS, Deveney CW, Sheppard BC. Patient and hospital characteristics on the variance of perioperative outcomes for pancreatic resection in the United States: a plea for outcome-based and not volume-based referral guidelines. Arch Surg. 2009; 144:713–721.16. Park JS, Hwang HK, Kim JK, Cho SI, Yoon DS, Lee WJ, et al. Clinical validation and risk factors for delayed gastric emptying based on the International Study Group of Pancreatic Surgery (ISGPS) Classification. Surgery. 2009; 146:882–887.17. Enomoto LM, Gusani NJ, Dillon PW, Hollenbeak CS. Impact of surgeon and hospital volume on mortality, length of stay, and cost of pancreaticoduodenectomy. J Gastrointest Surg. 2014; 18:690–700.18. Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006; 244:10–15.19. Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002; 346:1128–1137.20. Fong Y, Gonen M, Rubin D, Radzyner M, Brennan MF. Long-term survival is superior after resection for cancer in high-volume centers. Ann Surg. 2005; 242:540–544.21. Al-Refaie WB, Muluneh B, Zhong W, Parsons HM, Tuttle TM, Vickers SM, et al. Who receives their complex cancer surgery at low-volume hospitals? J Am Coll Surg. 2012; 214:81–87.22. Afsari A, Zhandoug Z, Young S, Ferguson L, Silapaswan S, Mittal V. Outcome analysis of pancreaticoduodenectomy at a community hospital. Am Surg. 2002; 68:281–284.23. Schell MT, Barcia A, Spitzer AL, Harris HW. Pancreaticoduodenectomy: volume is not associated with outcome within an academic health care system. HPB Surg. 2008; 2008:825940.24. Akhtar K, Perricone VV, Chang D, Watson RJ. Experience of pancreaticoduodenectomy in a district general hospital. Br J Surg. 2000; 87:362–373.25. Chamberlain RS, Tichauer M, Klaassen Z, Paragi PR. Complex pancreatic surgery: safety and feasibility in the community setting. J Gastrointest Surg. 2011; 15:184–190.26. Kanhere HA, Trochsler MI, Kanhere MH, Lord AN, Maddern GJ. Pancreaticoduodenectomy: outcomes in a low-volume, specialised Hepato Pancreato Biliary unit. World J Surg. 2014; 38:1484–1490.27. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003; 349:2117–2127.28. Eppsteiner RW, Csikesz NG, McPhee JT, Tseng JF, Shah SA. Surgeon volume impacts hospital mortality for pancreatic resection. Ann Surg. 2009; 249:635–640.29. Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001; 130:415–422.30. van Heek NT, Kuhlmann KF, Scholten RJ, de Castro SM, Busch OR, van Gulik TM, et al. Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg. 2005; 242:781–788.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A modified single jejunal loop reconstruction by performing proximal gastrojejunostomy after Whipple's pancreticoduodenectomy in a low-volume hospital
- One hundred sixty pancreaticoduodenectomies for periampullary cancers in a growing-volume setting: a single-institution and a single-surgeon's experience
- The Complication Rate according to the Method of Pancreaticojejunostomy after Pancreaticoduodenectomy
- Laparoscopic pancreaticoduodenectomy with excision of aberrant right hepatic artery after preoperative segmental embolization in mid-bile duct cancer
- Technical knacks and outcomes of extended extrahepatic bile duct resection in patients with mid bile duct cancer