Cancer Res Treat.
2017 Jan;49(1):92-103. 10.4143/crt.2015.476.
Comparison of Total Body Irradiation (TBI) Conditioning with Non-TBI for Autologous Stem Cell Transplantation in Newly Diagnosed or Relapsed Mature T- and NK-Cell Non-Hodgkin Lymphoma
- Affiliations
-
- 1Division of Hemato-Oncology, Department of Internal Medicine, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Laboratory Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 5Department of Nuclear Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 6Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kstwoh@skku.edu
- 7Department of Health Sciences and Technology, SAIHST, Sungkyunkwan University, Seoul, Korea.
- KMID: 2367507
- DOI: http://doi.org/10.4143/crt.2015.476
Abstract
- PURPOSE
This retrospective study was conducted for comparison of survival outcomes and toxicities of autologous stem cell transplantation (ASCT) based on the use of total body irradiation (TBI) as a part of the conditioning regimen in patients with mature T- and natural killer (NK)-cell lymphomas.
MATERIALS AND METHODS
Patients who underwent ASCT in the upfront or salvage setting between January 2000 and December 2013 were analyzed. Patients were dichotomized according to the TBI group (n=38) and non-TBI group (n=60) based on the type of conditioning regimen for ASCT.
RESULTS
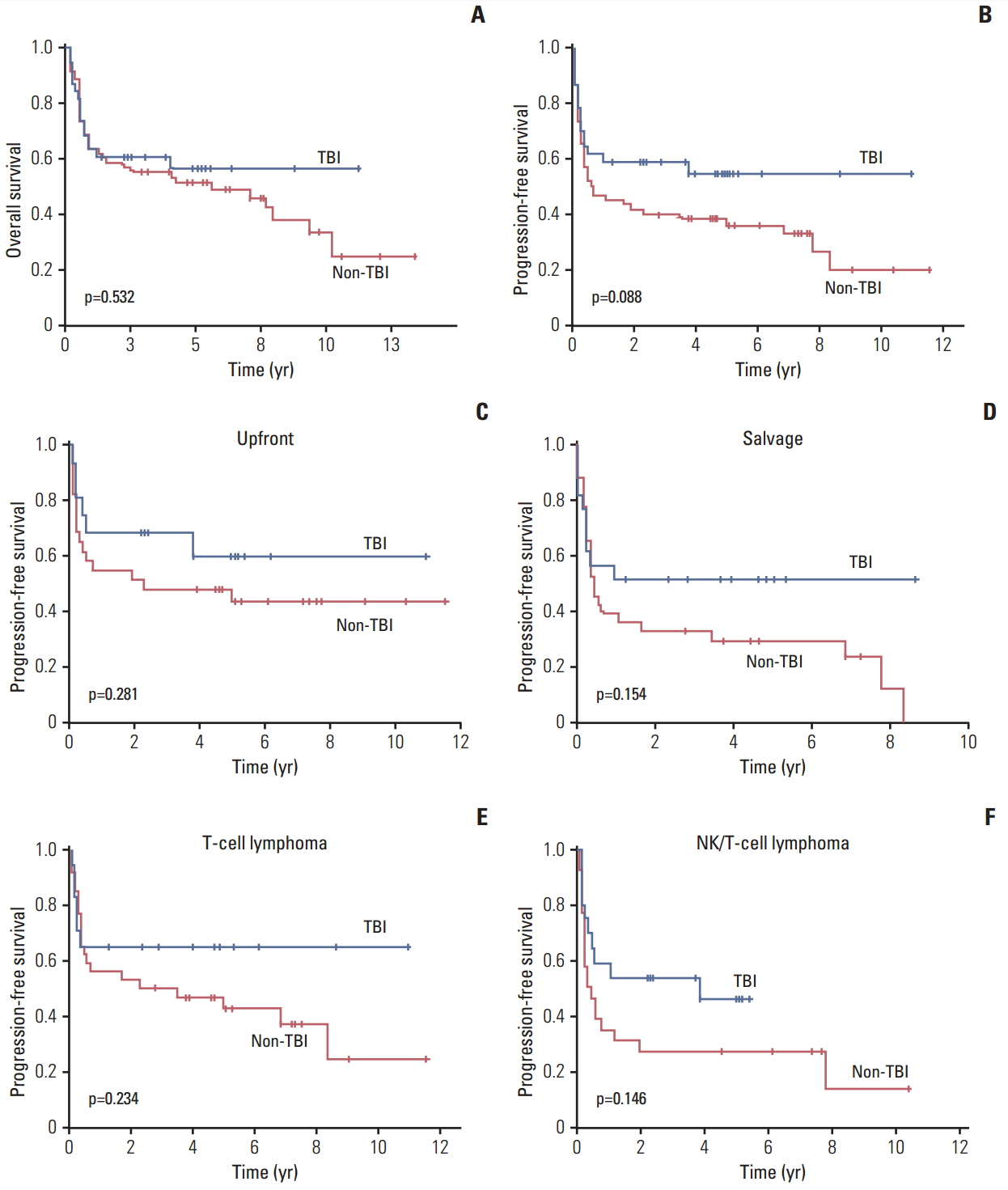
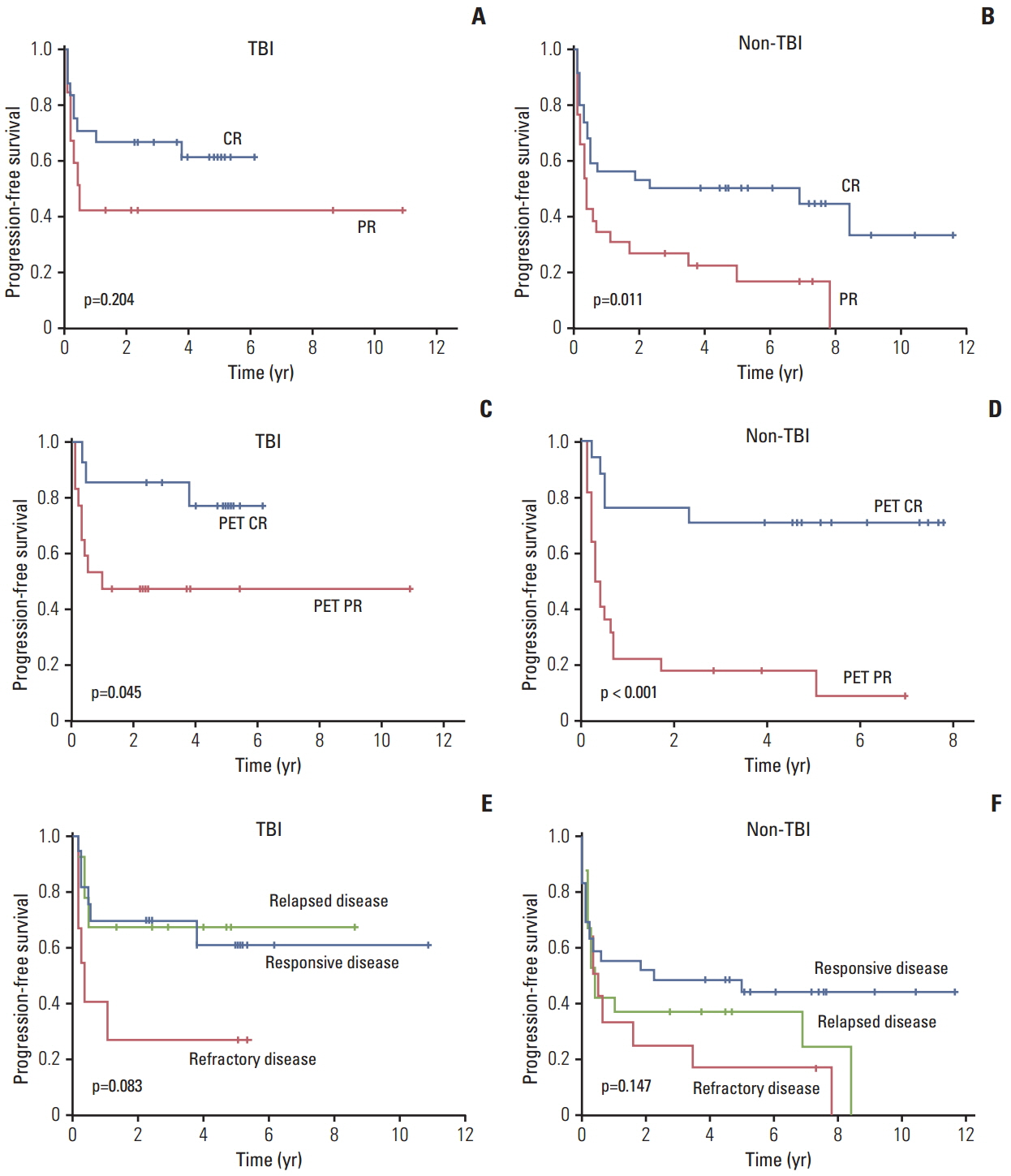
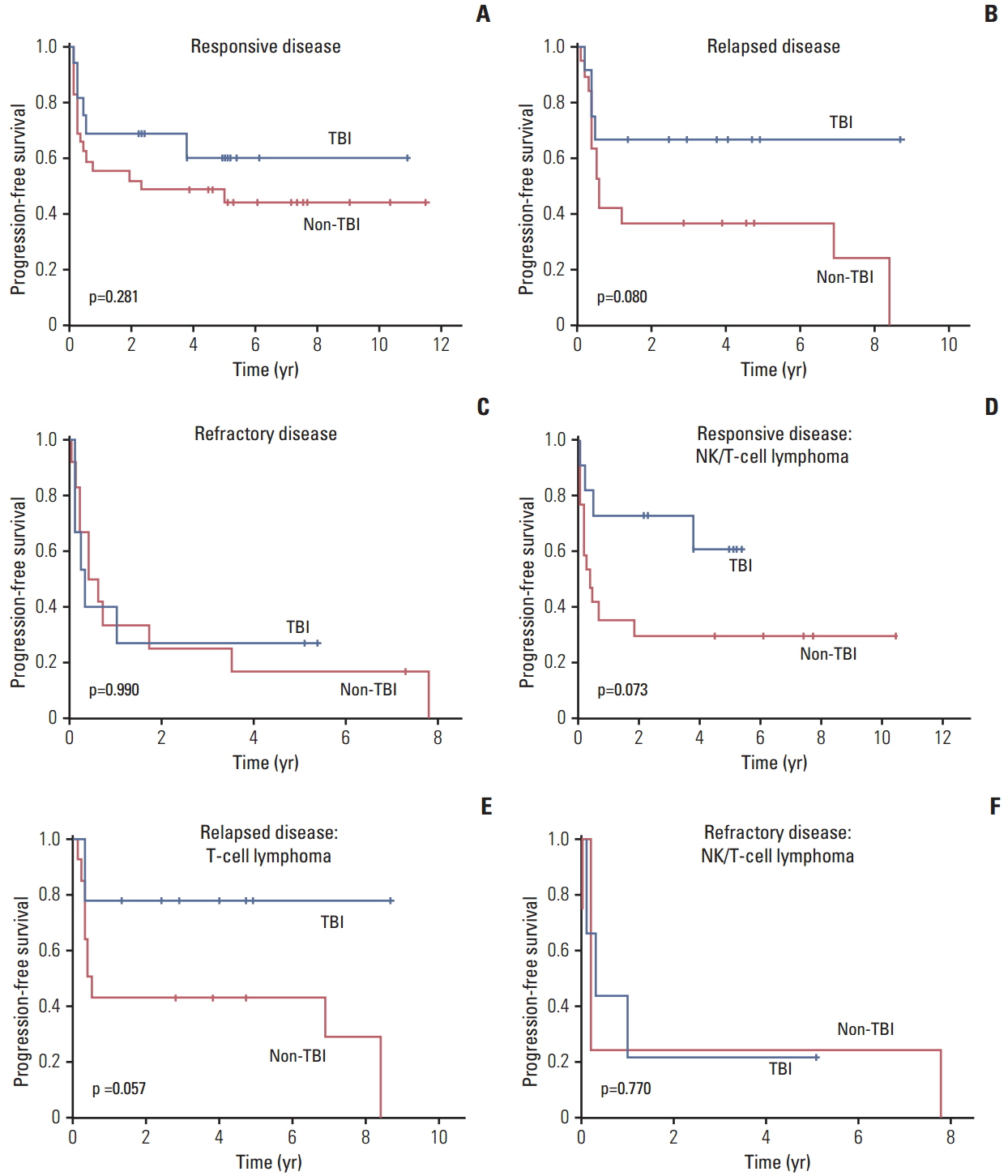
Patients with responsive disease underwent upfront ASCT (TBI, n=16; non-TBI, n=29) whereas patients with refractory disease (TBI, n=9; non-TBI, n=12) or relapsed disease (TBI, n=13; non-TBI, n=19) underwent ASCT after salvage treatment. Hematologic and non-hematologic toxicities were manageable, and the median cumulative toxicity score according to Seattle criteria was estimated as 2 (range, 0 to 7) in both groups. No significant difference in 100-day mortality was observed between the TBI (13%, 5/38) and non-TBI (12%, 12/60) groups, and most deaths were related to disease progression. There was no difference in overall and progression-free survival; however, the TBI group showed a trend of better survival in upfront and salvage ASCT than the non-TBI group. However, patients with refractory disease showed the worst outcome regardless of the use of TBI. Patients who showed complete response before ASCT showed better progression-free survival than thosewho showed partial response.
CONCLUSION
TBI could be used as an effective part of conditioning for ASCT in patients with mature T- and NK-cell lymphomas.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Philip T, Guglielmi C, Hagenbeek A, Somers R, Van der Lelie H, Bron D, et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin's lymphoma. N Engl J Med. 1995; 333:1540–5.
Article2. Rudiger T, Weisenburger DD, Anderson JR, Armitage JO, Diebold J, MacLennan KA, et al. Peripheral T-cell lymphoma (excluding anaplastic large-cell lymphoma): results from the Non-Hodgkin's Lymphoma Classification Project. Ann Oncol. 2002; 13:140–9.3. A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. The Non-Hodgkin's Lymphoma Classification Project. Blood. 1997; 89:3909–18.4. d'Amore F, Relander T, Lauritzsen GF, Jantunen E, Hagberg H, Anderson H, et al. Up-front autologous stem-cell transplantation in peripheral T-cell lymphoma: NLG-T-01. J Clin Oncol. 2012; 30:3093–9.5. Foss FM. Treatment strategies for peripheral T-cell lymphomas. Best Pract Res Clin Haematol. 2013; 26:43–56.
Article6. Jantunen E, Wiklund T, Juvonen E, Putkonen M, Lehtinen T, Kuittinen O, et al. Autologous stem cell transplantation in adult patients with peripheral T-cell lymphoma: a nation-wide survey. Bone Marrow Transplant. 2004; 33:405–10.
Article7. Yang P. TEST: a public health and law enforcement collaboration to increase HIV/AIDS prevention in Westchester County, New York. J Public Health Manag Pract. 2009; 15:118–22.8. Feyler S, Prince HM, Pearce R, Towlson K, Nivison-Smith I, Schey S, et al. The role of high-dose therapy and stem cell rescue in the management of T-cell malignant lymphomas: a BSBMT and ABMTRR study. Bone Marrow Transplant. 2007; 40:443–50.
Article9. Reimer P, Rudiger T, Geissinger E, Weissinger F, Nerl C, Schmitz N, et al. Autologous stem-cell transplantation as first-line therapy in peripheral T-cell lymphomas: results of a prospective multicenter study. J Clin Oncol. 2009; 27:106–13.
Article10. Yhim HY, Kim JS, Mun YC, Moon JH, Chae YS, Park Y, et al. Clinical outcomes and prognostic factors of up-front autologous stem cell transplantation in patients with extranodal natural killer/T cell lymphoma. Biol Blood Marrow Transplant. 2015; 21:1597–604.
Article11. Yin J, Wei J, Xu JH, Xiao Y, Zhang YC. Autologous stem cell transplantation as the first-line treatment for peripheral T cell lymphoma: results of a comprehensive meta-analysis. Acta Haematol. 2014; 131:114–25.
Article12. Gkotzamanidou M, Papadimitriou CA. Peripheral T-cell lymphoma: the role of hematopoietic stem cell transplantation. Crit Rev Oncol Hematol. 2014; 89:248–61.
Article13. Shustov A. Controversies in autologous and allogeneic hematopoietic cell transplantation in peripheral T/NK-cell lymphomas. Best Pract Res Clin Haematol. 2013; 26:89–99.
Article14. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press;2008.15. Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, et al. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored International Working Group. J Clin Oncol. 1999; 17:1244.16. Moon SH, Cho SK, Kim WS, Kim SJ, Ahn YC, Choe YS, et al. The role of 18F-FDG PET/CT for initial staging of nasal type natural killer/T-cell lymphoma: a comparison with conventional staging methods. J Nucl Med. 2013; 54:1039–44.
Article17. Bearman SI, Appelbaum FR, Buckner CD, Petersen FB, Fisher LD, Clift RA, et al. Regimen-related toxicity in patients undergoing bone marrow transplantation. J Clin Oncol. 1988; 6:1562–8.
Article18. Beitinjaneh A, Saliba RM, Medeiros LJ, Turturro F, Rondon G, Korbling M, et al. Comparison of survival in patients with T cell lymphoma after autologous and allogeneic stem cell transplantation as a frontline strategy or in relapsed disease. Biol Blood Marrow Transplant. 2015; 21:855–9.
Article19. Ellin F, Landstrom J, Jerkeman M, Relander T. Real-world data on prognostic factors and treatment in peripheral T-cell lymphomas: a study from the Swedish Lymphoma Registry. Blood. 2014; 124:1570–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Myeloablative Hematopoietic Stem Cell Transplantation with a Non-total Body Irradiation Regimen for Treating Pediatric Acute Lymphoblastic Leukemia
- Comparison of total body irradiation-based or non-total body irradiation-based conditioning regimens for allogeneic stem cell transplantation in pediatric leukemia patients
- Current Use of Total Body Irradiation in Haploidentical Allogeneic Hematopoietic Stem Cell Transplantation
- Effects of total body irradiation-based conditioning on allogeneic stem cell transplantation for pediatric acute leukemia: a single-institution study
- Autologous Stem Cell Transplantation using a Modified TAM Conditioning Regimen for Clinically Aggressive Non-Hodgkin's Lymphoma