Cancer Res Treat.
2017 Jan;49(1):54-60. 10.4143/crt.2016.045.
Estimation of the Incidence of Hepatocellular Carcinoma and Cholangiocarcinoma in Songkhla, Thailand, 1989-2013, Using Multiple Imputation Method
- Affiliations
-
- 1Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Hat Yai, Thailand. hutcha.s@psu.ac.th
- 2Department of Disease Control, Ministry of Public Health, Bangkok, Thailand.
- 3Thailand MOPH - U.S. CDC Collaboration (TUC), Ministry of Public Health, Nonthaburi, Thailand.
- KMID: 2367503
- DOI: http://doi.org/10.4143/crt.2016.045
Abstract
- PURPOSE
Histological specimens are not required for diagnosis of liver and bile duct (LBD) cancer, resulting in a high percentage of unknown histologies. We compared estimates of hepatocellular carcinoma (HCC) and cholangiocarcinoma (CCA) incidences by imputing these unknown histologies.
MATERIALS AND METHODS
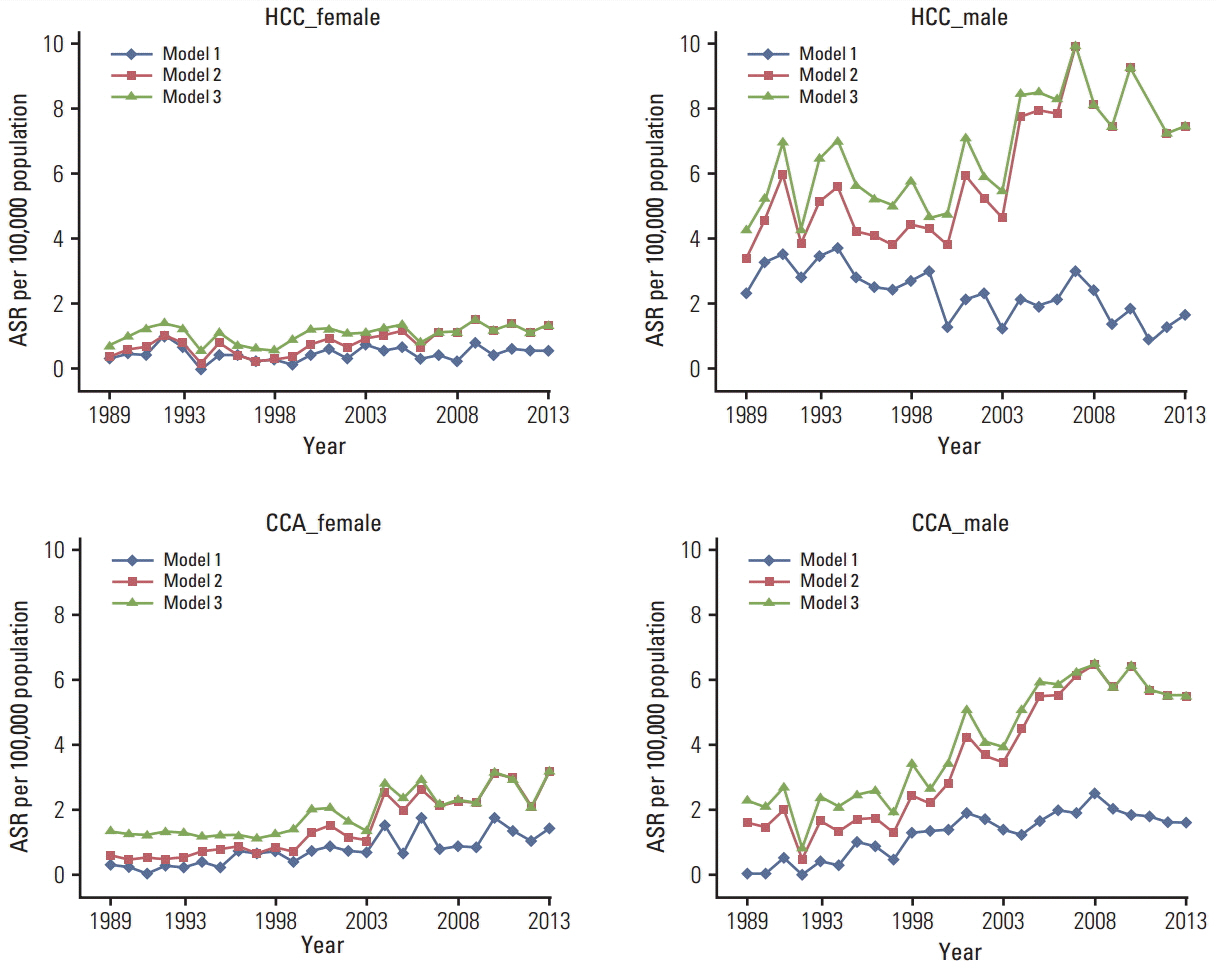
A retrospective study was conducted using data from the Songkhla Cancer Registry, southern Thailand, from 1989 to 2013. Multivariate imputation by chained equations (mice) was used in re-classification of the unknown histologies. Age-standardized rates (ASR) of HCC and CCA by sex were calculated and the trends were compared.
RESULTS
Of 2,387 LBD cases, 61% had unknown histology. After imputation, the ASR of HCC in males during 1989 to 2007 increased from 4 to 10 per 100,000 and then decreased after 2007. The ASR of CCA increased from 2 to 5.5 per 100,000, and the ASR of HCC in females decreased from 1.5 in 2009 to 1.3 in 2013 and that of CCA increased from less than 1 to 1.9 per 100,000 by 2013. Results of complete case analysis showed somewhat similar, although less dramatic, trends.
CONCLUSION
In Songkhla, the incidence of CCA appears to be stable after increasing for 20 years whereas the incidence of HCC is now declining. The decline in incidence of HCC among males since 2007 is probably due to implementation of the hepatitis B virus vaccine in the 1990s. The rise in incidence of CCA is a concern and highlights the need for case control studies to elucidate the risk factors.
MeSH Terms
Figure
Reference
-
References
1. Srivatanakul P, Sriplung H, Deerasamee S. Epidemiology of liver cancer: an overview. Asian Pac J Cancer Prev. 2004; 5:118–25.2. Hung GY, Horng JL, Yen HJ, Lee CY, Lin LY. Changing incidence patterns of hepatocellular carcinoma among age groups in Taiwan. J Hepatol. 2015; 63:1390–6.
Article3. Altekruse SF, Petrick JL, Rolin AI, Cuccinelli JE, Zou Z, Tatalovich Z, et al. Geographic variation of intrahepatic cholangiocarcinoma, extrahepatic cholangiocarcinoma, and hepatocellular carcinoma in the United States. PLoS One. 2015; 10:e0120574.
Article4. Luke C, Price T, Roder D. Epidemiology of cancer of the liver and intrahepatic bile ducts in an Australian population. Asian Pac J Cancer Prev. 2010; 11:1479–85.5. Ghouri YA, Mian I, Blechacz B. Cancer review: cholangiocarcinoma. J Carcinog. 2015; 14:1.
Article6. Cardinale V, Semeraro R, Torrice A, Gatto M, Napoli C, Bragazzi MC, et al. Intra-hepatic and extra-hepatic cholangiocarcinoma: New insight into epidemiology and risk factors. World J Gastrointest Oncol. 2010; 2:407–16.
Article7. Khuhaprema T, Attasara P, Sriplung H, Wiangnon S, Sumitsawan Y, Sangrajrang S. Cancer in Thailand Vol. VI, 2004-2006. Bangkok: National Cancer Institute;2012.8. Khuhaprema T, Attasara P, Sriplung H, Wiangnon S, Sangrajrang S. Cancer in Thailand Vol VII, 2007-2009. Bangkok: National Cancer Institute;2013.9. Sithithaworn P, Yongvanit P, Duenngai K, Kiatsopit N, Pairojkul C. Roles of liver fluke infection as risk factor for cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2014; 21:301–8.
Article10. Song HN, Go SI, Lee WS, Kim Y, Choi HJ, Lee US, et al. Population-based regional cancer incidence in Korea: comparison between urban and rural areas. Cancer Res Treat. 2016; 48:789–97.
Article11. Wiangnon S, Kamsa-ard S, Suwanrungruang K, Promthet S, Kamsa-ard S, Mahaweerawat S, et al. Trends in incidence of hepatocellular carcinoma, 1990-2009, Khon Kaen, Thailand. Asian Pac J Cancer Prev. 2012; 13:1065–8.12. Kamsa-ard S, Wiangnon S, Suwanrungruang K, Promthet S, Khuntikeo N, Kamsa-ard S, et al. Trends in liver cancer incidence between 1985 and 2009, Khon Kaen, Thailand: cholangiocarcinoma. Asian Pac J Cancer Prev. 2011; 12:2209–13.13. Van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011; 45:1–67.14. White IR, Daniel R, Royston P. Avoiding bias due to perfect prediction in multiple imputation of incomplete categorical variables. Comput Stat Data Anal. 2010; 54:2267–75.
Article15. He Y, Yucel R, Zaslavsky AM. Misreporting, missing data, and multiple imputation: improving accuracy of cancer registry databases. Chance (N Y). 2008; 21:55–8.16. Forman D, Bray F, Brewster DH, Gombe Mbalawa C, Kohler B, Pineros M, et al. Cancer incidence in five continents. Vol. X. IARC Scientific Publications No. 164. Lyon: International Agency for Research on Cancer;2014.17. Population Projection Working Group; Office of the National Economic and Social Development Board. Population projections for Thailand 2010-2040. Bangkok: Office of the National Economic and Social Development Board;2013.18. R Core Team. R: A Language and Environment for Statistical Computing [Internet]. Vienna: R Foundation for Statistical Computing;2014. [cited 2014 Dec 1]. Available from: http://www.r-project.org/.19. Doll R, Payne P, Waterhouse JA. Cancer incidence in five continents, Vol. I. Geneva: Union for International Cancer Control;1966.20. Chub-uppakarn S, Panichart P, Theamboonlers A, Poovorawan Y. Impact of the hepatitis B mass vaccination program in the southern part of Thailand. Southeast Asian J Trop Med Public Health. 1998; 29:464–8.21. Chimparlee N, Oota S, Phikulsod S, Tangkijvanich P, Poovorawan Y. Hepatitis B and hepatitis C virus in Thai blood donors. Southeast Asian J Trop Med Public Health. 2011; 42:609–15.22. Cummings P. Missing data and multiple imputation. JAMA Pediatr. 2013; 167:656–61.
Article23. Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009; 338:b2393.
Article24. Barzi F, Woodward M. Imputations of missing values in practice: results from imputations of serum cholesterol in 28 cohort studies. Am J Epidemiol. 2004; 160:34–45.
Article25. Hardt J, Herke M, Brian T, Laubach W. Multiple imputation of missing data: a simulation study on a binary response. Open J Stat. 2013; 3:370–8.26. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 4th ed. Geneva: World Health Organization;2010.27. Bjerregaard JK, Mortensen MB, Pfeiffer P; Academy of Geriatric Cancer Research (AgeCare). Trends in cancer of the liver, gall bladder, bile duct, and pancreas in elderly in Denmark, 1980-2012. Acta Oncol. 2016; 55 Suppl 1:40–5.
Article28. Chhieng DC. Fine needle aspiration biopsy of liver: an update. World J Surg Oncol. 2004; 2:5.29. Jongsuksuntigul P, Imsomboon T. Opisthorchiasis control in Thailand. Acta Trop. 2003; 88:229–32.
Article30. Worasith C, Kamamia C, Yakovleva A, Duenngai K, Wangboon C, Sithithaworn J, et al. Advances in the diagnosis of human opisthorchiasis: development of Opisthorchis viverrini antigen detection in urine. PLoS Negl Trop Dis. 2015; 9:e0004157.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in incidence of uterine cancer in Songkhla, Southern Thailand
- Combined Hepatocellular-Cholangiocarcinoma: Recent Progress in Pathology and Classification
- Combined Hepatocellular-cholangiocarcinoma
- The Mixed Hepatocellular-Cholangiocarcinoma Confirmed by Liver and Neck Node Biopsy
- Synchronous Hepatocellular Carcinoma and Cholangiocarcinoma Arising in Two Different Dysplastic Nodules