J Korean Fract Soc.
2017 Jan;30(1):40-51. 10.12671/jkfs.2017.30.1.40.
Impaired Bone Healing Metabolic and Mechanical Causes
- Affiliations
-
- 1Department of Orthopedic Surgery, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu, Korea. ossoj@ynu.ac.kr
- KMID: 2367352
- DOI: http://doi.org/10.12671/jkfs.2017.30.1.40
Abstract
- Non-union is one of the most devastating complications after fracture fixation. It usually results in prolonged treatment duration and unpredictable results. We reviewed the literature to identify recent information regarding the following: risk factors of nonunion; mechanical risk factors, including fracture gap width and stability, osteonecrosis and healing mechanism, osteoporotic fracture and fixation method, the characteristics of fracture, soft tissue injury, local infection, and multiple fractures; as well as the metabolic risk factors, including age, comorbidities, smoking, alcoholism, and medications. The technique and devices for fracture treatment have been developed, and treatments of nonunion are evolving according to the enhancement of our understanding of nonunion. Clinicians should refer to the risk factors and advancements while developing a treatment plan.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Outcomes following Treatment of Geriatric Distal Femur Fractures with Analyzing Risk Factors for the Nonunion
Soo-young Jeong, Jae-Ho Lee, Ki-Chul Park
J Korean Fract Soc. 2019;32(4):188-195. doi: 10.12671/jkfs.2019.12.4.188.
Reference
-
1. Giannoudis PV, Gudipati S, Harwood P, Kanakaris NK. Long bone non-unions treated with the diamond concept: a case series of 64 patients. Injury. 2015; 46:Suppl 8. S48–S54.
Article2. Brinker MR, O'Connor DP. The biological basis for nonunions. JBJS Rev. 2016; 4:DOI: 10.2106/JBJS.RVW.15.00078.
Article3. Zura R, Mehta S, Della Rocca GJ, Steen RG. Biological risk factors for nonunion of bone fracture. JBJS Rev. 2016; 4:DOI: 10.2106/JBJS.RVW.O.00008.
Article4. Riemer BL, Butterfield SL, Burke CJ 3rd, Mathews D. Immediate plate fixation of highly comminuted femoral diaphyseal fractures in blunt polytrauma patients. Orthopedics. 1992; 15:907–916.
Article5. Tornetta P 3rd, Tiburzi D. Reamed versus nonreamed anterograde femoral nailing. J Orthop Trauma. 2000; 14:15–19.
Article6. Bishop JA, Palanca AA, Bellino MJ, Lowenberg DW. Assessment of compromised fracture healing. J Am Acad Orthop Surg. 2012; 20:273–282.
Article7. Augat P, Faschingbauer M, Seide K, et al. Biomechanical methods for the assessment of fracture repair. Injury. 2014; 45:Suppl 2. S32–S38.
Article8. Matsuyama J, Ohnishi I, Sakai R, et al. A new method for evaluation of fracture healing by echo tracking. Ultrasound Med Biol. 2008; 34:775–783.
Article9. Marsh D. Concepts of fracture union, delayed union, and nonunion. Clin Orthop Relat Res. 1998; 355 Suppl. S22–S30.
Article10. Einhorn TA. The cell and molecular biology of fracture healing. Clin Orthop Relat Res. 1998; 355 Suppl. S7–S21.
Article11. Hayda RA, Brighton CT, Esterhai JL Jr. Pathophysiology of delayed healing. Clin Orthop Relat Res. 1998; 355 Suppl. S31–S40.
Article12. Gómez-Barrena E, Rosset P, Lozano D, Stanovici J, Ermthaller C, Gerbhard F. Bone fracture healing: cell therapy in delayed unions and nonunions. Bone. 2015; 70:93–101.
Article13. Russel T. Fractures of the tibia and fibula. In : Rockwood CA, Green DP, editors. Fractures in adults. 4th ed. Philadelphia: Lippincott- Raven;1996. p. 389–394.14. Richardson JB, Cunningham JL, Goodship AE, O'Connor BT, Kenwright J. Measuring stiffness can define healing of tibial fractures. J Bone Joint Surg Br. 1994; 76:389–394.
Article15. Wade RH, Moorcroft CI, Thomas PB. Fracture stiffness as a guide to the management of tibial fractures. J Bone Joint Surg Br. 2001; 83:533–535.
Article16. Duffy P, Trask K, Hennigar A, Barron L, Leighton RK, Dunbar MJ. Assessment of fragment micromotion in distal femur fracture fixation with RSA. Clin Orthop Relat Res. 2006; 448:105–113.
Article17. Madanat R, Mäkinen TJ, Moritz N, Mattila KT, Aro HT. Accuracy and precision of radiostereometric analysis in the measurement of three-dimensional micromotion in a fracture model of the distal radius. J Orthop Res. 2005; 23:481–488.
Article18. Solomon LB, Stevenson AW, Callary SA, Sullivan TR, Howie DW, Chehade MJ. The accuracy and precision of radiostereometric analysis in monitoring tibial plateau fractures. Acta Orthop. 2010; 81:487–494.
Article19. Little DG, Ramachandran M, Schindeler A. The anabolic and catabolic responses in bone repair. J Bone Joint Surg Br. 2007; 89:425–433.
Article20. Oryan A, Monazzah S, Bigham-Sadegh A. Bone injury and fracture healing biology. Biomed Environ Sci. 2015; 28:57–71.21. Ai-Aql ZS, Alagl AS, Graves DT, Gerstenfeld LC, Einhorn TA. Molecular mechanisms controlling bone formation during fracture healing and distraction osteogenesis. J Dent Res. 2008; 87:107–118.
Article22. Poniatowski ŁA, Wojdasiewicz P, Gasik R, Szukiewicz D. Transforming growth factor Beta family: insight into the role of growth factors in regulation of fracture healing biology and potential clinical applications[Internet]. Mediators Inflamm;2015. DOI: 10.1155/2015/137823. 2015 Jan 29. Available from: www.hindawi.com/journals/mi/2015/137823/.23. Hankenson KD, Zimmerman G, Marcucio R. Biological perspectives of delayed fracture healing. Injury. 2014; 45:Suppl 2. S8–S15.
Article24. Brinker MR, Bailey DE Jr. Fracture healing in tibia fractures with an associated vascular injury. J Trauma. 1997; 42:11–19.
Article25. Lu C, Miclau T, Hu D, Marcucio RS. Ischemia leads to delayed union during fracture healing: a mouse model. J Orthop Res. 2007; 25:51–61.
Article26. Dishowitz MI, Mutyaba PL, Takacs JD, et al. Systemic inhibition of canonical Notch signaling results in sustained callus inflammation and alters multiple phases of fracture healing. PLoS One. 2013; 8:e68726.
Article27. Alexander KA, Chang MK, Maylin ER, et al. Osteal macrophages promote in vivo intramembranous bone healing in a mouse tibial injury model. J Bone Miner Res. 2011; 26:1517–1532.
Article28. Xing Z, Lu C, Hu D, et al. Multiple roles for CCR2 during fracture healing. Dis Model Mech. 2010; 3:451–458.
Article29. Marsell R, Einhorn TA. The biology of fracture healing. Injury. 2011; 42:551–555.
Article30. Merceron C, Vinatier C, Portron S, et al. Differential effects of hypoxia on osteochondrogenic potential of human adiposederived stem cells. . Am J Physiol Cell Physiol. 2010; 298:C355–C364.
Article31. Amarilio R, Viukov SV, Sharir A, Eshkar-Oren I, Johnson RS, Zelzer E. HIF1α regulation of Sox9 is necessary to maintain differentiation of hypoxic prechondrogenic cells during early skeletogenesis. Development. 2007; 134:3917–3928.
Article32. Wagegg M, Gaber T, Lohanatha FL, et al. Hypoxia promotes osteogenesis but suppresses adipogenesis of human mesenchymal stromal cells in a hypoxia-inducible factor-1 dependent manner. PLoS One. 2012; 7:e46483.
Article33. D'Ippolito G, Diabira S, Howard GA, Roos BA, Schiller PC. Low oxygen tension inhibits osteogenic differentiation and enhances stemness of human MIAMI cells. Bone. 2006; 39:513–522.34. Riddle RC, Khatri R, Schipani E, Clemens TL. Role of hypoxiainducible factor-1alpha in angiogenic-osteogenic coupling. J Mol Med (Berl). 2009; 87:583–590.35. Kumagai K, Vasanji A, Drazba JA, Butler RS, Muschler GF. Circulating cells with osteogenic potential are physiologically mobilized into the fracture healing site in the parabiotic mice model. J Orthop Res. 2008; 26:165–175.
Article36. Colnot C. Skeletal cell fate decisions within periosteum and bone marrow during bone regeneration. J Bone Miner Res. 2009; 24:274–282.
Article37. Einhorn TA. The science of fracture healing. J Orthop Trauma. 2005; 19:S4–S6.
Article38. Yuasa M, Mignemi NA, Barnett JV, et al. The temporal and spatial development of vascularity in a healing displaced fracture. Bone. 2014; 67:208–221.
Article39. Kwong FN, Harris MB. Recent developments in the biology of fracture repair. J Am Acad Orthop Surg. 2008; 16:619–625.
Article40. Schwarz C, Wulsten D, Ellinghaus A, Lienau J, Willie BM, Duda GN. Mechanical load modulates the stimulatory effect of BMP2 in a rat nonunion model. Tissue Eng Part A. 2013; 19:247–254.
Article41. Thompson Z, Miclau T, Hu D, Helms JA. A model for intramembranous ossification during fracture healing. J Orthop Res. 2002; 20:1091–1098.
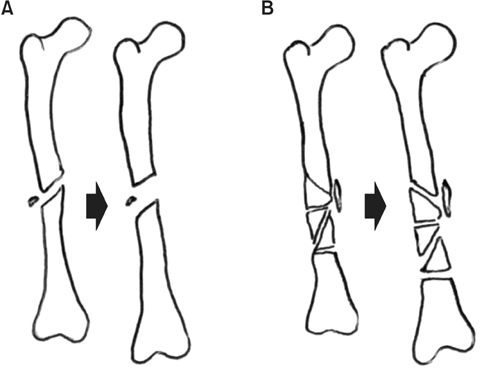
Article42. Jagodzinski M, Krettek C. Effect of mechanical stability on fracture healing: an update. Injury . 2007; 38:Suppl 1. S3–S10.43. Gaston MS, Simpson AH. Inhibition of fracture healing. J Bone Joint Surg Br. 2007; 89:1553–1560.
Article44. Hak DJ, Fitzpatrick D, Bishop JA, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury. 2014; 45:Suppl 2. S3–S7.
Article45. Aro HT, Chao EY. Bone-healing patterns affected by loading, fracture fragment stability, fracture type, and fracture site compression. Clin Orthop Relat Res. 1993; (293):8–17.
Article46. Claes L, Reusch M, Göckelmann M, et al. Metaphyseal fracture healing follows similar biomechanical rules as diaphyseal healing. J Orthop Res. 2011; 29:425–432.
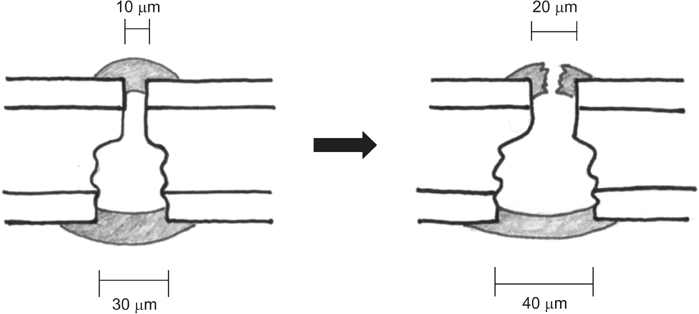
Article47. Ganz R, Perren SM, Rüter A. Mechanical induction of bone resorption. Fortschr Kiefer Gesichtschir. 1975; 19:45–48.48. Cheal EJ, Mansmann KA, DiGioia AM 3rd, Hayes WC, Perren SM. Role of interfragmentary strain in fracture healing: ovine model of a healing osteotomy. J Orthop Res. 1991; 9:131–142.
Article49. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002; 84:1093–1110.50. Claes L, Grass R, Schmickal T, et al. Monitoring and healing analysis of 100 tibial shaft fractures. Langenbecks Arch Surg. 2002; 387:146–152.
Article51. Hietaniemi K, Paavolainen P, Penttinen R. Connective tissue parameters in experimental nonunion. J Orthop Trauma. 1996; 10:114–118.
Article52. Wenda K, Runkel M, Degreif J, Rudig L. Minimally invasive plate fixation in femoral shaft fractures. Injury. 1997; 28:Suppl 1. A13–A19.
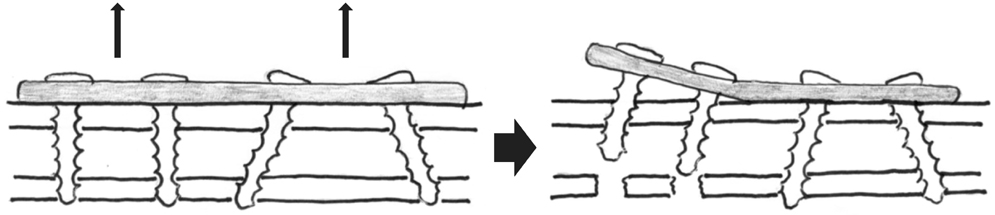
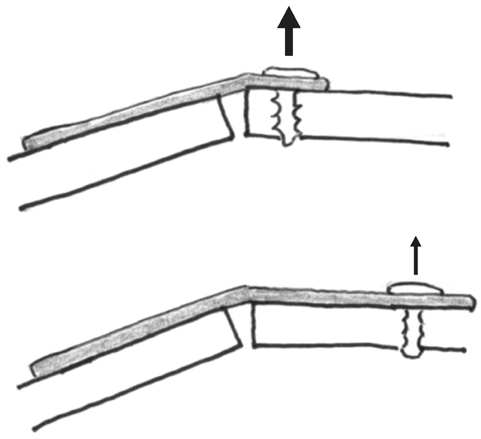
Article53. Kregor PJ, Senft D, Parvin D, et al. Cortical bone perfusion in plated fractured sheep tibiae. J Orthop Res. 1995; 13:715–724.54. Gautier E, Perren SM. Limited contact dynamic compression plate (LC-DCP): biomechanical research as basis to new plate design. Orthopade. 1992; 21:11–23.55. Kessler SB. “Spongiosation” of cortical bone. Hefte Unfallheilkd. 1983; 161:76–79.56. Chao EY, Inoue N, Koo TK, Kim YH. Biomechanical considerations of fracture treatment and bone quality maintenance in elderly patients and patients with osteoporosis. Clin Orthop Relat Res. 2004; (425):12–25.
Article57. Calori GM, Albisetti W, Agus A, Iori S, Tagliabue L. Risk factors contributing to fracture non-unions. Injury. 2007; 38:Suppl 2. S11–S18.
Article58. Ring D, Barrick WT, Jupiter JB. Recalcitrant nonunion. Clin Orthop Relat Res. 1997; (340):181–189.
Article59. Rodriguez-Merchan EC, Forriol F. Nonunion: general principles and experimental data. Clin Orthop Relat Res. 2004; (419):4–12.60. Reichert IL, McCarthy ID, Hughes SP. The acute vascular response to intramedullary reaming. Microsphere estimation of blood flow in the intact ovine tibia. J Bone Joint Surg Br. 1995; 77:490–493.
Article61. Court-Brown C, McQueen M. Compartment syndrome delays tibial union. Acta Orthop Scand. 1987; 58:249–252.
Article62. DeLee JC, Stiehl JB. Open tibia fracture with compartment syndrome. Clin Orthop Relat Res. 1981; (160):175–184.
Article63. Dickson K, Katzman S, Delgado E, Contreras D. Delayed unions and nonunions of open tibial fractures. Correlation with arteriography results. Clin Orthop Relat Res. 1994; (302):189–193.64. Concia E, De Lalla F, Di Perri G, et al. Orientamenti diagnostico-terapeutici nella gestione delle infezioni osteoarticolari. SaSaronno, Italy: Pharma Project Group s.r.l;2003.65. Meyer RA Jr, Tsahakis PJ, Martin DF, Banks DM, Harrow ME, Kiebzak GM. Age and ovariectomy impair both the normalization of mechanical properties and the accretion of mineral by the fracture callus in rats. J Orthop Res. 2001; 19:428–435.
Article66. Meyer RA Jr, Meyer MH, Tenholder M, Wondracek S, Wasserman R, Garges P. Gene expression in older rats with delayed union of femoral fractures. J Bone Joint Surg Am. 2003; 85:1243–1254.
Article67. Street JT, Wang JH, Wu QD, Wakai A, McGuinness A, Redmond HP. The angiogenic response to skeletal injury is preserved in the elderly. J Orthop Res. 2001; 19:1057–1066.
Article68. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004; 86:1359–1365.
Article69. Parker MJ. Prediction of fracture union after internal fixation of intracapsular femoral neck fractures. Injury. 1994; 25:Suppl 2. B3–B6.
Article70. Macey LR, Kana SM, Jingushi S, Terek RM, Borretos J, Bolander ME. Defects of early fracture-healing in experimental diabetes. J Bone Joint Surg Am. 1989; 71:722–733.
Article71. Jeng CL, Campbell JT, Tang EY, Cerrato RA, Myerson MS. Tibiotalocalcaneal arthrodesis with bulk femoral head allograft for salvage of large defects in the ankle. Foot Ankle Int. 2013; 34:1256–1266.
Article72. Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg. 2013; 52:207–211.
Article73. Ding YX, Hou LQ, Xiong KR. Effect of electroacupuncture on expression of proliferating cell nuclear antigen and glial fibrillary acidic protein in subventricular zone of Parkinson's disease rats. Zhen Ci Yan Jiu. 2012; 37:286–290.74. Gonzalez MH, Weinzweig N. Muscle flaps in the treatment of osteomyelitis of the lower extremity. J Trauma. 2005; 58:1019–1023.
Article75. Assiotis A, Sachinis NP, Chalidis BE. Pulsed electromagnetic fields for the treatment of tibial delayed unions and nonunions. A prospective clinical study and review of the literature. J Orthop Surg Res. 2012; 7:24.
Article76. Dodds RA, Catterall A, Bitensky L, Chayen J. Abnormalities in fracture healing induced by vitamin B6-deficiency in rats. Bone. 1986; 7:489–495.
Article77. Einhorn TA, Bonnarens F, Burstein AH. The contributions of dietary protein and mineral to the healing of experimental fractures. A biomechanical study. J Bone Joint Surg Am. 1986; 68:1389–1395.
Article78. Koval KJ, Maurer SG, Su ET, Aharonoff GB, Zuckerman JD. The effects of nutritional status on outcome after hip fracture. J Orthop Trauma. 1999; 13:164–169.
Article79. Metsemakers WJ, Roels N, Belmans A, Reynders P, Nijs S. Risk factors for nonunion after intramedullary nailing of femoral shaft fractures: Remaining controversies. Injury. 2015; 46:1601–1607.
Article80. Rodriguez EK, Boulton C, Weaver MJ, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: a retrospective multicenter case-control study of 283 fractures. Injury. 2014; 45:554–559.
Article81. Solomon DH, Hochberg MC, Mogun H, Schneeweiss S. The relation between bisphosphonate use and non-union of fractures of the humerus in older adults. Osteoporos Int. 2009; 20:895–901.
Article82. Ali AM, El-Shafie M, Willett KM. Failure of fixation of tibial plateau fractures. J Orthop Trauma. 2002; 16:323–329.
Article83. van Wunnik BP, Weijers PH, van Helden SH, Brink PR, Poeze M. Osteoporosis is not a risk factor for the development of nonunion: a cohort nested case-control study. Injury. 2011; 42:1491–1494.
Article84. Heppenstall RB, Brighton CT. Fracture healing in the presence of anemia. Clin Orthop Relat Res. 1977; (123):253–258.
Article85. Urabe K, Hotokebuchi T, Oles KJ, et al. Inhibition of endochondral ossification during fracture repair in experimental hypothyroid rats. J Orthop Res. 1999; 17:920–925.
Article86. Kyrö A, Usenius JP, Aarnio M, Kunnamo I, Avikainen V. Are smokers a risk group for delayed healing of tibial shaft fractures? Ann Chir Gynaecol. 1993; 82:254–262.87. Chakkalakal DA, Novak JR, Fritz ED, et al. Inhibition of bone repair in a rat model for chronic and excessive alcohol consumption. Alcohol. 2005; 36:201–214.
Article88. Chakkalakal DA. Alcohol-induced bone loss and deficient bone repair. Alcohol Clin Exp Res. 2005; 29:2077–2090.
Article89. Furr AM, Schweinfurth JM, May WL. Factors associated with long-term complications after repair of mandibular fractures. Laryngoscope. 2006; 116:427–430.
Article90. Duckworth AD, Bennet SJ, Aderinto J, Keating JF. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Joint Surg Br. 2011; 93:811–816.91. Foulk DA, Szabo RM. Diaphyseal humerus fractures: natural history and occurrence of nonunion. Orthopedics. 1995; 18:333–335.
Article92. Marquez-Lara A, Hutchinson ID, Nuñez F Jr, Smith TL, Miller AN. Nonsteroidal anti-inflammatory drugs and bone-healing: a systematic review of research quality. JBJS Rev. 2016; 4:DOI: 10.2106/JBJS.RVW.O.00055.
Article93. Cottrell J, O'Connor JP. Effect of non-steroidal anti-inflammatory drugs on bone healing. Pharmaceuticals (Basel). 2010; 3:1668–1693.
Article94. Warriner AH, Saag KG. Prevention and treatment of bone changes associated with exposure to glucocorticoids. Curr Osteoporos Rep. 2013; 11:341–347.
Article95. Wheelock C, Glass J, St Anna L. Clinical inquiry. Do inhaled steroids reduce bone mineral density and increase fracture risk? J Fam Pract. 2012; 61:493–508.96. Huddleston PM, Steckelberg JM, Hanssen AD, Rouse MS, Bolander ME, Patel R. Ciprofloxacin inhibition of experimental fracture healing. J Bone Joint Surg Am. 2000; 82:161–173.97. Perry AC, Prpa B, Rouse MS, et al. Levofloxacin and trovafloxacin inhibition of experimental fracture-healing. Clin Orthop Relat Res. 2003; (414):95–100.
Article98. Isefuku S, Joyner CJ, Simpson AH. Gentamicin may have an adverse effect on osteogenesis. J Orthop Trauma. 2003; 17:212–216.
Article99. Isefuku S, Joyner CJ, Simpson AH. Toxic effect of rifampicin on human osteoblast-like cells. J Orthop Res. 2001; 19:950–954.
Article100. Street JT, McGrath M, O'Regan K, Wakai A, McGuinness A, Redmond HP. Thromboprophylaxis using a low molecular weight heparin delays fracture repair. Clin Orthop Relat Res. 2000; (381):278–289.
Article101. Dalén P, Blomgren K, Bauer J. Warfarin can have a negative effect on bone formation. Lakartidningen. 1999; 96:3074.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Utility of Biochemical Marker of Bone Turnover: Fracture Risk Prediction and Bone Healing
- Current Concepts of Bone Healing
- An Assessment of the Mechanical Properties of Long Bone Fractures Using an Impulse Response Method
- Current and Future Strategies to Enhance Healing at the Tendon-To-Bone Interface of a Rotator Cuff Tear
- Basic Study on the Effect of Korean Ginseng upon Fracture Healing of the Bone