Associations among the Degree of Nonalcoholic Fatty Liver Disease, Metabolic Syndrome, Degree of Obesity in Children, and Parental Obesity
- Affiliations
-
- 1Department of Pediatrics, Jeju National University School of Medicine, Jeju, Korea. kskang@jejunu.ac.kr
- 2Department of Radiology, Jeju National University School of Medicine, Jeju, Korea.
- KMID: 2364779
- DOI: http://doi.org/10.5223/pghn.2016.19.3.199
Abstract
- PURPOSE
To analyze the associations among the degrees of nonalcoholic fatty liver disease (NAFLD) by ultrasonography and metabolic syndrome, degrees of obesity in children, and degrees of parental obesity.
METHODS
A total of 198 children with obesity who visited a pediatric obesity clinic were prospectively enrolled in this study. The severity of NAFLD based on ultrasonography was classified into no, mild, moderate, or severe NAFLD group. The degree of obesity based on the percentage over standard weight for height per sex was classified into mild, moderate, or severe.
RESULTS
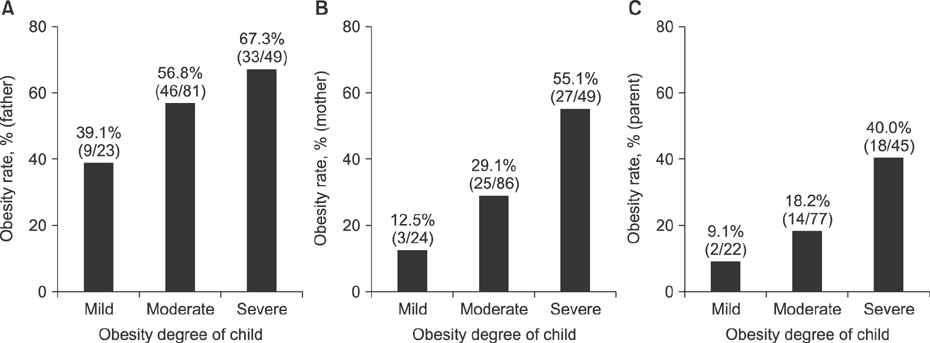
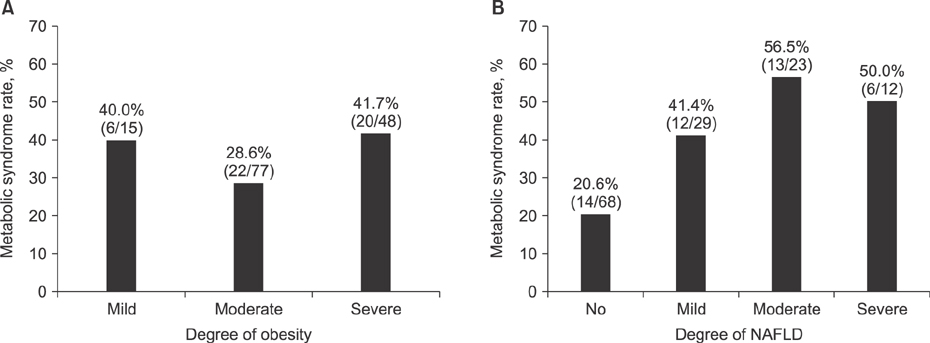
Of 132 patients evaluated for the degree of NAFLD and metabolic syndrome, the p-value of correlation between the two factors was 0.009. Therefore, metabolic syndrome might significantly affect the degree of NAFLD. Of 158 patients evaluated for the degree of NAFLD and the degree of obesity, the p-value of correlation between the two factors was 0.122. Of 154 patients evaluated for the degree of obesity and father's obesity, the p-value was 0.076. Of 159 patients evaluated for the degree of obesity and mother's obesity, the p-value was 0.000, indicating that mother's obesity could significantly affect the degree of obesity in children. Of 142 patients evaluated for the degree of obesity and metabolic syndrome, the p-value was 0.288.
CONCLUSION
Metabolic syndrome might significantly affect the degree of nonalcoholic fatty liver in children. In addition, mother's obesity might be a significant factor that affects the degree of obesity in children.
MeSH Terms
Figure
Cited by 6 articles
-
Nutritional Counseling for Obese Children with Obesity-Related Metabolic Abnormalities in Korea
Ki Soo Kang
Pediatr Gastroenterol Hepatol Nutr. 2017;20(2):71-78. doi: 10.5223/pghn.2017.20.2.71.The Analysis of Factors Causing the High Prevalence of Child Obesity in Jeju Island
Eun Hye Park, Min-Su Oh, Sorina Kim, Juyeon Lee, Ki Soo Kang
Pediatr Gastroenterol Hepatol Nutr. 2018;21(2):127-133. doi: 10.5223/pghn.2018.21.2.127.Clinical Practice Guideline for the Diagnosis and Treatment of Pediatric Obesity: Recommendations from the Committee on Pediatric Obesity of the Korean Society of Pediatric Gastroenterology Hepatology and Nutrition
Dae Yong Yi, Soon Chul Kim, Ji Hyuk Lee, Eun Hye Lee, Jae Young Kim, Yong Joo Kim, Ki Soo Kang, Jeana Hong, Jung Ok Shim, Yoon Lee, Ben Kang, Yeoun Joo Lee, Mi Jin Kim, Jin Soo Moon, Hong Koh, JeongAe You, Young-Sook Kwak, Hyunjung Lim, Hye Ran Yang
Pediatr Gastroenterol Hepatol Nutr. 2019;22(1):1-27. doi: 10.5223/pghn.2019.22.1.1.Association Between Vitamin D Deficiency and Suspected Nonalcoholic Fatty Liver Disease in an Adolescent Population
Young Hoon Cho, Ju Whi Kim, Jung Ok Shim, Hye Ran Yang, Ju Young Chang, Jin Soo Moon, Jae Sung Ko
Pediatr Gastroenterol Hepatol Nutr. 2019;22(3):233-241. doi: 10.5223/pghn.2019.22.3.233.Pathologic Impact of Insulin Resistance and Sensitivity on the Severity of Liver Histopathology in Pediatric Non-Alcoholic Steatohepatitis
Byung Han Park, Jung Min Yoon, Ja Hye Kim, Jin-Hwa Moon, Young Ho Lee, Se Min Jang, Yong Joo Kim
Yonsei Med J. 2017;58(4):756-762. doi: 10.3349/ymj.2017.58.4.756.Factors associated with Advanced Bone Age in Overweight and Obese Children
Min-Su Oh, Sorina Kim, Juyeon Lee, Mu Sook Lee, Yoon-Joo Kim, Ki-Soo Kang
Pediatr Gastroenterol Hepatol Nutr. 2020;23(1):89-97. doi: 10.5223/pghn.2020.23.1.89.
Reference
-
1. Korean Education Ministry. The results for school health examination survey 2014 [Internet]. Sejong: Korean Education Ministry;2015. cited 2015 Feb 12. Available from: http://www.moe.go.kr/web/106888/ko/board/view.do?bbsId=339&boardSeq=58466.2. Keane VA. Assessment of growth. In : Kliegman RM, Stanton BF, St Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier;2015.3. Wieckowska A, Feldstein AE. Nonalcoholic fatty liver disease in the pediatric population: a review. Curr Opin Pediatr. 2005; 17:636–641.
Article4. Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009; 58:1538–1544.
Article5. Patton HM, Sirlin C, Behling C, Middleton M, Schwimmer JB, Lavine JE. Pediatric nonalcoholic fatty liver disease: a critical appraisal of current data and implications for future research. J Pediatr Gastroenterol Nutr. 2006; 43:413–427.6. Patton HM, Yates K, Unalp-Arida A, Behling CA, Huang TT, Rosenthal P, et al. Association between metabolic syndrome and liver histology among children with nonalcoholic Fatty liver disease. Am J Gastroenterol. 2010; 105:2093–2102.
Article7. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997; 337:869–873.
Article8. Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP, Hurley M, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002; 123:745–750.
Article9. Lambert M, Paradis G, O'Loughlin J, Delvin EE, Hanley JA, Levy E. Insulin resistance syndrome in a representative sample of children and adolescents from Quebec, Canada. Int J Obes Relat Metab Disord. 2004; 28:833–841.
Article10. Yoo S, Lee SY, Kim KN, Sung E. Obesity in Korean pre-adolescent school children: comparison of various anthropometric measurements based on bioelectrical impedance analysis. Int J Obes (Lond). 2006; 30:1086–1090.
Article11. Ahn YM, Sohn M, Choi SH. Comparison in weight, height, degree of obesity and body mass index among different methods for body shape classification in school-age children. J Korean Acad Nurs. 2010; 40:775–784.
Article12. Vajro P, Lenta S, Socha P, Dhawan A, McKiernan P, Baumann U, et al. Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2012; 54:700–713.
Article13. Roldan-Valadez E, Favila R, Martínez-López M, Uribe M, Méndez-Sánchez N. Imaging techniques for assessing hepatic fat content in nonalcoholic fatty liver disease. Ann Hepatol. 2008; 7:212–220.
Article14. Nobili V, Vizzutti F, Arena U, Abraldes JG, Marra F, Pietrobattista A, et al. Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology. 2008; 48:442–448.
Article15. Joseph AE, Saverymuttu SH, al-Sam S, Cook MG, Maxwell JD. Comparison of liver histology with ultrasonography in assessing diffuse parenchymal liver disease. Clin Radiol. 1991; 43:26–31.
Article16. Park SH, Kim PN, Kim KW, Lee SW, Yoon SE, Park SW, et al. Macrovesicular hepatic steatosis in living liver donors: use of CT for quantitative and qualitative assessment. Radiology. 2006; 239:105–112.
Article17. Radetti G, Kleon W, Stuefer J, Pittschieler K. Non-alcoholic fatty liver disease in obese children evaluated by magnetic resonance imaging. Acta Paediatr. 2006; 95:833–837.
Article18. Pacifico L, Celestre M, Anania C, Paolantonio P, Chiesa C, Laghi A. MRI and ultrasound for hepatic fat quantification: relationships to clinical and metabolic characteristics of pediatric nonalcoholic fatty liver disease. Acta Paediatr. 2007; 96:542–547.
Article19. Mencin AA, Lavine JE. Nonalcoholic fatty liver disease in children. Curr Opin Clin Nutr Metab Care. 2011; 14:151–157.
Article20. Loomba R, Sirlin CB, Schwimmer JB, Lavine JE. Advances in pediatric nonalcoholic fatty liver disease. Hepatology. 2009; 50:1282–1293.
Article21. Sundaram SS, Zeitler P, Nadeau K. The metabolic syndrome and nonalcoholic fatty liver disease in children. Curr Opin Pediatr. 2009; 21:529–535.
Article22. Park SK, Ryoo JH, Choi JM, Seo MW, Park CM. The risk of abdominal obesity according to the degree of non-alcoholic fatty liver disease in Korean men. J Korean Med Sci. 2016; 31:410–416.
Article23. Etelson D, Brand DA, Patrick PA, Shirali A. Childhood obesity: do parents recognize this health risk? Obes Res. 2003; 11:1362–1368.
Article24. Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. Am J Clin Nutr. 1998; 67:1130–1135.
Article25. Chang JH, Kim DH, Kim HS, Choi IK, Cheong MY, Kim DK. Prevalence of metabolic syndrome in obese children. Korean J Pediatr. 2004; 47:1149–1156.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of the Nonalcoholic Fatty Liver Disease in Obese Children
- Gut Microbiota and Clinical Disease: Obesity and Nonalcoholic Fatty Liver Disease
- Management of Patients with Nonalcoholic Fatty Liver Disease with Lifestyle Modification
- Comorbid diseases in nonalcoholic fatty liver disease
- Clinical impact of nonalcoholic fatty liver disease on other medical diseases