Allergy Asthma Respir Dis.
2016 Mar;4(2):140-144. 10.4168/aard.2016.4.2.140.
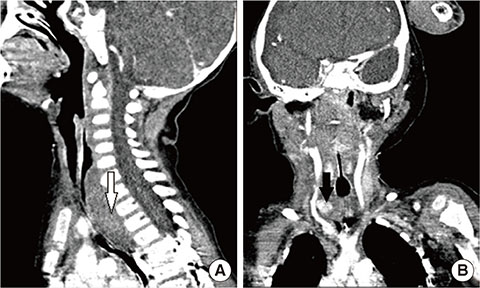
Extracorporeal membrane oxygenation treatment in peanut aspiration with complications
- Affiliations
-
- 1Department of Pediatrics, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. kwkim@yuhs.ac
- 2Institute of Allergy, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Cardiovascular Surgery, Congenital Heart Disease Center, Severance Cardiovascular Hospital, Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2361287
- DOI: http://doi.org/10.4168/aard.2016.4.2.140
Abstract
- Foreign body aspiration commonly occurs, especially among children younger than 3 years of age. Most endobronchial foreign bodies may be easily removed by bronchoscopy and have a good prognosis. Despite advances in bronchoscopic procedures, difficulties in management of and complications from foreign body aspiration are still noted. We present a foreign body aspiration case with acute respiratory distress syndrome caused aspiration pneumonia, which was successfully treated by bronchoscopy under extracorporeal membrane oxygenation (ECMO). ECMO can be an effective and potentially life-saving method in complicated foreign body aspiration with uncompensated respiratory failure.
MeSH Terms
Figure
Reference
-
1. Kiyan G, Uygun I, Karadag B, Tugtepe H, Iskit SH, Dagli TE. Foreign body aspiration in children. Kulak Burun Bogaz Ihtis Derg. 2004; 12:128–133.2. Chiu CY, Wong KS, Lai SH, Hsia SH, Wu CT. Factors predicting early diagnosis of foreign body aspiration in children. Pediatr Emerg Care. 2005; 21:161–164.3. Asif M, Shah SA, Khan F, Ghani R. Analysis of tracheobronchial foreign bodies with respect to sex, age, type and presentation. J Ayub Med Coll Abbottabad. 2007; 19:13–15.4. Dikensoy O, Usalan C, Filiz A. Foreign body aspiration: clinical utility of flexible bronchoscopy. Postgrad Med J. 2002; 78:399–403.
Article5. Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg. 2010; 111:1016–1025.
Article6. Marik PE. Pulmonary aspiration syndromes. Curr Opin Pulm Med. 2011; 17:148–154.
Article7. Eren S, Balci AE, Dikici B, Doblan M, Eren MN. Foreign body aspiration in children: experience of 1160 cases. Ann Trop Paediatr. 2003; 23:31–37.
Article8. Rovin JD, Rodgers BM. Pediatric foreign body aspiration. Pediatr Rev. 2000; 21:86–90.
Article9. Kim HY, Kong SG, Park HJ. Foreign body aspiration in children: 30-years experience in a single institution. Pediatr Allergy Respir Dis. 2009; 19:383–391.10. Son CY, Wee JO, Kim SO, Oh IJ, Park CM, Kim KS, et al. A retrospective review of tracheobronchial foreign bodies. Tuberc Respir Dis. 2005; 58:600–606.
Article11. Dalton HJ. Extracorporeal life support: moving at the speed of light. Respir Care. 2011; 56:1445–1453.
Article12. Maslach-Hubbard A, Bratton SL. Extracorporeal membrane oxygenation for pediatric respiratory failure: History, development and current status. World J Crit Care Med. 2013; 2:29–39.
Article13. Park AH, Tunkel DE, Park E, Barnhart D, Liu E, Lee J, et al. Management of complicated airway foreign body aspiration using extracorporeal membrane oxygenation (ECMO). Int J Pediatr Otorhinolaryngol. 2014; 78:2319–2321.
Article14. Shlizerman L, Mazzawi S, Rakover Y, Ashkenazi D. Foreign body aspiration in children: the effects of delayed diagnosis. Am J Otolaryngol. 2010; 31:320–324.
Article15. Skinner SC, Hirschl RB, Bartlett RH. Extracorporeal life support. Semin Pediatr Surg. 2006; 15:242–250.
Article16. Cavallone LF, Vannucci A. Review article: extubation of the difficult airway and extubation failure. Anesth Analg. 2013; 116:368–383.17. Muellenbach RM, Kredel M, Wunder C, Kustermann J, Wurmb T, Schwemmer U, et al. Arteriovenous extracorporeal lung assist as integral part of a multimodal treatment concept: a retrospective analysis of 22 patients with ARDS refractory to standard care. Eur J Anaesthesiol. 2008; 25:897–904.
Article18. Jacobs JP, Goldman AP, Cullen S, Rocco D, Samanli U, Macrae DJ, et al. Carotid artery pseudoaneurysm as a complication of ECMO. Ann Vasc Surg. 1997; 11:630–633.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extracorporeal Membrane Oxygenation Therapy for Aspiration Pneumonia in a Patient following Left Pneumonectomy for Lung Cancer
- Successful Retrieval of a Fractured Guidewire during Extracorporeal Membrane Oxygenator Insertion
- Extracorporeal Membrane Oxygenation for Complicated Scrub Typhus
- Intracranial Hemorrhage Identified in the Early Stage after Applying Extracorporeal Membrane Oxygenation to Support Cardiopulmonary Resuscitation
- Catastrophic catecholamine-induced cardiomyopathy rescued by extracorporeal membrane oxygenation in recurrent malignant pheochromocytoma