Yeungnam Univ J Med.
2019 Sep;36(3):254-259. 10.12701/yujm.2019.00213.
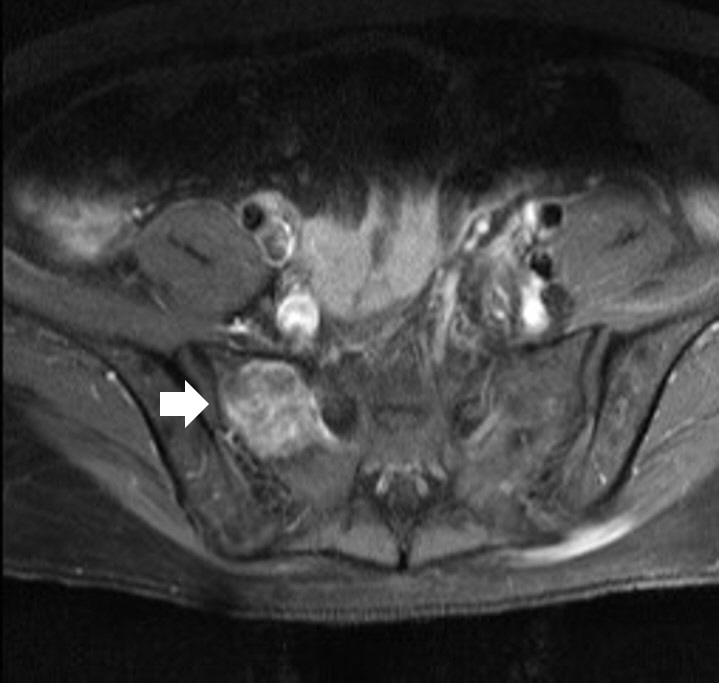
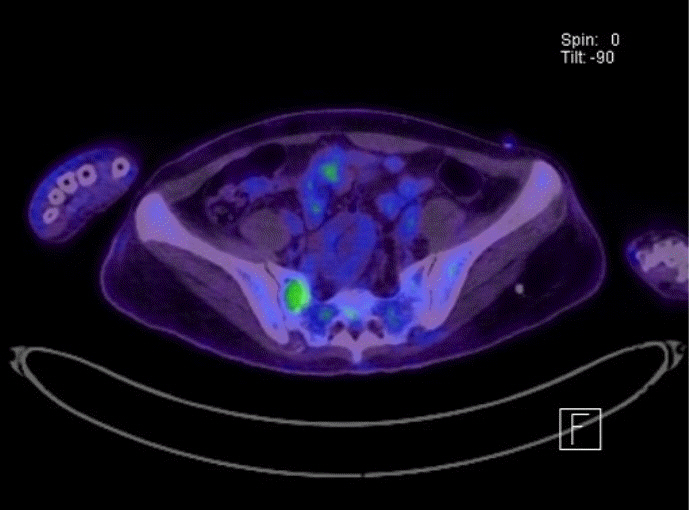
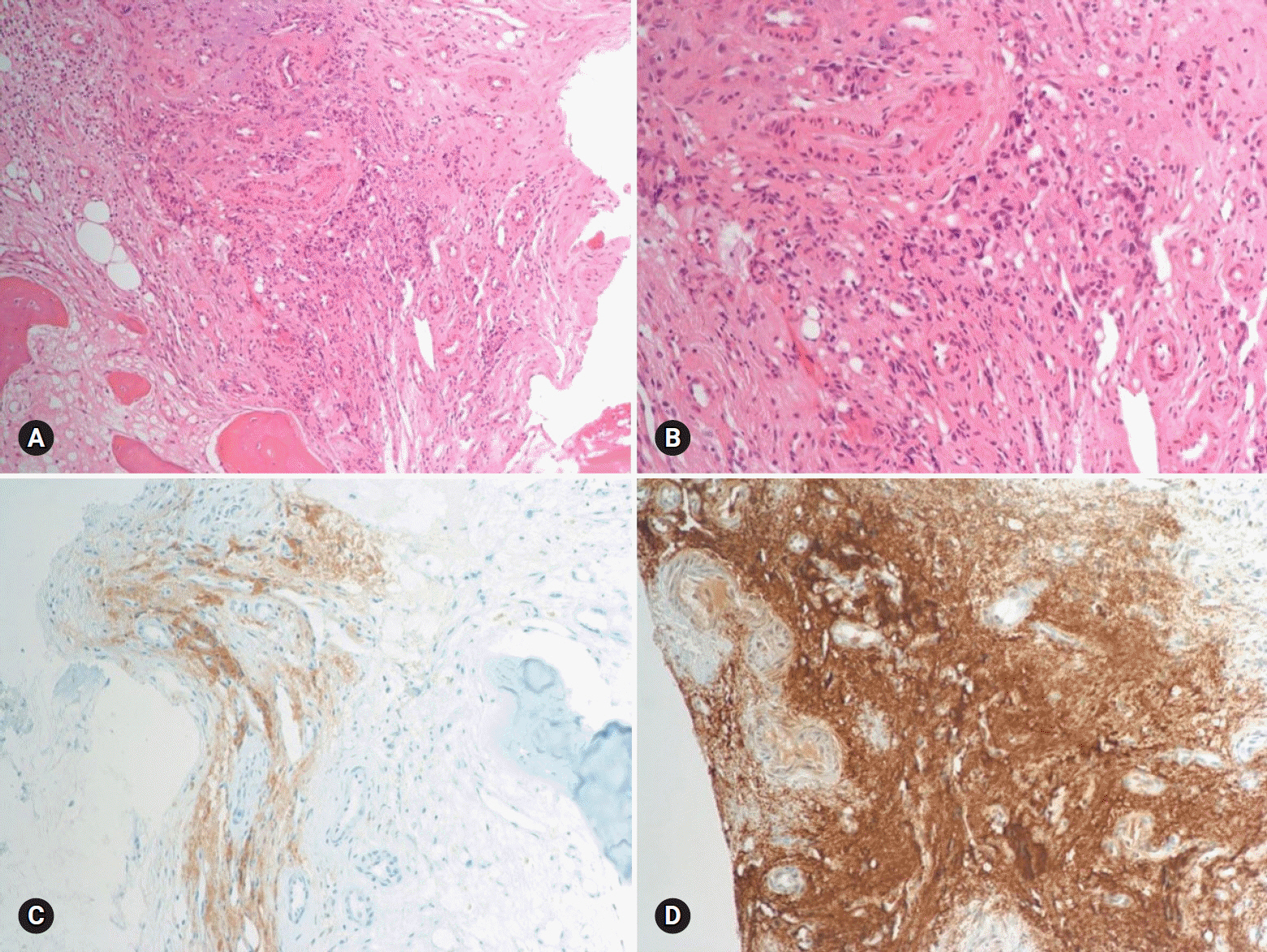
Catastrophic catecholamine-induced cardiomyopathy rescued by extracorporeal membrane oxygenation in recurrent malignant pheochromocytoma
- Affiliations
-
- 1Department of Cardiology, G SAM Hospital, Gunpo, Korea. danieruyo@gmail.com
- KMID: 2460195
- DOI: http://doi.org/10.12701/yujm.2019.00213
Abstract
- Pheochromocytoma (PCC) is a rare catecholamine-producing tumor with the incidence in hypertension of 0.1-0.6%. PCC crisis is an endocrine emergency that can lead to hemodynamic disturbance and organ failure such as catecholamine-induced cardiomyopathy. The circulatory collapse caused by it often requires mechanical support. The author reports an unusual case in which a patient who previously underwent surgery for malignant PCC developed catecholamine-induced cardiomyopathy, and successfully recovered using extracorporeal membrane oxygenation.
MeSH Terms
Figure
Reference
-
References
1. Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005; 366:665–75.
Article2. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014; 99:1915–42.
Article3. Whitelaw BC, Prague JK, Mustafa OG, Schulte KM, Hopkins PA, Gilbert JA, et al. Phaeochromocytoma crisis. Clin Endocrinol (Oxf). 2014; 80:13–22.
Article4. Prejbisz A, Lenders JW, Eisenhofer G, Januszewicz A. Cardiovascular manifestations of phaeochromocytoma. J Hypertens. 2011; 29:2049–60.
Article5. Suh IW, Lee CW, Kim YH, Hong MK, Lee JW, Kim JJ, et al. Catastrophic catecholamine-induced cardiomyopathy mimicking acute myocardial infarction, rescued by extracorporeal membrane oxygenation (ECMO) in pheochromocytoma. J Korean Med Sci. 2008; 23:350–4.
Article6. Sojod G, Diana M, Wall J, D'Agostino J, Mutter D, Marescaux J. Successful extracorporeal membrane oxygenation treatment for pheochromocytoma-induced acute cardiac failure. Am J Emerg Med. 2012; 30:1017. e1-3.
Article7. Giavarini A, Chedid A, Bobrie G, Plouin PF, Hagège A, Amar L. Acute catecholamine cardiomyopathy in patients with phaeochromocytoma or functional paraganglioma. Heart. 2013; 99:1438–44.
Article8. Otusanya O, Goraya H, Iyer P, Landi K, Tibb A, Msaouel P. A vicious cycle of acute catecholamine cardiomyopathy and circulatory collapse secondary to pheochromocytoma. Oxf Med Case Reports. 2015; 2015:343–5.
Article9. Yi DW, Kim SY, Shin DH, Kang YH, Son SM. Pheochromocytoma crisis after a dexamethasone suppression test for adrenal incidentaloma. Endocrine. 2010; 37:213–9.
Article10. An JY, Kim DR, Oh JY, Han YC, Lee IS, Kown TJ, et al. A case of recurrent glucocorticoid-induced pheochromocytoma crisis during the treatment of urticarial. Korean J Med. 2015; 88:564–9.
Article11. Barrett C, van Uum SH, Lenders JW. Risk of catecholaminergic crisis following glucocorticoid administration in patients with an adrenal mass: a literature review. Clin Endocrinol (Oxf). 2015; 83:622–8.
Article12. Tischler AS, Perlman RL, Morse GM, Sheard BE. Glucocorticoids increase catecholamine synthesis and storage in PC12 pheochromocytoma cell cultures. J Neurochem. 1983; 40:364–70.
Article13. McMahon A, Sabban EL. Regulation of expression of dopamine beta-hydroxylase in PC12 cells by glucocorticoids and cyclic AMP analogues. J Neurochem. 1992; 59:2040–7.14. Yang S, Zhang L. Glucocorticoids and vascular reactivity. Curr Vasc Pharmacol. 2004; 2:1–12.
Article15. Harari A, Inabnet WB 3rd. Malignant pheochromocytoma: a review. Am J Surg. 2011; 201:700–8.
Article16. Baudin E, Habra MA, Deschamps F, Cote G, Dumont F, Cabanillas M, et al. Therapy of endocrine disease: treatment of malignant pheochromocytoma and paraganglioma. Eur J Endocrinol. 2014; 171:R111–22.
Article17. Tanaka S, Ito T, Tomoda J, Higashi T, Yamada G, Tsuji T. Malignant pheochromocytoma with hepatic metastasis diagnosed 20 years after resection of the primary adrenal lesion. Intern Med. 1993; 32:789–94.
Article18. Ilias I, Divgi C, Pacak K. Current role of metaiodobenzylguanidine in the diagnosis of pheochromocytoma and medullary thyroid cancer. Semin Nucl Med. 2011; 41:364–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catecholamine-Induced Cardiomyopathy associated with Neuroblastoma and Treated with Extracorporeal Membrane Oxygenation as a Bridge to Recovery
- Catastrophic Catecholamine-Induced Cardiomyopathy Mimicking Acute Myocardial Infarction, Rescued by Extracorporeal Membrane Oxygenation (ECMO) in Pheochromocytoma
- A Case of Pheochromocytoma Presented with Severe Left Ventricular Dysfunction Combined with Cardiogenic Shock after Caesearian Section Delivery Responding to Treatment of Extracorporeal Membrane Oxygenation
- A case of pheochromocytoma with acute pancreatitis and catecholamine-induced cardiomyopathy
- Anesthetic experience of pheochromocytoma resection with catecholamine-induced cardiomyopathy and congestive heart failure : A case report