J Korean Med Assoc.
2016 Nov;59(11):872-880. 10.5124/jkma.2016.59.11.872.
Updated information on smoking cessation management
- Affiliations
-
- 1Department of Family Medicine, Hallym University School of Medicine, Chuncheon, Korea. paek@hallym.or.kr
- KMID: 2358435
- DOI: http://doi.org/10.5124/jkma.2016.59.11.872
Abstract
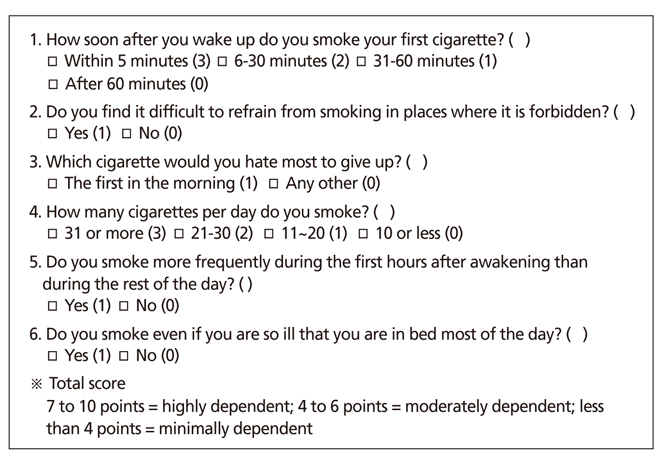
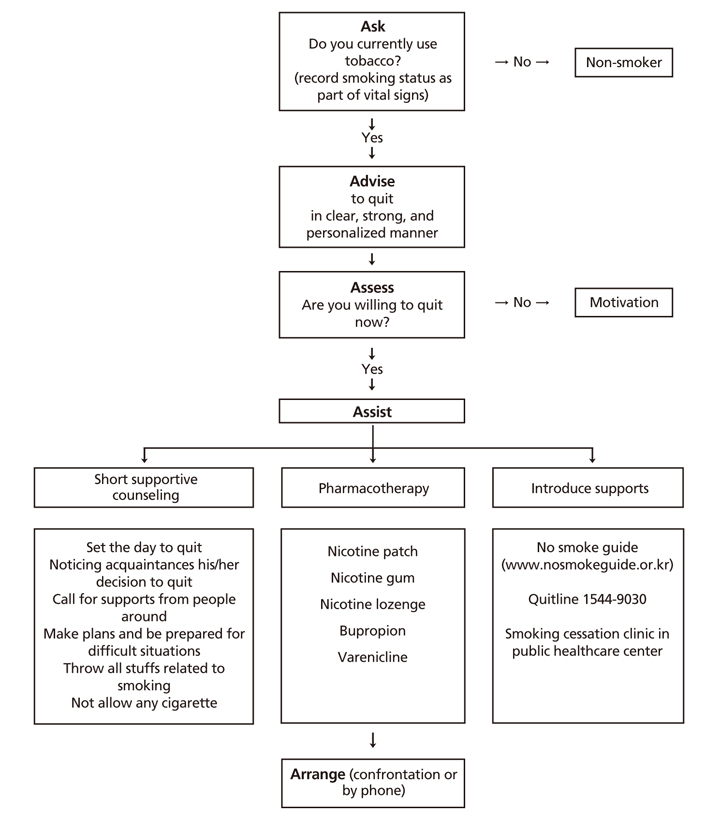
- Smoking is a leading cause of premature death, and the World Health Organization estimates 8 million deaths per year are due to smoking-related diseases. Most smokers want to quit smoking, which is not easy because of nicotine dependence. Physicians can help smokers quit smoking by assessing their dependence and motivating them on their clinic visits. Brief advices provided by doctors is a simple and very cost-effective methods of smoking cessation. The most effective method of helping smokers stop smoking is combining pharmacotherapy with advice and behavioral intervention. Sometimes, intensive counseling, either individual or group, is needed to promote smoking cessation. Health care providers also need to be familiar with pharmacotherapy. Additionally, other sources of support, such as written materials, a telephone quit-line, and strategies for preventing relapses should be integrated into the treatment. Future research could contribute to further understanding about the effects of various intensities of treatment, particular settings for treatment, or a treatment's effect among specific populations. This could include identifying the optimal amount of behavioral support to use with pharmacotherapy.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Factors Related to Smoking Relapse among Military Personnel in Korea: Data from Smoking Cessation Clinics, 2015–2017
Eunjoo Kwon, Eun-Hee Nah
Korean J Health Promot. 2018;18(3):138-146. doi: 10.15384/kjhp.2018.18.3.136.
Reference
-
1. Gellert C, Schottker B, Brenner H. Smoking and all-cause mortality in older people: systematic review and meta-analysis. Arch Intern Med. 2012; 172:837–844.2. Centers for Disease Control and Prevention (CDC). Smoking-attributable mortality, years of potential life lost, and productivity losses: United States, 2000-2004. MMWR Morb Mortal Wkly Rep. 2008; 57:1226–1228.3. Siu AL. US Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015; 163:622–634.
Article4. Rigotti NA. Strategies to help a smoker who is struggling to quit. JAMA. 2012; 308:1573–1580.
Article5. Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013; (5):CD000165.
Article6. OECD Library. OECD factbook 2013: economic, environmental and social statistics [Internet]. 2013. Paris: Organization for Economic Cooperation and Development;cited 2016 Sep 11. Available from: http://www.oecd-ilibrary.org/economics/oecd-factbook-2013_factbook-2013-en.7. Ministry of Health and Welfare, Korea Center for Disease Control and Prevention. Korea National Health and Nutrition Examination survey [Internet]. Cheongju: Korea Center for Disease Control and Prevention;2015. cited 2016 Sep 11. Available from: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.8. Jung-Choi KH, Khang YH, Cho HJ. Hidden female smokers in Asia: a comparison of self-reported with cotinine-verified smoking prevalence rates in representative national data from an Asian population. Tob Control. 2012; 21:536–542.
Article9. Sheffer CE, Anders M, Brackman SL, Steinberg MB, Barone C. Tobacco intervention practices of primary care physicians treating lower socioeconomic status patients. Am J Med Sci. 2012; 343:388–396.
Article10. Schroeder SA. Depression, smoking, and heart disease: how can psychiatrists be effective? Am J Psychiatry. 2011; 168:876–878.
Article11. Jung KJ, Yun YD, Baek SJ, Jee SH, Kim IS. Smoking-attributable mortality among Korean adults, 2012. J Korea Soc Health Inform Stat. 2013; 38:36–48.12. Jee SH, Jung KJ, Jeon C, Kim H, Yun YD, Kim IS. Smoking attributable risk and medical care cost in 2012 in Korea. J Korean Soc Health Stat. 2014; 39:25–41.13. Cao Y, Kenfield S, Song Y, Rosner B, Qiu W, Sesso HD, Gaziano JM, Ma J. Cigarette smoking cessation and total and cause-specific mortality: a 22-year follow-up study among US male physicians. Arch Intern Med. 2011; 171:1956–1959.
Article14. Hart C, Gruer L, Bauld L. Does smoking reduction in midlife reduce mortality risk? Results of 2 long-term prospective cohort studies of men and women in Scotland. Am J Epidemiol. 2013; 178:770–779.
Article15. Song YM, Sung J, Cho HJ. Reduction and cessation of cigarette smoking and risk of cancer: a cohort study of Korean men. J Clin Oncol. 2008; 26:5101–5106.
Article16. Lee SK, Kweon HJ, Lim DJ, Kim KR, MO HH, Do HJ, Oh SW, Lym YL, Choi JK, Joh HK, Cho DY. The usefulness of heavy smoking index as a test for nicotine dependence. J Korean Acad Fam Med. 2008; 29:405–411.17. 2008 PHS Guideline Update Panel, Liaisons, and Staff. Treating tobacco use and dependence: 2008 update U.S. Public Health Service Clinical Practice guideline executive summary. Respir Care. 2008; 53:1217–1222.18. Patnode CD, Henderson JT, Thompson JH, Senger CA, Fortmann SP, Whitlock EPL. Behavioral counseling and pharmacotherapy interventions for tobacco cessation in adults, including pregnant women: a review of reviews for the US Preventive Services Task Force. Rockville: Agency for Health-care Research and Quality;2015.19. Ministry of Health and Welfare. Smoking cessation guidebook for health care professionals [Internet]. Seoul: Korea Health Promotion Foundation;2011. cited 2016 Sep 11. Available from: http://www.nosmokeguide.or.kr/common/downLoad.mbs?fileSeq=202244&boardId=25762.20. Mills EJ, Thorlund K, Eapen S, Wu P, Prochaska JJ. Cardiovascular events associated with smoking cessation pharmacotherapies: a network meta-analysis. Circulation. 2014; 129:28–41.
Article21. Kim MH, Min S. Craving and treatment in smoking. J Korean Med Assoc. 2011; 54:401–408.
Article22. Berlin I, Grange G, Jacob N, Tanguy ML. Nicotine patches in pregnant smokers: randomised, placebo controlled, multicentre trial of efficacy. BMJ. 2014; 348:g1622.
Article23. National Centre for Smoking Cessation and Training. Local stop smoking services: service and delivery guidance 2014 [Internet]. London: National Centre for Smoking Cessation and Training;2014. cited 2016 Sep 7. Available at: http://www.ncsct.co.uk/publication_service_and_delivery_guidance_2014.php.24. Cooper S, Taggar J, Lewis S, Marlow N, Dickinson A, White-more R, Coleman T. Smoking, Nicotine and Pregnancy (SNAP) Trial Team. Effect of nicotine patches in pregnancy on infant and maternal outcomes at 2 years: follow-up from the randomised, double-blind, placebo-controlled SNAP trial. Lancet Respir Med. 2014; 2:728–737.
Article25. van der Meer RM, Willemsen MC, Smit F, Cuijpers P. Smoking cessation interventions for smokers with current or past depression. Cochrane Database Syst Rev. 2013; (8):CD006102.
Article26. Farley AC, Hajek P, Lycett D, Aveyard P. Interventions for preventing weight gain after smoking cessation. Cochrane Database Syst Rev. 2012; 1:CD006219.
Article27. Anthenelli RM, Benowitz NL, West R, St Aubin L, McRae T, Lawrence D, Ascher J, Russ C, Krishen A, Evins AE. Neuro-psychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet. 2016; 387:2507–2520.
Article28. US Food and Drug Administration. FDA Drug Safety Communication: FDA updates label for stop smoking drug Chantix (varenicline) to include potential alcohol interaction, rare risk of seizures, and studies of side effects on mood, behavior, or thinking [Internet]. Silver Spring: Food and Drug Administration;cited 2016 Sep 7. Available from: http://www.fda.gov/Drugs/DrugSafety/ucm436494.htm.29. Huang Y, Li W, Yang L, Jiang Y, Wu Y. Long-term efficacy and safety of varenicline for smoking cessation: a systematic review and meta-analysis of randomized controlled trials. J Public Health. 2012; 20:355–365.
Article30. Ebbert JO, Hughes JR, West RJ, Rennard SI, Russ C, McRae TD, Treadow J, Yu CR, Dutro MP, Park PW. Effect of varenicline on smoking cessation through smoking reduction: a randomized clinical trial. JAMA. 2015; 313:687–694.
Article31. Ebbert JO, Hatsukami DK, Croghan IT, Schroeder DR, Allen SS, Hays JT, Hurt RD. Combination varenicline and bupropion SR for tobacco-dependence treatment in cigarette smokers: a randomized trial. JAMA. 2014; 311:155–163.
Article32. Koegelenberg CF, Noor F, Bateman ED, van Zyl-Smit RN, Bruning A, O'Brien JA, Smith C, Abdool-Gaffar MS, Emanuel S, Esterhuizen TM, Irusen EM. Efficacy of varenicline combined with nicotine replacement therapy vs varenicline alone for smoking cessation: a randomized clinical trial. JAMA. 2014; 312:155–161.
Article33. Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016; 4:116–128.
Article34. Boyle RG, Solberg LI, Fiore MC. Electronic medical records to increase the clinical treatment of tobacco dependence: a systematic review. Am J Prev Med. 2010; 39:6 Suppl 1. S77–S82.35. DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991; 59:295–304.
Article36. West R. Time for a change: putting the transtheoretical (stages of change) model to rest. Addiction. 2005; 100:1036–1039.
Article37. Fu SS, van Ryn M, Sherman SE, Burgess DJ, Noorbaloochi S, Clothier B, Taylor BC, Schlede CM, Burke RS, Joseph AM. Proactive tobacco treatment and population-level cessation: a pragmatic randomized clinical trial. JAMA Intern Med. 2014; 174:671–677.
Article38. Solberg LI, Boyle RG, Davidson G, Magnan SJ, Carlson CL. Patient satisfaction and discussion of smoking cessation during clinical visits. Mayo Clin Proc. 2001; 76:138–143.
Article39. Barnfather KD, Cope GF, Chapple IL. Effect of incorporating a 10 minute point of care test for salivary nicotine metabolites into a general practice based smoking cessation programme: randomised controlled trial. BMJ. 2005; 331:999.
Article40. Parkes G, Greenhalgh T, Griffin M, Dent R. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ. 2008; 336:598–600.
Article41. Bize R, Burnand B, Mueller Y, Rege-Walther M, Camain JY, Cornuz J. Biomedical risk assessment as an aid for smoking cessation. Cochrane Database Syst Rev. 2012; 12:CD004705.
Article42. Lindson-Hawley N, Aveyard P, Hughes JR. Reduction versus abrupt cessation in smokers who want to quit. Cochrane Database Syst Rev. 2012; 11:CD008033.
Article43. Lindson-Hawley N, Banting M, West R, Michie S, Shinkins B, Aveyard P. Gradual versus abrupt smoking cessation: a randomized, controlled noninferiority trial. Ann Intern Med. 2016; 164:585–592.44. Baha M, Le Faou AL. Gradual versus abrupt quitting among French treatment-seeking smokers. Prev Med. 2014; 63:96–102.
Article45. Park SW. Evidence-based smoking cessation counseling: motivational intervention and relapse prevention. J Korean Med Assoc. 2011; 54:1036–1046.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of Internet Smoking Cessation Program to Encourage the Personal Intention to Quit Smoking
- Changing Mechanisms Corresponding to The Changing Stages of Smoking Cessation
- A Study on Health-related Quality of Life, Smoking Knowledge, Smoking Attitude, and Smoking Cessation Intention in Male Smokers
- Comparison of the Characteristics of Smoking Cessation Success between Short-term and Long-term Success Groups
- The Study of the Process of Smoking Cessation in Adults