Ann Rehabil Med.
2016 Aug;40(4):666-674. 10.5535/arm.2016.40.4.666.
Prediction of Ambulatory Status After Hip Fracture Surgery in Patients Over 60 Years Old
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. guitarren.kim@samsung.com
- KMID: 2356652
- DOI: http://doi.org/10.5535/arm.2016.40.4.666
Abstract
OBJECTIVE
To predict ambulatory capacity, 1 month after physical therapy following hip fracture surgery.
METHODS
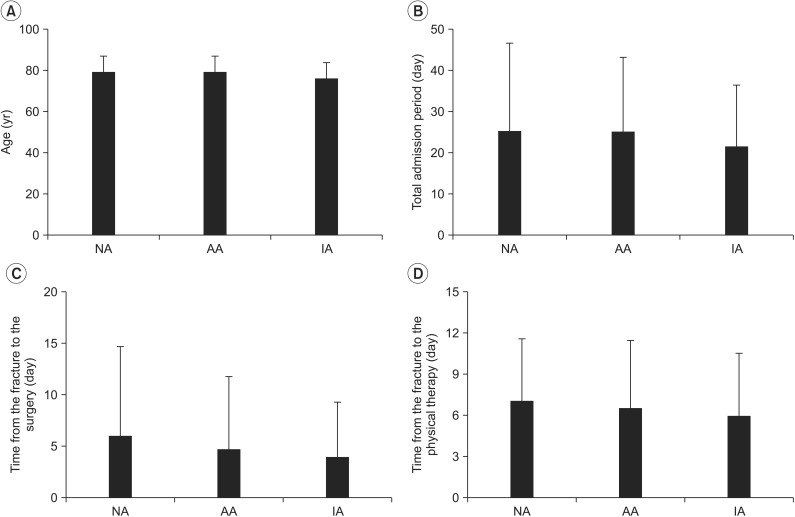
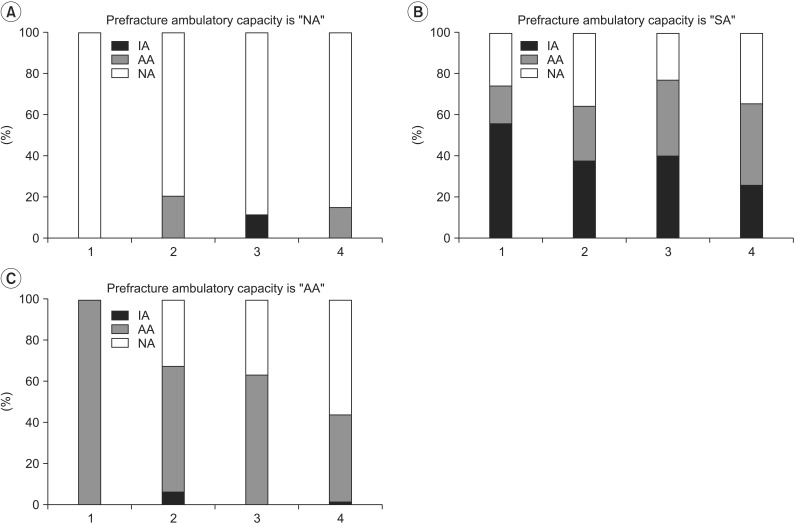
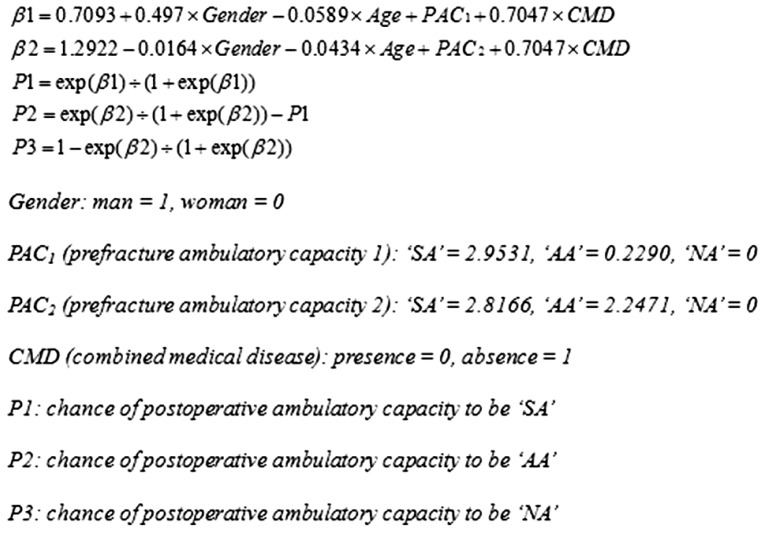
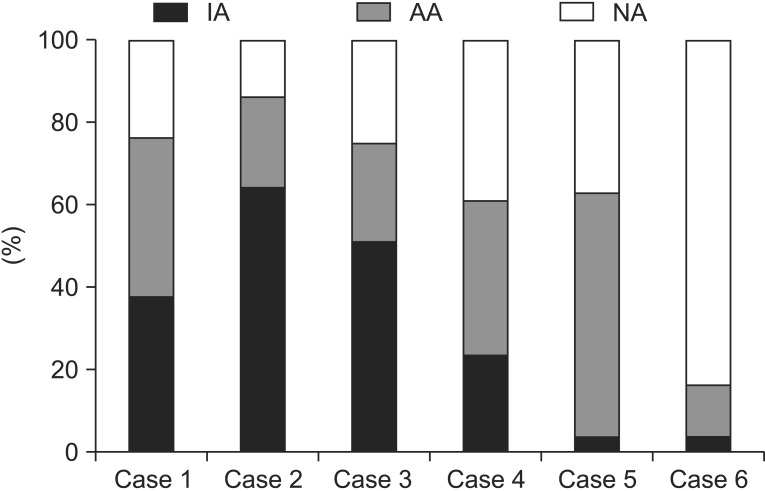
A retrospective chart review was carried out. Patients more than 60 years old, who underwent hip fracture surgery and received physical therapies, were selected (n=548). Age, gender, presence of cognitive dysfunction, combined medical diseases, combined fractures, previous history of hip surgery, prefracture ambulatory capacity, days from the fracture to surgery, type of fracture, type of surgery, presence of postoperative complications, days from the surgery to physical therapy, and total admission period, were collected. Prefracture ambulatory capacity and postoperative ambulatory capacity were classified into non-ambulatory status (NA), ambulation with assistive device (AA), and independent-ambulation without any assistive device (IA). Multiple-logistic regression analysis was performed for the prediction of postoperative ambulatory capacity.
RESULTS
Age (odds ratio [OR]=0.94 for IA and 0.96 for IA or AA), gender (OR=1.64 for IA and 0.98 for IA or AA), prefracture ambulatory capacity (OR of IA=19.17 for IA; OR of IA=16.72 for IA or AA; OR of AA=1.26 for IA, OR of AA=9.46 for IA or AA), and combined medical disease (OR=2.02) were found to be the factors related to postoperative ambulatory capacity and the prediction model was set up using these four factors.
CONCLUSION
Using this model, we can predict the ambulatory capacity following hip fracture surgery. Further prospective studies should be constructed to improve postoperative ambulatory capacity.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Effects of Repetitive Peripheral Magnetic Stimulation Over Vastus Lateralis in Patients After Hip Replacement Surgery
Junghyun Baek, Nohkyoung Park, Bongju Lee, Sungju Jee, Shinseung Yang, Sangkuk Kang
Ann Rehabil Med. 2018;42(1):67-75. doi: 10.5535/arm.2018.42.1.67.
Reference
-
1. Fuller GF. Falls in the elderly. Am Fam Physician. 2000; 61:2159–2168. 2173–2174. PMID: 10779256.2. Rose S, Maffulli N. Hip fractures: an epidemiological review. Bull Hosp Jt Dis. 1999; 58:197–201. PMID: 10711369.3. Lim JY, Park WB, Oh MK, Kang EK, Paik NJ. Falls in a proportional region population in Korean elderly: incidence, consequences, and risk factors. J Korean Geriatr Soc. 2010; 14:8–17.
Article4. Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997; 103:12S–19S. PMID: 9302893.
Article5. Dubljanin-Raspopovic E, Markovic Denic L, Marinkovic J, Grajic M, Tomanovic Vujadinovic S, Bumbasirevic M. Use of early indicators in rehabilitation process to predict one-year mortality in elderly hip fracture patients. Hip Int. 2012; 22:661–667. PMID: 23233176.6. Van Hook FW, Demonbreun D, Weiss BD. Ambulatory devices for chronic gait disorders in the elderly. Am Fam Physician. 2003; 67:1717–1724. PMID: 12725450.7. Levin P. Ambulatory assistive devices in orthopaedics: uses and modifications. J Am Acad Orthop Surg. 2010; 18:315–316. PMID: 20511435.8. Kristensen MT. Factors affecting functional prognosis of patients with hip fracture. Eur J Phys Rehabil Med. 2011; 47:257–264. PMID: 21597435.9. Hershkovitz A, Kalandariov Z, Hermush V, Weiss R, Brill S. Factors affecting short-term rehabilitation outcomes of disabled elderly patients with proximal hip fracture. Arch Phys Med Rehabil. 2007; 88:916–921. PMID: 17601474.
Article10. Folden S, Tappen R. Factors influencing function and recovery following hip repair surgery. Orthop Nurs. 2007; 26:234–241. PMID: 17882100.
Article11. Foss NB, Kristensen MT, Kehlet H. Prediction of postoperative morbidity, mortality and rehabilitation in hip fracture patients: the cumulated ambulation score. Clin Rehabil. 2006; 20:701–708. PMID: 16944827.
Article12. Semel J, Gray JM, Ahn HJ, Nasr H, Chen JJ. Predictors of outcome following hip fracture rehabilitation. PM R. 2010; 2:799–805. PMID: 20869677.
Article13. Bellelli G, Noale M, Guerini F, Turco R, Maggi S, Crepaldi G, et al. A prognostic model predicting recovery of walking independence of elderly patients after hip-fracture surgery: an experiment in a rehabilitation unit in Northern Italy. Osteoporos Int. 2012; 23:2189–2200. PMID: 22222753.
Article14. Mungas D. In-office mental status testing: a practical guide. Geriatrics. 1991; 46:54–58. 6366PMID: 2060803.15. Bohannon RW. Scoring transfer and locomotion independence of home care patients: Barthel versus functional independence measure. Int J Rehabil Res. 1999; 22:65–66. PMID: 10207754.16. Holt G, Smith R, Duncan K, Hutchison JD, Gregori A. Gender differences in epidemiology and outcome after hip fracture: evidence from the Scottish Hip Fracture Audit. J Bone Joint Surg Br. 2008; 90:480–483. PMID: 18378923.17. Lee D, Jo JY, Jung JS, Kim SJ. Prognostic factors predicting early recovery of pre-fracture functional mobility in elderly patients with hip fracture. Ann Rehabil Med. 2014; 38:827–835. PMID: 25566483.
Article18. Lieberman D, Fried V, Castel H, Weitzmann S, Lowenthal MN, Galinsky D. Factors related to successful rehabilitation after hip fracture: a case-control study. Disabil Rehabil. 1996; 18:224–230. PMID: 8743299.
Article19. Keevil VL, Hayat S, Dalzell N, Moore S, Bhaniani A, Luben R, et al. The physical capability of community-based men and women from a British cohort: the European Prospective Investigation into Cancer (EPIC)-Norfolk study. BMC Geriatr. 2013; 13:93. PMID: 24020915.
Article20. Haentjens P, Autier P, Barette M, Venken K, Vanderschueren D, Boonen S, et al. Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone. 2007; 41:958–964. PMID: 17913614.
Article21. Mathew RO, Hsu WH, Young Y. Effect of comorbidity on functional recovery after hip fracture in the elderly. Am J Phys Med Rehabil. 2013; 92:686–696. PMID: 23370578.
Article22. Kenzora JE, McCarthy RE, Lowell JD, Sledge CB. Hip fracture mortality: relation to age, treatment, preoperative illness, time of surgery, and complications. Clin Orthop Relat Res. 1984; (186):45–56. PMID: 6723159.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Could Patient Undergwent Surgical Treatment for Periprosthetic Femoral Fracture after Hip Arthroplasty Return to Their Status before Trauma?
- Ambulatory Outcome after Hip Fractures in Patients with Cerebrovascular Accident
- Risk Factors for Subsequent Contralateral Hip Fracture following Osteoporotic Hip Fracture Surgery
- Prognostic Factors for Functional Recovery at 1-Year Following Fragility Hip Fractures
- Second hip fracture in Hong Kong e Incidence, demographics, and mortality