Hip Pelvis.
2016 Jun;28(2):90-97. 10.5371/hp.2016.28.2.90.
Could Patient Undergwent Surgical Treatment for Periprosthetic Femoral Fracture after Hip Arthroplasty Return to Their Status before Trauma?
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. dshwang@cnu.ac.kr
- KMID: 2328344
- DOI: http://doi.org/10.5371/hp.2016.28.2.90
Abstract
- PURPOSE
The purpose of this study was to compare preoperative clinical outcomes before occurrence of periprosthetic femoral fracture (status before trauma) with postoperative clinical outcomes (status after operation) in patients with periprosthetic femoral fracture after hip arthroplasty.
MATERIALS AND METHODS
A retrospective review was performed of all periprosthetic femoral fracture after hip arthroplasty treated surgically at our institution from January 2010 to January 2014. Among 29 patients who underwent surgical treatment for periprosthetic femoral fracture after hip arthroplasty, 3 patients excluded because of non-union of the fracture site. The clinical outcomes were determined by using visual analogue scale for pain (VAS), Harris hip score (HHS), and ambulatory ability using Koval classification. VAS, HHS and ambulatory ability was assessed for all the included patients at the last follow-up of status before trauma and after operation.
RESULTS
The mean VAS, HHS and ambulatory ability at the last follow-up of status before trauma was 2.2 (range, 0-4), 78.9 (range, 48-92) and 1.9 (range, 1-5), respectively. The mean VAS, HHS and ambulatory ability at the last follow-up of status after operation was 3.1 (range, 1-5), 68.4 (range, 46-81) and 2.9 (range, 2-6), respectively. The clinical outcome of VAS, HHS and ambulatory ability were significantly worsened after surgical treatment for periprosthetic femoral fracture (P=0.010, P=0.001, and P=0.002, respectively).
CONCLUSION
Patients with periprosthetic femoral fracture after hip arthroplasty could not return to their status before trauma, although patients underwent appropriate surgical treatment and the fracture union achieved.
Keyword
MeSH Terms
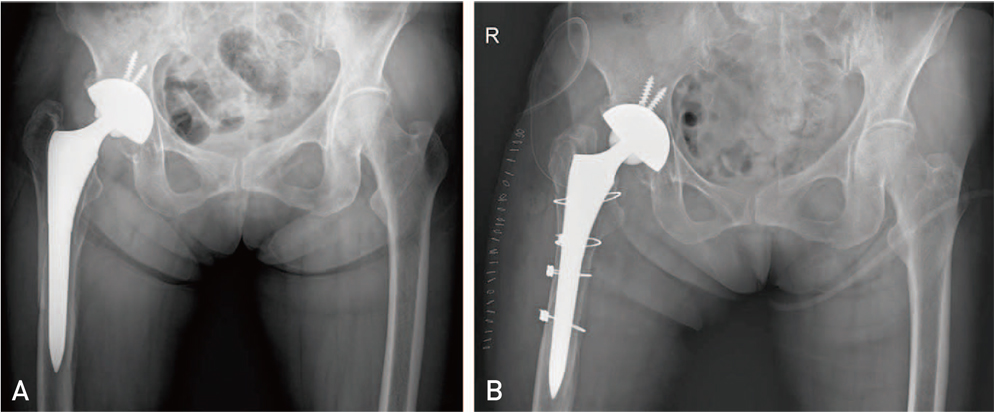
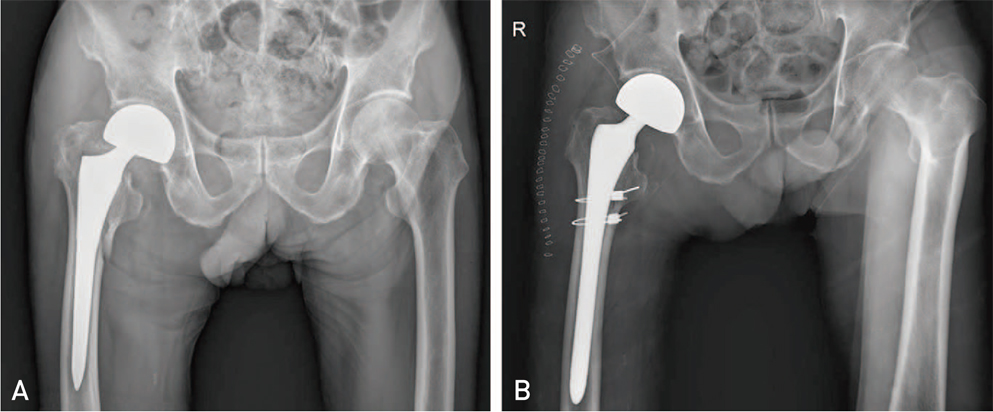
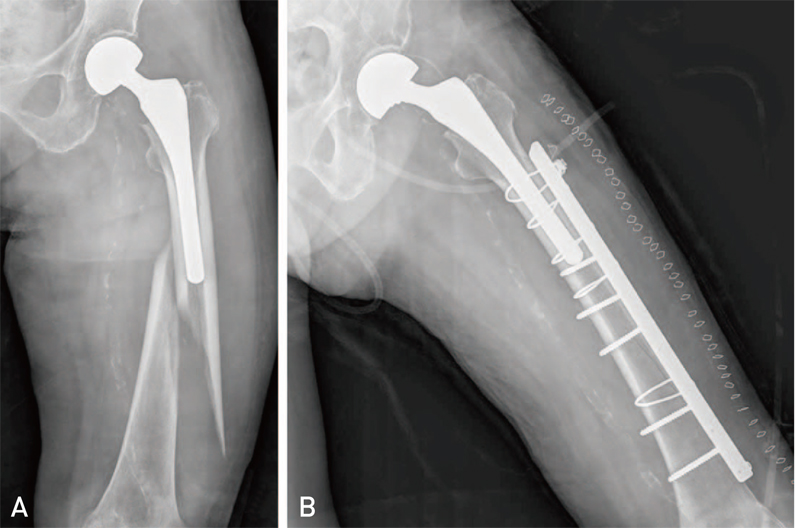
Figure
Cited by 1 articles
-
Prognostic Factors and Clinical Outcomes after Treatment of Periprosthetic Femoral Fractures Using a Cable-plate
Joon Soon Kang, Kyoung-Ho Moon, Bong Sung Ko, Tae Hoon Roh, Yeop Na, Yung-Hun Youn, Joo Hyun Park
Hip Pelvis. 2019;31(3):166-173. doi: 10.5371/hp.2019.31.3.166.
Reference
-
1. Horwitz IB, Lenobel MI. Artificial hip prosthesis in acute and nonunion fractures of the femoral neck: follow-up study of seventy cases. J Am Med Assoc. 1954; 155:564–567.
Article2. Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999; 30:183–190.3. Papadimitropoulos EA, Coyte PC, Josse RG, Greenwood CE. Current and projected rates of hip fracture in Canada. CMAJ. 1997; 157:1357–1363.4. Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007; 38:651–654.
Article5. Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am. 2003; 85-A:2156–2162.
Article6. Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011; 93:96–101.
Article7. Lindahl H, Oden A, Garellick G, Malchau H. The excess mortality due to periprosthetic femur fracture. A study from the Swedish national hip arthroplasty register. Bone. 2007; 40:1294–1298.
Article8. Klein GR, Parvizi J, Rapuri V, et al. Proximal femoral replacement for the treatment of periprosthetic fractures. J Bone Joint Surg Am. 2005; 87:1777–1781.
Article9. Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004; (420):80–95.
Article10. Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995; 44:293–304.11. Rayan F, Dodd M, Haddad FS. European validation of the Vancouver classification of periprosthetic proximal femoral fractures. J Bone Joint Surg Br. 2008; 90:1576–1579.
Article12. Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000; 15:59–62.
Article13. Park MS, Lim YJ, Chung WC, Ham DH, Lee SH. Management of periprosthetic femur fractures treated with distal fixation using a modular femoral stem using an anterolateral approach. J Arthroplasty. 2009; 24:1270–1276.
Article14. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995; (310):150–159.15. Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996; 275:858–865.
Article16. Phillips JR, Moran CG, Manktelow AR. Periprosthetic fractures around hip hemiarthroplasty performed for hip fracture. Injury. 2013; 44:757–762.
Article17. Cram P, Lu X, Callaghan JJ, Vaughan-Sarrazin MS, Cai X, Li Y. Long-term trends in hip arthroplasty use and volume. J Arthroplasty. 2012; 27:278–285.e2.
Article18. Beals RK, Tower SS. Periprosthetic fractures of the femur. An analysis of 93 fractures. Clin Orthop Relat Res. 1996; (327):238–246.19. Park SK, Kim YG, Kim SY. Treatment of periprosthetic femoral fractures in hip arthroplasty. Clin Orthop Surg. 2011; 3:101–106.
Article20. Niikura T, Lee SY, Sakai Y, Nishida K, Kuroda R, Kurosaka M. Treatment results of a periprosthetic femoral fracture case series: treatment method for Vancouver type b2 fractures can be customized. Clin Orthop Surg. 2014; 6:138–145.
Article21. Moreta J, Aguirre U, de Ugarte OS, Jáuregui I, Mozos JL. Functional and radiological outcome of periprosthetic femoral fractures after hip arthroplasty. Injury. 2015; 46:292–298.
Article22. Moore RE, Baldwin K, Austin MS, Mehta S. A systematic review of open reduction and internal fixation of periprosthetic femur fractures with or without allograft strut, cerclage, and locked plates. J Arthroplasty. 2014; 29:872–876.
Article23. García-Rey E, García-Cimbrelo E, Cruz-Pardos A, Madero R. Increase of cortical bone after a cementless long stem in periprosthetic fractures. Clin Orthop Relat Res. 2013; 471:3912–3921.
Article24. Scholz R, Pretzsch M, Matzen P, von Salis-Soglio GF. Treatment of periprosthetic femoral fractures associated with total hip arthroplasty. Z Orthop Ihre Grenzgeb. 2003; 141:296–302.25. Young SW, Pandit S, Munro JT, Pitto RP. Periprosthetic femoral fractures after total hip arthroplasty. ANZ J Surg. 2007; 77:424–428.
Article26. Visnjevac O, Davari-Farid S, Lee J, et al. The effect of adding functional classification to ASA status for predicting 30-day mortality. Anesth Analg. 2015; 121:110–116.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Periprosthetic Femoral Fractures after Hip Arthroplasty
- Periprosthetic Atypical Femoral Fracture-like Fracture after Hip Arthroplasty: A Report of Three Cases
- Repeated Periprosthethic Femoral Fracture in a Below Knee Amputee with Ipsilateral Cementless Total Hip Arthroplasty: A Case Report
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty
- Periprosthetic Femur Fracture due to Unrecognized Surgical Instrument Left in the Medullary Canal : A case report