J Cerebrovasc Endovasc Neurosurg.
2016 Jun;18(2):141-146. 10.7461/jcen.2016.18.2.141.
Treatment of a Giant Serpentine Aneurysm in the Anterior Cerebral Artery
- Affiliations
-
- 1Department of Neurosurgery, Busan Paik Hospital, Inje University, School of Medicine, Busan, Korea.
- 2Department of Diagnostic Radiology, Busan Paik Hospital, Inje University, School of Medicine, Busan, Korea. hwjeong2000@lycos.co.kr
- KMID: 2354891
- DOI: http://doi.org/10.7461/jcen.2016.18.2.141
Abstract
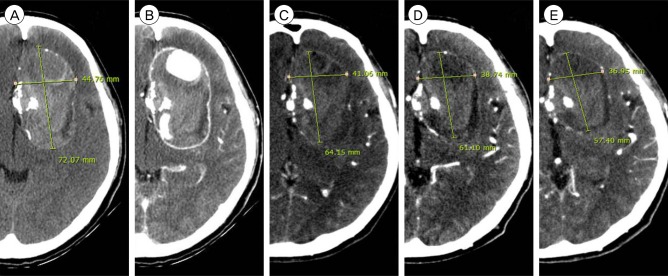
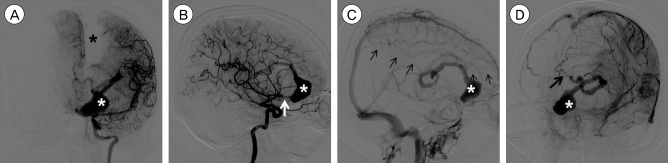
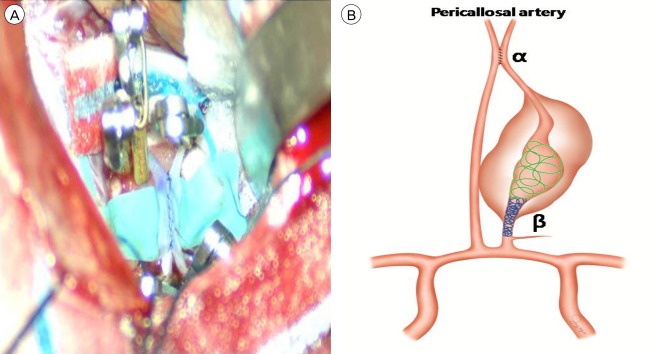
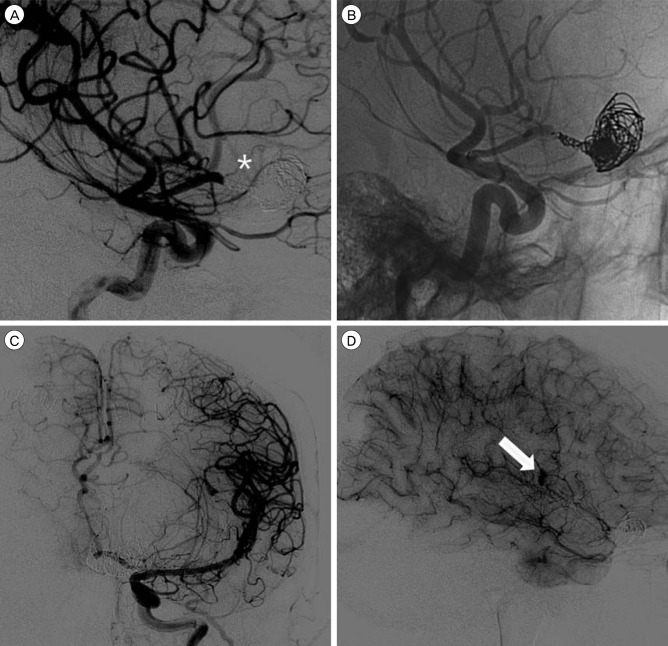
- A giant serpentine aneurysm (GSA) in the anterior cerebral artery (ACA) poses a technical challenge in treatment given its large size, unique neck, and dependent distal vessels. Here we report the case of a GSA in the ACA successfully treated with a combined surgical and endovascular approach. A 54-year-old woman presented with dull headache. On brain computed tomography (CT), a large mass (7 cm × 5 cm × 5 cm) was identified in the left frontal lobe. Cerebral angiography revealed a GSA in the left ACA. Bypass surgery of the distal ACA was performed, followed byocclusion of the entry channel via an endovascular approach. Follow-up CT performed 5 days after treatment revealed disappearance of the vascular channel and peripheral rim enhancement. Follow-up imaging studies performed 7 months after treatment revealed gradual reduction of the mass effect and patency of bypass flow. No complications were noted over a period of 1 year after surgery.
MeSH Terms
Figure
Reference
-
1. Abla AA, Lawton MT. Anterior cerebral artery bypass for complex aneurysms: An experience with intracranial-intracranial reconstruction and review of bypass options. J Neurosurg. 2014; 6. 120(6):1364–1377. PMID: 24745711.
Article2. Aletich VA, Debrun GM, Monsein LH, Nauta HJ, Spetzler RF. Giant serpentine aneurysms: A review and presentation of five cases. AJNR Am J Neuroradiol. 1995; 5. 16(5):1061–1072. PMID: 7639128.3. Amin-Hanjani S, Chen PR, Chang SW, Spetzler RF. Long-term follow-up of giant serpentine MCA aneurysm treated with EC-IC bypass and proximal occlusion. Acta Neurochir (Wien). 2006; 2. 148(2):227–228. PMID: 16322902.
Article4. Carlson AP. Tailored PICA revascularization for unusual ruptured fusiform vertebro-PICA origin aneurysms: Rationale and case illustrations. J Neurol Surg Rep. 2015; 11. 76(2):e275–e278. PMID: 26623241.
Article5. Christiano LD, Gupta G, Prestigiacomo CJ, Gandhi CD. Giant serpentine aneurysms. Neurosurg Focus. 2009; 5. 26(5):E5.
Article6. Dunn GP, Gerrard JL, Jho DH, Ogilvy CS. Surgical treatment of a large fusiform distal anterior cerebral artery aneurysm with in situ end-to-side A3-A3 bypass graft and aneurysm trapping: Case report and review of the literature. Neurosurgery. 2011; 2. 68(2):E587–E591. discussion E591. PMID: 21135720.7. Fanning NF, Kelleher MO, Ryder DQ. The pretzel sign: Angiographic pattern of tortuous intra-aneurysmal blood flow in a giant serpentine aneurysm. Br J Neurosurg. 2003; 2. 17(1):67–71. PMID: 12779205.
Article8. Ferroli P, Ciceri E, Addis A, Broggi G. Self-closing surgical clips for use in pericallosal artery-pericallosal artery side-to-side bypass. J Neurosurg. 2008; 8. 109(2):330–334. PMID: 18671649.
Article9. Horowitz MB, Yonas H, Jungreis C, Hung TK. Management of a giant middle cerebral artery fusiform serpentine aneurysm with distal clip application and retrograde thrombosis: Case report and review of the literature. Surg Neurol. 1994; 3. 41(3):221–225. PMID: 8146737.
Article10. Ikeda A, Shibuya M, Okada T, Kageyama N. Microvascular side-to-side anastomosis. basic problems and clinical applications. Neurol Med Chir (Tokyo). 1986; 5. 26(5):379–384. PMID: 2429217.11. Lawton MT, Hamilton MG, Morcos JJ, Spetzler RF. Revascularization and aneurysm surgery: Current techniques, indications, and outcome. Neurosurgery. 1996; 1. 38(1):83–92. discussion 92-4. PMID: 8747955.
Article12. Lehecka M, Dashti R, Hernesniemi J, Niemela M, Koivisto T, Ronkainen A, et al. Microneurosurgical management of aneurysms at A3 segment of anterior cerebral artery. Surg Neurol. 2008; 8. 70(2):135–151. discussion 152. PMID: 18482754.
Article13. Otsuka G, Miyachi S, Handa T, Negoro M, Okamoto T, Suzuki O. Endovascular trapping of giant serpentine aneurysms by using guglielmi detachable coils: Successful reduction of mass effect. report of two cases. J Neurosurg. 2001; 5. 94(5):836–840. PMID: 11354420.14. Park ES, Ahn JS, Park JC, Kwon DH, Kwun BD, Kim CJ. STA-ACA bypass using the contralateral STA as an interposition graft for the treatment of complex ACA aneurysms: Report of two cases and a review of the literature. Acta Neurochir (Wien). 012; 8. 154(8):1447–1453. PMID: 22692589.
Article15. Segal HD, McLaurin RL. Giant serpentine aneurysm. report of two cases. J Neurosurg. 1977; 1. 46(1):115–120. PMID: 830809.16. Suzuki S, Takahashi T, Ohkuma H, Shimizu T, Fujita S. Management of giant serpentine aneurysms of the middle cerebral artery--review of literature and report of a case successfully treated by STA-MCA anastomosis only. Acta Neurochir (Wien). 1992; 117(1-2):23–29. PMID: 1514425.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Giant Serpentine Aneurysm of the Middle Cerebral Artery
- Giant Serpentine Intracranial Aneurysm Treated with Wrapping under the Extracorporeal Circulation and Hypothermia
- Giant Serpentine Aneurysm of the Anterior Communicating Artery: Case Report
- Surgical Treatment of Giant Serpentine Aneurysm of A2-A3 Segment Distal Anterior Cerebral Artery : Technical Case Report
- Giant Serpentine Aneurysm of the Posterior Cerebral Artery: Case Report