J Dent Anesth Pain Med.
2016 Sep;16(3):193-197. 10.17245/jdapm.2016.16.3.193.
Body composition and hemodynamic changes in patients with special needs
- Affiliations
-
- 1Department of Dental Anesthesiology, Kyushu University Hospital, Fukuoka, Japan. tsukamoto@dent.kyushu-u.ac.jp
- 2Department of Dental Anesthesiology, Faculty of Dental Science, Kyushu University, Fukuoka, Japan.
- KMID: 2354654
- DOI: http://doi.org/10.17245/jdapm.2016.16.3.193
Abstract
- BACKGROUND
Some patients with special needs exhibit intellectual disability, including deficits in cognitive skills and decreased quality of life. The purpose of this study was to retrospectively compare changes in body composition and hemodynamics during general anesthesia in patients with and without special needs.
METHODS
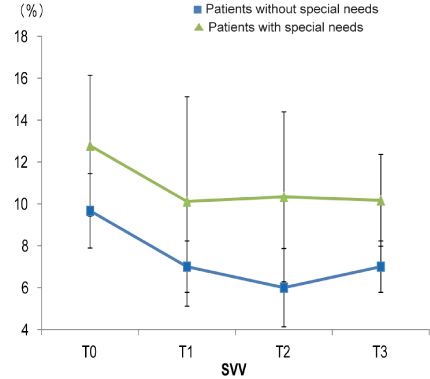
The backgrounds of patients who underwent oral maxillofacial surgery under general anesthesia were recorded from medical records. Intracellular water (ICW), extracellular water (ECW), stroke volume variation (SVV), and heart rate (HR) were recorded for 3 h after the start of anesthesia. Categorical data were compared using an unpaired t-test, and a P-value of less than 0.05 was regarded as significant. Numerical data were compared using the Bonferroni correction, and a P-value of less than 0.0125 was regarded as significant.
RESULTS
A total of 21 patients were included in the study: 10 patients without special needs (non-S-group) and 11 patients with special needs (S-group). There were no significant differences in patients' backgrounds, except with regard to height (P = 0.03). In both groups, ICW and ECW were maintained, although they were lower in the S-group compared to the non-S-group. SVV was maintained in both groups, although it was higher in the S-group than the non-S-group. HR was significantly lower in the S-group 1 h after induction of anesthesia (P < 0.003).
CONCLUSIONS
Changes in hemodynamics due to body fluid imbalance should be monitored during general anesthesia, especially for patients with special needs.
Keyword
MeSH Terms
Figure
Reference
-
1. Shirakawa T. Dental care for special needs children. Jpn J Pediatr Dent. 2010; 48:659–666.
Article2. Messieha Z, Ananda RC, Hoffman I, Hoffman W. Five year outcomes study of dental rehabilitation conducted under general anesthesia for special needs patients. Anesth Prog. 2007; 54:170–174.
Article3. Lee HS, Jung HI, Kim SM, Kim J, Doh RM, Lee JH. Attitudes of Korean Dental students toward individuals with special health care needs. J Dent Educ. 2015; 79:1024–1030.
Article4. Dolan TA, Atchison K, Huynh TN. Access to dental care among older adults in the United States. J Dent Educ. 2005; 69:961–974.
Article5. Malbrain ML, Huygh J, Dabrowski W, De Waele JJ, Staelens A, Wauters J. The use of bio-electrical impedance analysis (BIA) to guide fluid management, resuscitation and deresuscitation in critically ill patients: a bench-to bed side review. Anaesthesiol Intensive Ther. 2014; 46:381–391.
Article6. Tomaske M, Knirsch W, Kretshmar O, Woitzek K, Balmer C, Schmitz A, et al. Cardiac output measurement in children: comparison of Aesculon® cardiac output monitor and thermodilution. Br J Anaesth. 2008; 100:517–520.
Article7. Jacob M, Chappell D, Conzen P, Finsterer U, Rehm M. Blood volume is normal after pre-operative overnight fasting. Acta Anaesthesiol Scand. 2008; 52:522–529.8. Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, et al. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg. 2001; 92:984–989.9. Yoshitaka S, Masahiro I, Mitsuru D, Michio K. A patient with Down's syndrome and undiagnosed hyper trophic cardiomyopathy developing acute heart failure during general anesthesia. J Clin Anesth. 2008; 32:1647–1650.
Article10. Ohashi Y, Otani T, Tai R, Tanaka Y, Sakai K, Aikawa A. Assessment of body composition using dry mass index and ratio of total body water to estimated volume based on bioelectrical impedance analysis in chronic kidney disease patients. J Ren Nutr. 2013; 23:28–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Regular Exercise Program on Body Composition and Body Image in Adults Using One Fitness Center
- Body Composition Changes in Korean Children and Adolescents
- Volume Control by Using the Body Composition Monitor in a Puerperal Patient on Hemodialysis
- Validity of Bioelectrical Impedance Analysis (BIA) in Measurement of Human Body Composition
- The Usefulness of Body Composition Analysis in Obese patients