Yonsei Med J.
2015 Jan;56(1):204-211. 10.3349/ymj.2015.56.1.204.
NGF and HB-EGF: Potential Biomarkers that Reflect the Effects of Fesoterodine in Patients with Overactive Bladder Syndrome
- Affiliations
-
- 1Department of Obstetrics and Gynecology, International St. Mary's Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea.
- 2Department of Obstetrics and Gynecology, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea. swbai@yuhs.ac
- KMID: 2352808
- DOI: http://doi.org/10.3349/ymj.2015.56.1.204
Abstract
- PURPOSE
To determine whether levels of nerve growth factor (NGF) and heparin-binding epidermal growth factor-like growth factor (HB-EGF) can be used to objectively assess overactive bladder syndrome (OAB) treatment outcome and to evaluate the effects of fixed-dose fesoterodine on OAB symptoms.
MATERIALS AND METHODS
This study included 124 participants (62 patients with OAB and 62 controls) in Severance Hospital between 2010 and 2012. In patients with OAB, 4 mg fesoterodine was administered once daily. Repeated evaluations of putative biomarker levels, urine creatinine (Cr) levels, and questionnaire responses, including the Overactive Bladder Symptom Score (OABSS) and the Overactive Bladder Questionnaire (OAB q), were performed from baseline to 16 weeks.
RESULTS
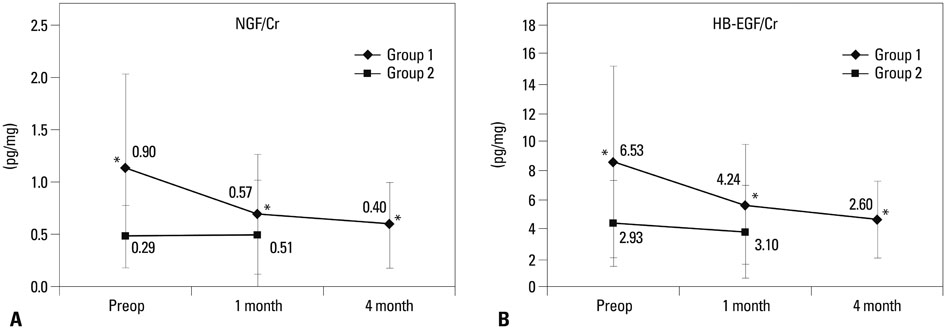
Urinary levels of NGF/Cr (OAB: 1.13+/-0.9 pg/mg; control: 0.5+/-0.29 pg/mg) and HB-EGF/Cr (OAB: 8.73+/-6.55 pg/mg; control: 4.45+/-2.93 pg/mg) were significantly higher in subjects with OAB than in controls (p<0.001). After 16 weeks of fixed-dose fesoterodine treatment, urinary NGF/Cr levels (baseline: 1.13+/-0.08 pg/mg; 16 weeks: 0.60+/-0.4 pg/mg; p=0.02) and HB-EGF/Cr levels significantly decreased (baseline: 8.73+/-6.55 pg/mg; 16 weeks: 4.72+/-2.69 pg/mg; p=0.03, respectively). Both the OABSS and OAB q scores improved (p<0.001). However, there were no a statistically significant correlations between these urinary markers and symptomatic scores.
CONCLUSION
Urinary levels of NGF and HB-EGF may be potential biomarkers for evaluating outcome of OAB treatment. Fixed-dose fesoterodine improved OAB symptoms. Future studies are needed to further examine the significance of urinary NGF and HB-EGF levels as therapeutic markers for OAB.
Keyword
MeSH Terms
-
Adult
Benzhydryl Compounds/pharmacology/*therapeutic use
Biological Markers/urine
Case-Control Studies
Creatinine/urine
Female
Heparin-binding EGF-like Growth Factor/*urine
Humans
Male
Middle Aged
Nerve Growth Factor/*urine
Questionnaires
Treatment Outcome
Urinary Bladder, Overactive/*drug therapy/physiopathology/*urine
Urodynamics
Benzhydryl Compounds
Biological Markers
Creatinine
Heparin-binding EGF-like Growth Factor
Nerve Growth Factor
Figure
Reference
-
1. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006; 50:1306–1314.
Article2. Abrams P, Kelleher CJ, Kerr LA, Rogers RG. Overactive bladder significantly affects quality of life. Am J Manag Care. 2000; 6:11 Suppl. S580–S590.3. Hanno P, Dmochowski R. Status of international consensus on interstitial cystitis/bladder pain syndrome/painful bladder syndrome: 2008 snapshot. Neurourol Urodyn. 2009; 28:274–286.
Article4. Rodríguez MA, Afari N, Buchwald DS. National Institute of Diabetes and Digestive and Kidney Diseases Working Group on Urological Chronic Pelvic Pain. Evidence for overlap between urological and nonurological unexplained clinical conditions. J Urol. 2009; 182:2123–2131.
Article5. Liu HT, Kuo HC. Urinary nerve growth factor level could be a potential biomarker for diagnosis of overactive bladder. J Urol. 2008; 179:2270–2274.
Article6. Liu HT, Kuo HC. Urinary nerve growth factor levels are increased in patients with bladder outlet obstruction with overactive bladder symptoms and reduced after successful medical treatment. Urology. 2008; 72:104–108.
Article7. Steers WD, Kolbeck S, Creedon D, Tuttle JB. Nerve growth factor in the urinary bladder of the adult regulates neuronal form and function. J Clin Invest. 1991; 88:1709–1715.
Article8. Keay SK, Zhang CO, Shoenfelt J, Erickson DR, Whitmore K, Warren JW, et al. Sensitivity and specificity of antiproliferative factor, heparin-binding epidermal growth factor-like growth factor, and epidermal growth factor as urine markers for interstitial cystitis. Urology. 2001; 57:6 Suppl 1. 9–14.
Article9. Kim J, Keay SK, Freeman MR. Heparin-binding epidermal growth factor-like growth factor functionally antagonizes interstitial cystitis antiproliferative factor via mitogen-activated protein kinase pathway activation. BJU Int. 2009; 103:541–546.
Article10. Parsons CL, Greenberger M, Gabal L, Bidair M, Barme G. The role of urinary potassium in the pathogenesis and diagnosis of interstitial cystitis. J Urol. 1998; 159:1862–1866.
Article11. Abrams P, Cardozo L, Khoury S, Wein A. Incontinence. 4th International Consultation on Incontinence. Paris: Health Publication Ltd.;2009.12. Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, et al. Symptom assessment tool for overactive bladder syndrome--overactive bladder symptom score. Urology. 2006; 68:318–323.
Article13. Coyne K, Revicki D, Hunt T, Corey R, Stewart W, Bentkover J, et al. Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: the OAB-q. Qual Life Res. 2002; 11:563–574.14. Keay S, Zhang CO, Kagen DI, Hise MK, Jacobs SC, Hebel JR, et al. Concentrations of specific epithelial growth factors in the urine of interstitial cystitis patients and controls. J Urol. 1997; 158:1983–1988.
Article15. Jacobs BL, Smaldone MC, Tyagi V, Philips BJ, Jackman SV, Leng WW, et al. Increased nerve growth factor in neurogenic overactive bladder and interstitial cystitis patients. Can J Urol. 2010; 17:4989–4994.16. Erickson DR, Tomaszewski JE, Kunselman AR, Stetter CM, Peters KM, Rovner ES, et al. Urine markers do not predict biopsy findings or presence of bladder ulcers in interstitial cystitis/painful bladder syndrome. J Urol. 2008; 179:1850–1856.
Article17. Goto T, Morioka J, Inamura H, Yano M, Kodaira K, Igarashi Y, et al. Urinary eosinophil-derived neurotoxin concentrations in patients with atopic dermatitis: a useful clinical marker for disease activity. Allergol Int. 2007; 56:433–438.
Article18. Zimmerli LU, Schiffer E, Zürbig P, Good DM, Kellmann M, Mouls L, et al. Urinary proteomic biomarkers in coronary artery disease. Mol Cell Proteomics. 2008; 7:290–298.
Article19. Good DM, Thongboonkerd V, Novak J, Bascands JL, Schanstra JP, Coon JJ, et al. Body fluid proteomics for biomarker discovery: lessons from the past hold the key to success in the future. J Proteome Res. 2007; 6:4549–4555.
Article20. Candela JV, Park E, Gerspach JM, Davidoff R, Stout L, Levy SM, et al. Evaluation of urinary IL-1alpha and IL-1beta in gravid females and patients with bacterial cystitis and microscopic hematuria. Urol Res. 1998; 26:175–180.
Article21. Khullar V, Rovner ES, Dmochowski R, Nitti V, Wang J, Guan Z. Fesoterodine dose response in subjects with overactive bladder syndrome. Urology. 2008; 71:839–843.
Article22. Wyndaele JJ, Goldfischer ER, Morrow JD, Gong J, Tseng LJ, Guan Z, et al. Effects of flexible-dose fesoterodine on overactive bladder symptoms and treatment satisfaction: an open-label study. Int J Clin Pract. 2009; 63:560–567.
Article23. Bhide AA, Cartwright R, Khullar V, Digesu GA. Biomarkers in overactive bladder. Int Urogynecol J. 2013; 24:1065–1072.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Investigations of Urinary Nerve Growth Factor as a Biomarker for Overactive Bladder Syndrome
- Role of Nerve Growth Factor in Overactive Bladder
- Potential Biomarkers for Diagnosis of Overactive Bladder Patients: Urinary Nerve Growth Factor, Prostaglandin E2, and Adenosine Triphosphate
- Urinary Nerve Growth Factor as a Potential Biomarker of Treatment Outcomes in Overactive Bladder Patients
- Inhibition of voltage-dependent K+ channels by antimuscarinic drug fesoterodine in coronary arterial smooth muscle cells