J Gynecol Oncol.
2015 Oct;26(4):262-269. 10.3802/jgo.2015.26.4.262.
Longer waiting times for early stage cervical cancer patients undergoing radical hysterectomy are associated with diminished long-term overall survival
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Prince of Songkla University Faculty of Medicine, Songkhla, Thailand. hjitti@yahoo.com
- KMID: 2345916
- DOI: http://doi.org/10.3802/jgo.2015.26.4.262
Abstract
OBJECTIVE
The aim of this study was to evaluate the impact of surgical waiting time on clinical outcome in early stage cervical cancer.
METHODS
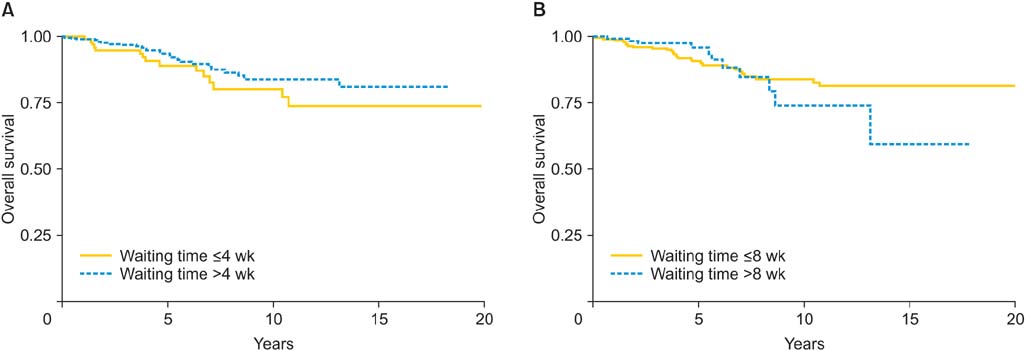
The cohort consisted of 441 patients diagnosed with stages IA2-IB1cervical cancer who underwent radical hysterectomy and pelvic node dissection. The patients were divided into two groups based on surgical waiting time. The associations between waiting time and other potential prognostic factors with clinical outcome were evaluated.
RESULTS
The median surgical waiting time was 43 days. Deep stromal invasion (hazard ratio [HR], 2.5; 95% confidence interval [CI], 1.4 to 4.6; p=0.003) and lymph node metastasis (HR, 2.9; 95% CI, 1.3 to 6.7; p=0.026) were identified as independent prognostic factors for recurrence-free survival while no prognostic significance of surgical waiting time was found (p=0.677). On multivariate analysis of overall survival (OS), only deep stromal invasion (HR, 2.6; 95% CI, 1.3 to 5.0; p=0.009) and lymph node metastasis (HR, 3.6; 95% CI, 1.5 to 8.6; p=0.009) were identified as independent prognostic factors for OS. Although OS showed no significant difference between short (< or =8 weeks) and long (>8 weeks) waiting times, multivariate analysis of OS with time-varying effects revealed that a waiting time longer than 8 weeks was associated with poorer long-term survival (after 5 years; HR, 3.4; 95% CI, 1.3 to 9.2; p=0.021).
CONCLUSION
A longer surgical waiting time was associated with diminished long-term OS of early stage cervical cancer patients.
MeSH Terms
Figure
Cited by 1 articles
-
Effect of Waiting Time from Pathological Diagnosis to Definitive Concurrent Chemoradiation for Cervical Cancer on Overall Survival
Kyoung Won Noh, Bomi Kim, Chel Hun Choi, Tae-Joong Kim, Jeong-Won Lee, Byoung-Gie Kim, Duk-Soo Bae, Won Kyung Cho, Won Park, Yoo-Young Lee
Cancer Res Treat. 2022;54(1):245-252. doi: 10.4143/crt.2021.023.
Reference
-
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.2. Vaccarella S, Lortet-Tieulent J, Plummer M, Franceschi S, Bray F. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013; 49:3262–3273.3. Kruhaprema T, Attasara P, Sriplung H, Wiangnon S, Sangrajrang S. Cancer in Thailand vol VII, 2007-2009. Bangkok: Bangkok Medical Publisher;2013.4. Wilailak S. Epidemiologic report of gynecologic cancer in Thailand. J Gynecol Oncol. 2009; 20:81–83.5. Chittithaworn S, Hanprasertpong J, Tungsinmunkong K, Geater A. Association between prognostic factors and disease-free survival of cervical cancer stage IB1 patients undergoing radical hysterectomy. Asian Pac J Cancer Prev. 2007; 8:530–534.6. Yun YH, Kim YA, Min YH, Park S, Won YJ, Kim DY, et al. The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol. 2012; 23:2731–2737.7. Stec AA, Coons BJ, Chang SS, Cookson MS, Herrell SD, Smith JA Jr, et al. Waiting time from initial urological consultation to nephrectomy for renal cell carcinoma: does it affect survival? J Urol. 2008; 179:2152–2157.8. Raptis DA, Fessas C, Belasyse-Smith P, Kurzawinski TR. Clinical presentation and waiting time targets do not affect prognosis in patients with pancreatic cancer. Surgeon. 2010; 8:239–246.9. Elit LM, O'Leary EM, Pond GR, Seow HY. Impact of wait times on survival for women with uterine cancer. J Clin Oncol. 2014; 32:27–33.10. van Harten MC, Hoebers FJ, Kross KW, van Werkhoven ED, van den Brekel MW, van Dijk BA. Determinants of treatment waiting times for head and neck cancer in the Netherlands and their relation to survival. Oral Oncol. 2015; 51:272–278.11. Umezu T, Shibata K, Kajiyama H, Yamamoto E, Mizuno M, Kikkawa F. Prognostic factors in stage IA-IIA cervical cancer patients treated surgically: does the waiting time to the operation affect survival? Arch Gynecol Obstet. 2012; 285:493–497.12. Perri T, Issakov G, Ben-Baruch G, Felder S, Beiner ME, Helpman L, et al. Effect of treatment delay on survival in patients with cervical cancer: a historical cohort study. Int J Gynecol Cancer. 2014; 24:1326–1332.13. E C, Dahrouge S, Samant R, Mirzaei A, Price J. Radical radiotherapy for cervix cancer: the effect of waiting time on outcome. Int J Radiat Oncol Biol Phys. 2005; 61:1071–1077.14. McLaughlin JM, Anderson RT, Ferketich AK, Seiber EE, Balkrishnan R, Paskett ED. Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. J Clin Oncol. 2012; 30:4493–4500.15. Brazda A, Estroff J, Euhus D, Leitch AM, Huth J, Andrews V, et al. Delays in time to treatment and survival impact in breast cancer. Ann Surg Oncol. 2010; 17:Suppl 3. 291–296.16. Chen Z, King W, Pearcey R, Kerba M, Mackillop WJ. The relationship between waiting time for radiotherapy and clinical outcomes: a systematic review of the literature. Radiother Oncol. 2008; 87:3–16.17. The Lung Cancer Working Party of the British Thoracic Society Standards of Care Committee. BTS recommendations to respiratory physicians for organising the care of patients with lung cancer. Thorax. 1998; 53:Suppl 1. S1–S8.18. Alberts WM, Bepler G, Hazelton T, Ruckdeschel JC, Williams JH. American College of Chest Physicians. Lung cancer: practice organization. Chest. 2003; 123:1 Suppl. 332S–337S.19. Takeda N, Sakuragi N, Takeda M, Okamoto K, Kuwabara M, Negishi H, et al. Multivariate analysis of histopathologic prognostic factors for invasive cervical cancer treated with radical hysterectomy and systematic retroperitoneal lymphadenectomy. Acta Obstet Gynecol Scand. 2002; 81:1144–1151.20. Phoophitphong T, Hanprasertpong J, Dechsukhum C, Geater A. Correlation of angiogenesis and recurrence-free survival of early stage cervical cancer patients undergoing radical hysterectomy with pelvic lymph node dissection. J Obstet Gynaecol Res. 2007; 33:840–848.21. Park JY, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Outcomes after radical hysterectomy according to tumor size divided by 2-cm interval in patients with early cervical cancer. Ann Oncol. 2011; 22:59–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The twenty-first century role of Piver-Rutledge type III radical hysterectomy and FIGO stage IA, IB1, and IB2 cervical cancer in the era of robotic surgery: a personal perspective
- Minimally invasive radical hysterectomy and the importance of avoiding cancer cell spillage for early-stage cervical cancer: a narrative review
- A comparison of robot assisted and abdominal radical hysterectomy (RH) for early stage cervical and endometrial cancer
- Vaginal evisceration after radical hysterectomy and adjuvant radiation
- Novel vaginoplasty technique involving the use of peritoneal flaps during laparoscopic radical hysterectomy for early-stage cervical cancer