Ann Dermatol.
2016 Aug;28(4):464-469. 10.5021/ad.2016.28.4.464.
Stressful Events and Serum Concentration of Substance P in Acne Patients
- Affiliations
-
- 1Division of Skin Disease Prophylaxis, Department of Geriatric Medicine and Gerontology, Poznan University of Medical Sciences, Poznan, Poland. mariolapawlaczyk@o2.pl
- 2Department of Clinical Psychology, Poznan University of Medical Sciences, Poznan, Poland.
- 3Department of Biology and Environmental Study, Poznan University of Medical Sciences, Poznan, Poland.
- 4Department of Clinical Immunology, Poznan University of Medical Sciences, Poznan, Poland.
- 5Department of Computer Science and Statistics, Poznan University of Medical Sciences, Poznan, Poland.
- KMID: 2344817
- DOI: http://doi.org/10.5021/ad.2016.28.4.464
Abstract
- BACKGROUND
Psychological stress is an important factor of acne pathogenesis. Stress related production of hormones, cytokines and neuropeptides may result in the chronic course and exacerbations of the disease.
OBJECTIVE
The aim of the study was to evaluate the relationship between acne severity, intensity of emotional stress and serum concentration of substance P (scSP), to compare the intensity of adversities, psychological stress and scSP in acne patients with healthy controls and to compare coping techniques for stress.
METHODS
The study consisted of 80 patients. Emotional stress was analyzed with the use of social readjustment rating scale, whereas the methods of coping with stress were assessed with the coping inventory for stressful situation questionnaire. The blood concentration of substance P was analyzed by enzyme-linked immunosorbent assay method in a group of 40 patients with acne vulgaris and in control subjects.
RESULTS
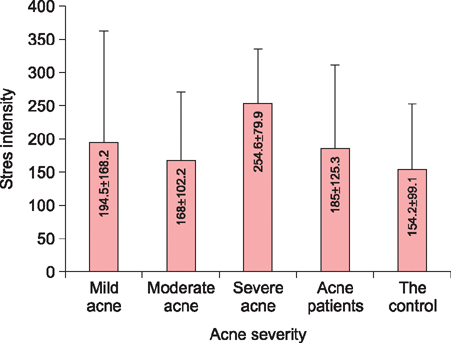
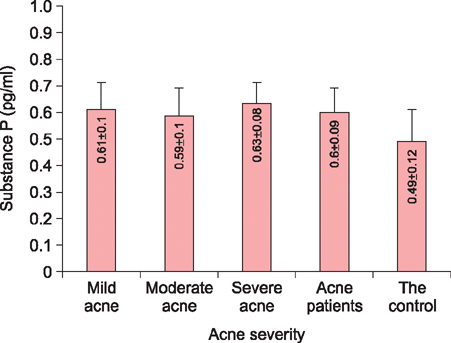
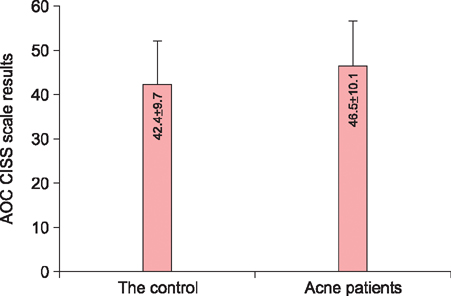
There was no statistically significant difference between the severity of acne and the intensity of stress. Acne patients presented a higher average scSP than the controls. No statistically significant correlation was observed between the severity of acne and scSP; however, the intensity of stress correlated with scSP in the control group. The evaluation of methods of coping with stress showed significantly higher rate for the avoidance-oriented coping among acne patients.
CONCLUSION
The number of stressful events is not a factor that determines the severity of acne. The course of the disease may depend on tolerance to stress and methods of coping with stress.
Keyword
MeSH Terms
Figure
Reference
-
1. Jafferany M. Psychodermatology: a guide to understanding common psychocutaneous disorders. Prim Care Companion J Clin Psychiatry. 2007; 9:203–213.2. Halvorsen JA, Stern RS, Dalgard F, Thoresen M, Bjertness E, Lien L. Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne: a population-based study. J Invest Dermatol. 2011; 131:363–370.
Article3. Picardi A, Lega I, Tarolla E. Suicide risk in skin disorders. Clin Dermatol. 2013; 31:47–56.
Article4. Arck PC, Slominski A, Theoharides TC, Peters EM, Paus R. Neuroimmunology of stress: skin takes center stage. J Invest Dermatol. 2006; 126:1697–1704.
Article5. Thomas DR. Psychosocial effects of acne. J Cutan Med Surg. 2004; 8:Suppl 4. 3–5.
Article6. Liezmann C, Klapp B, Peters EM. Stress, atopy and allergy: a re-evaluation from a psychoneuroimmunologic persepective. Dermatoendocrinol. 2011; 3:37–40.7. Lasek RJ, Chren MM. Acne vulgaris and the quality of life of adult dermatology patients. Arch Dermatol. 1998; 134:454–458.
Article8. Jones-Caballero M, Chren MM, Soler B, Pedrosa E, Peñas PF. Quality of life in mild to moderate acne: relationship to clinical severity and factors influencing change with treatment. J Eur Acad Dermatol Venereol. 2007; 21:219–226.
Article9. Khunger N, Kumar C. A clinico-epidemiological study of adult acne: is it different from adolescent acne? Indian J Dermatol Venereol Leprol. 2012; 78:335–341.
Article10. Zouboulis CC. Modern aspects of acne pathogenesis. J Dtsch Dermatol Ges. 2010; 8:Suppl 1. S7–S14.11. Makrantonaki E, Ganceviciene R, Zouboulis C. An update on the role of the sebaceous gland in the pathogenesis of acne. Dermatoendocrinol. 2011; 3:41–49.
Article12. Lee WJ, Jung HD, Lee HJ, Kim BS, Lee SJ, Kim DW. Influence of substance-P on cultured sebocytes. Arch Dermatol Res. 2008; 300:311–316.
Article13. Tan JK, Tang J, Fung K, Gupta AK, Thomas DR, Sapra S, et al. Development and validation of a comprehensive acne severity scale. J Cutan Med Surg. 2007; 11:211–216.
Article14. Ramli R, Malik AS, Hani AF, Jamil A. Acne analysis, grading and computational assessment methods: an overview. Skin Res Technol. 2012; 18:1–14.
Article15. Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967; 11:213–218.
Article16. Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol. 1990; 58:844–854.
Article17. Bowe W, Patel NB, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis: from anecdote to translational medicine. Benef Microbes. 2014; 5:185–199.
Article18. Toyoda M, Morohashi M. Pathogenesis of acne. Med Electron Microsc. 2001; 34:29–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparative Study on Stressful Life Events and Coping Methods of Medical Inpatients and Community People
- A Comparative Study on Stressful Life Events and Coping Methods of Hypertensive and Nonhypertensive Patients
- Acne Conglobata Induced by Anabolic Androgenic Steroids
- A Study of Serum Levels of Zinc in Acne Vulgaris
- Investigation on Acne Patients' Use and Awareness of Cosmetics for Acne