Korean J Gastroenterol.
2016 Jul;68(1):40-44. 10.4166/kjg.2016.68.1.40.
A Case of Gastro-Gastric Intussusception Secondary to Primary Gastric Lymphoma
- Affiliations
-
- 1Department of Internal Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea. kwonjg@cu.ac.kr
- 2Department of Radiology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- KMID: 2344491
- DOI: http://doi.org/10.4166/kjg.2016.68.1.40
Abstract
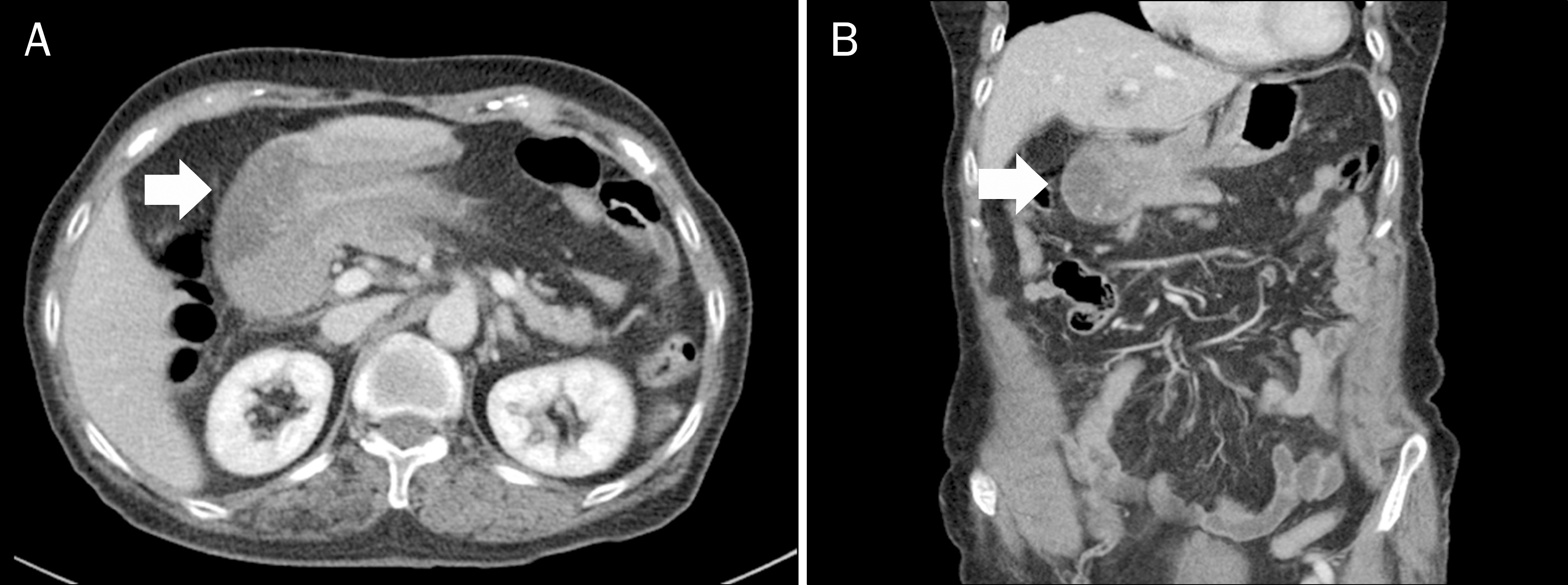
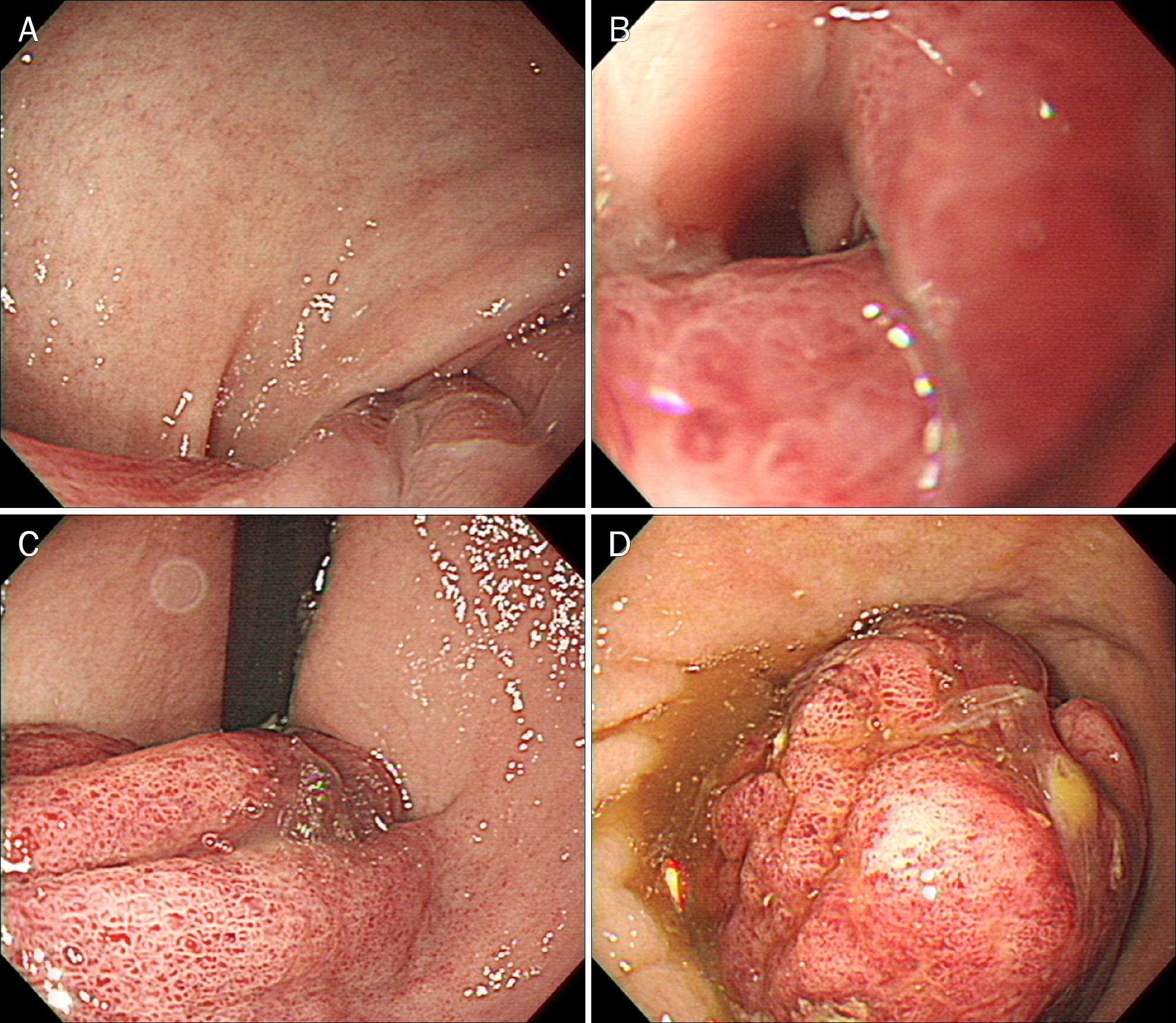
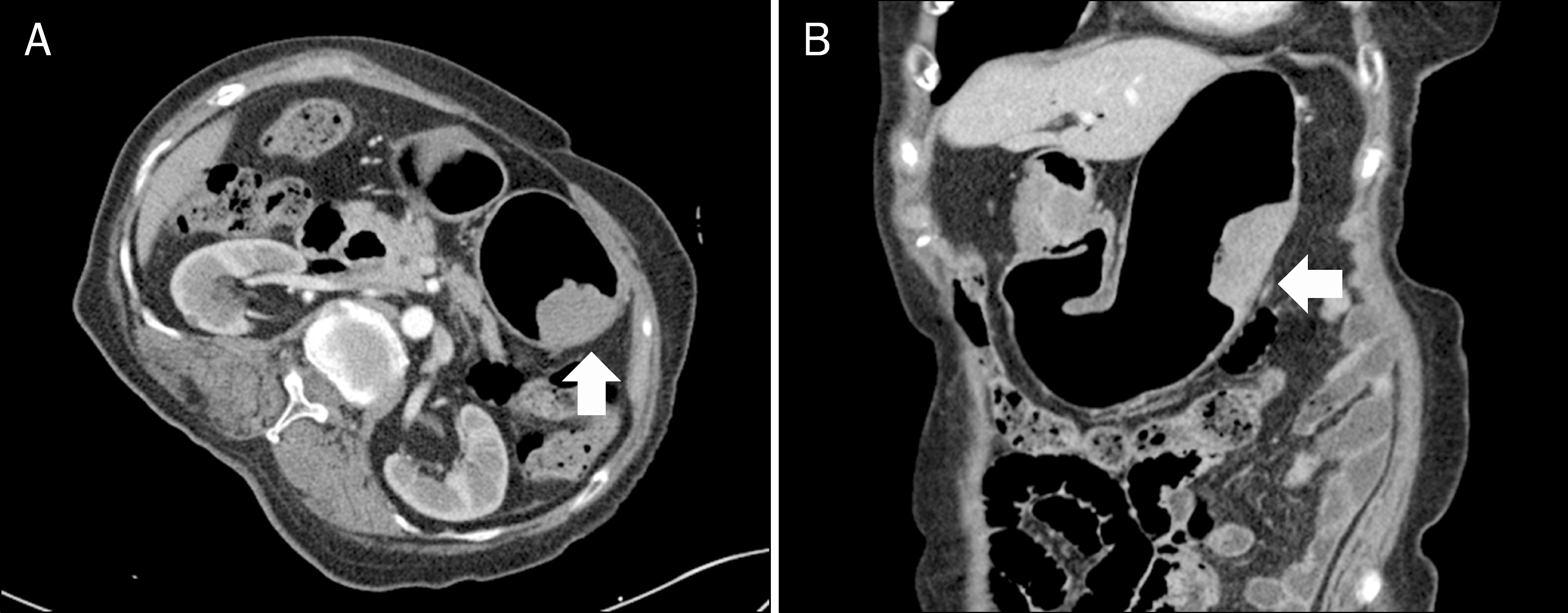
- In adults, most intussusceptions develop from a lesion, usually a benign or malignant neoplasm, and can occur at any site in the gastrointestinal tract. Intussusception in the proximal gastrointestinal tract is uncommon, and gastro-gastric intussusception is extremely rare. We present a case of gastro-gastric intussusception secondary to a primary gastric lymphoma. An 82-year-old female patient presented with acute onset chest pain and vomiting. Abdominal CT revealed a gastro-gastric intussusception. We performed upper gastrointestinal endoscopy, revealing a large gastric mass invaginated into the gastric lumen and distorting the distal stomach. Uncomplicated gastric reposition was achieved with endoscopy of the distal stomach. Histological evaluation of the gastric mass revealed a diffuse large B cell lymphoma that was treated with chemotherapy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009; 15:407–411.
Article2. Sachs M, Encke A. Entero-enteral invagination of the small intestine in adults. A rare cause of "uncertain abdomen". Langenbecks Arch Chir. 1993; 378:288–291.3. Kim DJ, Lee JH, Kim W. Gastroduodenal intussusception resulting from large hyperplastic polyp. J Gastric Cancer. 2012; 12:201–204.
Article4. Mouës CM, Steenvoorde P, Viersma JH, van Groningen K, de Bruïne JF. Jejunal intussusception of a gastric lipoma: a review of literature. Dig Surg. 2002; 19:418–420.
Article5. Ozdogan M, Hamaloglu E, Ozdemir A, Ozenc A. Antegrade jejunojejunal intussusception after Roux-en-Y esophagojejunostomy as an unusual cause of postoperative intestinal obstruction: report of a case. Surg Today. 2001; 31:355–357.
Article6. Eom BW, Ryu KW, Lee JH, et al. Gastrogastric intussusception secondary to a gastric carcinoma: report of a case. Surg Today. 2011; 41:1424–1427.
Article7. Shanbhogue A, Walsh C, Fasih N. Education and imaging. Gastrointestinal: gastrogastric intussusception. J Gastroenterol Hepatol. 2009; 24:169.8. Papaxoinis G, Papageorgiou S, Rontogianni D, et al. Primary gastrointestinal non-Hodgkin's lymphoma: a clinicopathologic study of 128 cases in Greece. A Hellenic Cooperative Oncology Group study (HeCOG). Leuk Lymphoma. 2006; 47:2140–2146.
Article9. Lee SH, Kwon IG, Ryu SW, Sohn SS. Jejunogastric intussusception: a rare complication of gastric cancer surgery. Int J Clin Exp Med. 2014; 7:4498–4502.10. Howard DD, DeShazo ME, Richards WO, Rodning CB. Retrograde jejunojejunal intussusception status following Roux-en-Y gastrojejunostomy. Int Surg. 2010; 95:177–182.11. Eisen LK, Cunningham JD, Aufses AH Jr. Intussusception in adults: institutional review. J Am Coll Surg. 1999; 188:390–395.12. Vikram R, McCulloch AS, Zealley IA. True gastrogastric intussusception: a rare radiologic diagnosis with surgical correlation. AJR Am J Roentgenol. 2006; 186:585–586.
Article13. Grundy A, Rayter Z, Shorthouse AJ. Gastrogastric intussuscepting leiomyomas. Gastrointest Radiol. 1984; 9:319–321.
Article14. Lianos G, Xeropotamos N, Bali C, Baltoggiannis G, Ignatiadou E. Adult bowel intussusception: presentation, location, etiology, diagnosis and treatment. G Chir. 2013; 34:280–283.15. Singla S, Guenthart BA, May L, Gaughan J, Meilahn JE. Intussusception after laparoscopic gastric bypass surgery: an underrecognized complication. Minim Invasive Surg. 2012; 2012:464853.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differences in Endoscopic Findings of Primary and Secondary Gastric Lymphoma
- A Case of Gastroduodenal Intussusception Secondary to Gastric Carcinoid Tumor
- Gastroduodenal Intussusception due to Gastric Submucosal Hemangiomatosis
- The Endoscopic Findings of Gastric Lymphoma
- A Case of Primary Gastric Lymphoma in Puberty