Differential Benefit of Statin in Secondary Prevention of Acute Myocardial Infarction according to the Level of Triglyceride and High Density Lipoprotein Cholesterol
- Affiliations
-
- 1Chonnam National University Hospital, Gwangju, Korea. mhjeong@chonnam.ac.kr
- 2Yeungnam University Hospital, Busan, Korea.
- 3Chungbuk National University Hospital, Cheongju, Korea.
- 4Gwangju Veterans Hospital, Gwangju, Korea.
- 5Kyunghee University College of Medicine, Seoul, Korea.
- KMID: 2344445
- DOI: http://doi.org/10.4070/kcj.2016.46.3.324
Abstract
- BACKGROUND AND OBJECTIVES
The differential benefit of statin according to the state of dyslipidemia has been sparsely investigated. We sought to address the efficacy of statin in secondary prevention of myocardial infarction (MI) according to the level of triglyceride and high density lipoprotein cholesterol (HDL-C) on admission.
SUBJECTS AND METHODS
Acute MI patients (24653) were enrolled and the total patients were divided according to level of triglyceride and HDL-C on admission: group A (HDL-C≥40 mg/dL and triglyceride<150 mg/dL; n=11819), group B (HDL-C≥40 mg/dL and triglyceride≥150 mg/dL; n=3329), group C (HDL-C<40 mg/dL and triglyceride<150 mg/dL; n=6062), and group D (HDL-C<40 mg/dL & triglyceride≥150 mg/dL; n=3443). We evaluated the differential efficacy of statin according to the presence or absence of component of dyslipidemia. The primary end points were major adverse cardiac events (MACE) for 2 years.
RESULTS
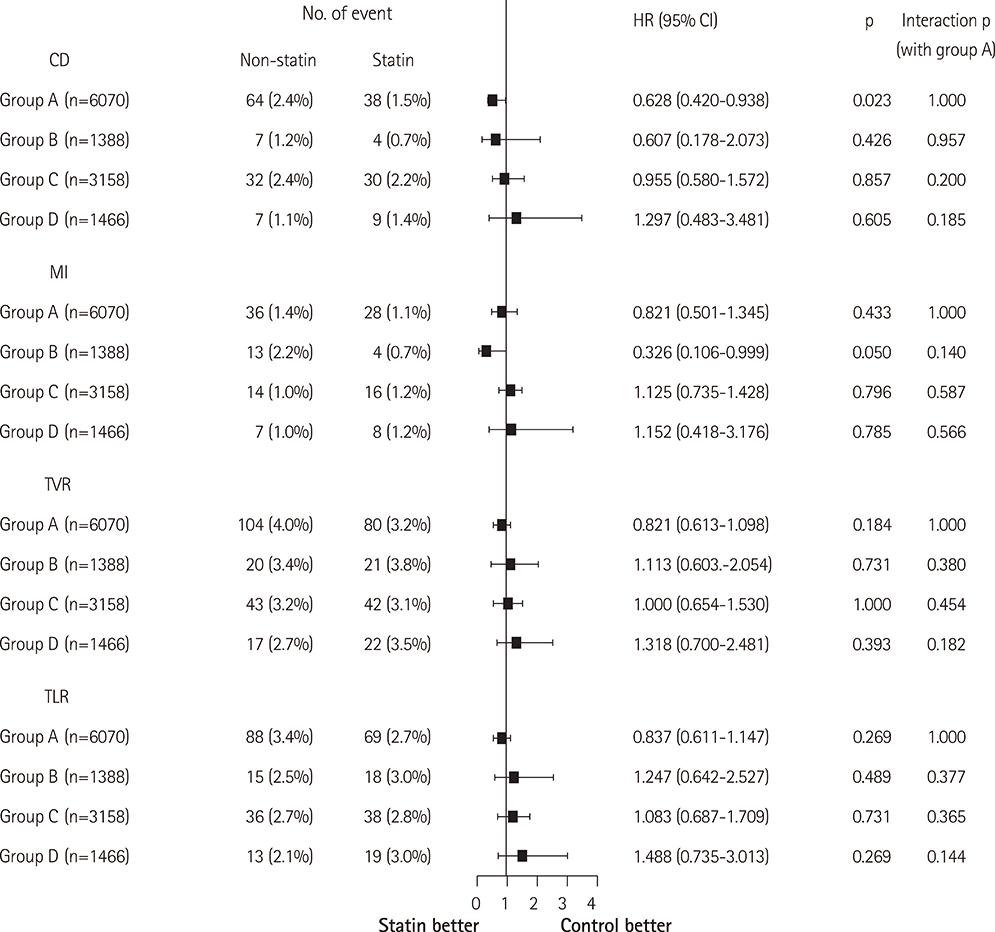
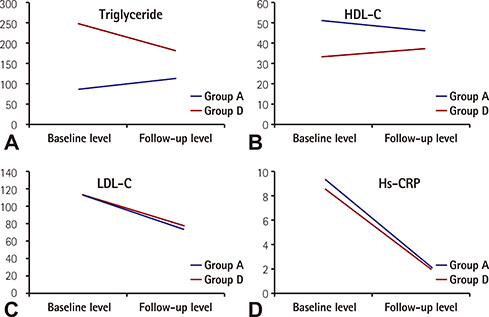
Statin therapy significantly reduced the risk of MACE in group A (hazard ratio=0.676; 95% confidence interval: 0.582-0.785; p<0.001). However, the efficacy of statin was not prominent in groups B, C, or D. In a propensity-matched population, the result was similar. In particular, the benefit of statin in group A was different compared with group D (interaction p=0.042)
CONCLUSION
The benefit of statin in patients with MI was different according to the presence or absence of dyslipidemia. In particular, because of the insufficient benefit of statin in patients with MI and dyslipidemia, a different lipid-lowering strategy is necessary in these patients.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
The Long and Winding Road: To the Proper Understanding of High-density Lipoprotein
Jidong Sung
Korean Circ J. 2020;50(3):248-249. doi: 10.4070/kcj.2020.0020.Implementation of National Health Policy for the Prevention and Control of Cardiovascular Disease in South Korea: Regional-Local Cardio-Cerebrovascular Center and Nationwide Registry
Ju Mee Wang, Byung Ok Kim, Jang-Whan Bae, Dong-Jin Oh
Korean Circ J. 2021;51(5):383-398. doi: 10.4070/kcj.2021.0001.Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes Metab J. 2023;47(1):59-71. doi: 10.4093/dmj.2021.0320.
Reference
-
1. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366:1267–1278.2. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Atorvastatin for acute coronary syndromes. JAMA. 2001; 286:533–535.3. Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004; 350:1495–1504.4. Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996; 335:1001–1009.5. Lee KH, Jeong MH, Kim HM, et al. Benefit of early statin therapy in patients with acute myocardial infarction who have extremely low low-density lipoprotein cholesterol. J Am Coll Cardiol. 2011; 58:1664–1671.6. Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008; 359:2195–2207.7. Huxley RR, Barzi F, Lam TH, et al. Isolated low levels of high-density lipoprotein cholesterol are associated with an increased risk of coronary heart disease: an individual participant data meta-analysis of 23 studies in the Asia-Pacific region. Circulation. 2011; 124:2056–2064.8. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012; 126:2020–2035.9. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2013; 82:E1–E27.10. Giraldez RR, Giugliano RP, Mohanavelu S, et al. Baseline low-density lipoprotein cholesterol is an important predictor of the benefit of intensive lipid-lowering therapy: a PROVE IT-TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction 22) analysis. J Am Coll Cardiol. 2008; 52:914–920.11. Emerging Risk Factors Collaboration. Di Angelantonio E, Sarwar N, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009; 302:1993–2000.12. Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002; 360:7–22.13. Colquhoun D, Keech A, Hunt D, et al. Effects of pravastatin on coronary events in 2073 patients with low levels of both low-density lipoprotein cholesterol and high- density lipoprotein cholesterol: results from the LIPID study. Eur Heart J. 2004; 25:771–777.14. Ballantyne CM, Olsson AG, Cook TJ, Mercuri MF, Pedersen TR, Kjekshus J. Influence of low high-density lipoprotein cholesterol and elevated triglyceride on coronary heart disease events and response to simvastatin therapy in 4S. Circulation. 2001; 104:3046–3051.15. Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005; 366:1849–1861.16. ACCORD Study Group. Ginsberg HN, Elam MB, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1563–1574.17. Brown BG, Zhao XQ, Chait A, et al. Simvastatin and niacin, antioxidant vitamins, or the combination for the prevention of coronary disease. N Engl J Med. 2001; 345:1583–1592.18. Brown G, Albers JJ, Fisher LD, et al. Regression of coronary artery disease as a result of intensive lipid-lowering therapy in men with high levels of apolipoprotein B. N Engl J Med. 1990; 323:1289–1298.19. Whitney EJ, Krasuski RA, Personius BE, et al. A randomized trial of a strategy for increasing high-density lipoprotein cholesterol levels: effects on progression of coronary heart disease and clinical events. Ann Intern Med. 2005; 142:95–104.20. Niesor EJ, Magg C, Ogawa N, et al. Modulating cholesteryl ester transfer protein activity maintains efficient pre-β-HDL formation and increases reverse cholesterol transport. J Lipid Res. 2010; 51:3443–3454.21. Nicholls SJ, Brewer HB, Kastelein JJ, et al. Effects of the CETP inhibitor evacetrapib administered as monotherapy or in combination with statins on HDL and LDL cholesterol: a randomized controlled trial. JAMA. 2011; 306:2099–2109.22. Daskalopoulou SS, Delaney JA, Filion KB, Brophy JM, Mayo NE, Suissa S. Discontinuation of statin therapy following an acute myocardial infarction: a population-based study. Eur Heart J. 2008; 29:2083–2091.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differences in the Korea Acute Myocardial Infarction Registry Compared with Western Registries
- Clinical Benefit of Statins in Korean Patients with Acute Myocardial Infarction: Experience of the Korea Acute Myocardial Infarction Registry
- Management of Dyslipidemia according to the 2015 Treatment Guideline for Diabetes: Controversies and Issues to Resolve
- Drug treatment of dyslipidemia
- Serum Lipid Changes during the Acute Phase of Acute Myocardial Infaction