A New MRI Grading System for Cervical Foraminal Stenosis Based on Axial T2-Weighted Images
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Institute of Radiation Medicine, Seoul National University Medical Research Center, Seongnam 13620, Korea. joonwoo2@gmail.com
- 2Department of Radiology, SMG-SNU Boramae Medical Center, Seoul 07061, Korea.
- 3Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 03080, Korea.
- 4Department of Radiology, University of Pittsburgh Medical Center, Pittsburgh, PA 15213, USA.
- KMID: 2344284
- DOI: http://doi.org/10.3348/kjr.2015.16.6.1294
Abstract
OBJECTIVE
The purpose of this study was to evaluate the reliability of a new magnetic resonance imaging (MRI) grading system for cervical neural foraminal stenosis (NFS).
MATERIALS AND METHODS
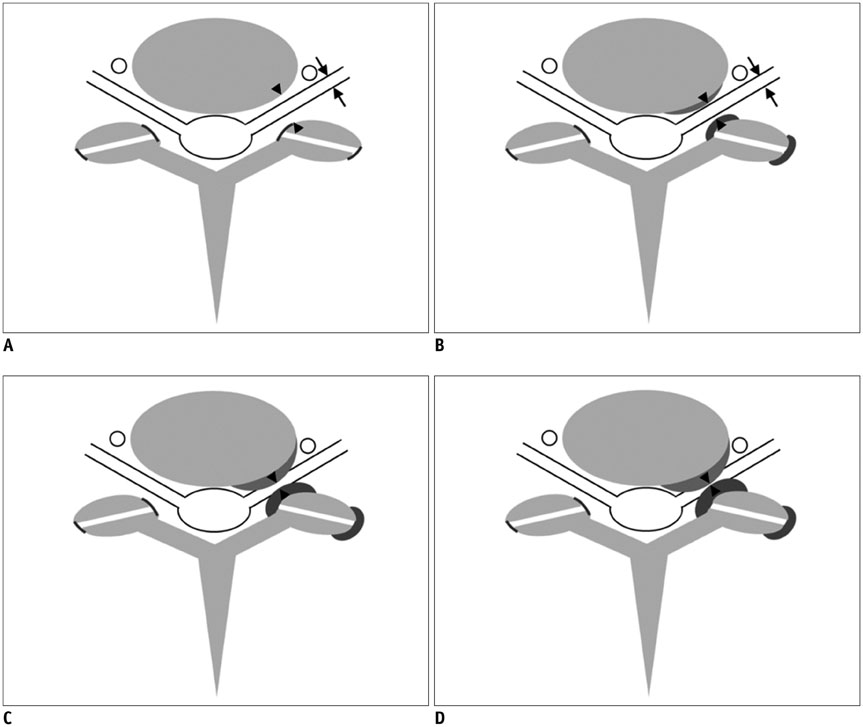
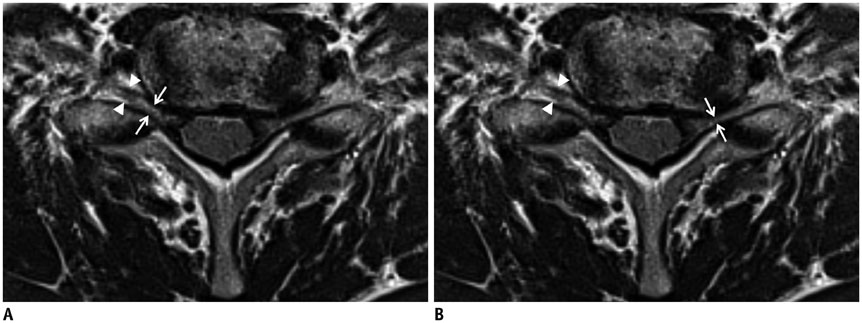
Cervical NFS at bilateral C4/5, C5/6, and C6/7 was classified into the following three grades based on the T2-weighted axial images: Grade 0 = absence of NFS, with the narrowest width of the neural foramen greater than the width of the extraforaminal nerve root (EFNR); Grade 1 = the narrowest width of the neural foramen the same or less than (but more than 50% of) the width of the EFNR; Grade 2 = the width of the neural foramen the same or less than 50% of the width of the EFNR. The MRIs of 96 patients who were over 60 years old (M:F = 50:46; mean age 68.4 years; range 61-86 years) were independently analyzed by seven radiologists. Interobserver and intraobserver agreements were analyzed using the percentage agreement, kappa statistics, and intraclass correlation coefficient (ICC).
RESULTS
For the distinction among the three individual grades at all six neural foramina, the ICC ranged from 0.68 to 0.73, indicating fair to good reproducibility. The percentage agreement ranged from 60.2% to 70.6%, and the kappa values (κ = 0.50-0.58) indicated fair to moderate agreement. The percentages of intraobserver agreement ranged from 85.4% to 93.8% (κ = 0.80-0.92), indicating near perfect agreement.
CONCLUSION
The new MRI grading system shows sufficient interobserver and intraobserver agreement to reliably assess cervical NFS.
MeSH Terms
Figure
Cited by 3 articles
-
Prognostic Value of Radiologic Extranodal Extension in Human Papillomavirus-Related Oropharyngeal Squamous Cell Carcinoma
Boeun Lee, Young Jun Choi, Seon-Ok Kim, Yoon Se Lee, Jung Yong Hong, Jung Hwan Baek, Jeong Hyun Lee
Korean J Radiol. 2019;20(8):1266-1274. doi: 10.3348/kjr.2018.0742.Facet Joint Versus Transforaminal Epidural Steroid Injections in Patients With Cervical Radicular Pain due to Foraminal Stenosis: A Retrospective Comparative Study
Ji Seon Chae, Won-joong Kim, Mi Jin Jue
J Korean Med Sci. 2022;37(25):e208. doi: 10.3346/jkms.2022.37.e208.Association between fatty infiltration in the cervical multifidus and treatment response following cervical interlaminar epidural steroid injection
Hyun-Jung Kwon, Chan-Sik Kim, Sungwon Kim, Syn Hae Yoon, Jungho Koh, Young Ki Kim, Seong-Soo Choi, Jin-Woo Shin, Doo-Hwan Kim
Korean J Pain. 2023;36(3):358-368. doi: 10.3344/kjp.23092.
Reference
-
1. Wainner RS, Gill H. Diagnosis and nonoperative management of cervical radiculopathy. J Orthop Sports Phys Ther. 2000; 30:728–744.2. Yousem DM, Atlas SW, Goldberg HI, Grossman RI. Degenerative narrowing of the cervical spine neural foramina: evaluation with high-resolution 3DFT gradient-echo MR imaging. AJNR Am J Neuroradiol. 1991; 12:229–236.3. Abbed KM, Coumans JV. Cervical radiculopathy: pathophysiology, presentation, and clinical evaluation. Neurosurgery. 2007; 60(1 Supp1 1):S28–S34.4. Modic MT, Masaryk TJ, Mulopulos GP, Bundschuh C, Han JS, Bohlman H. Cervical radiculopathy: prospective evaluation with surface coil MR imaging, CT with metrizamide, and metrizamide myelography. Radiology. 1986; 161:753–759.5. Russell EJ. Cervical disk disease. Radiology. 1990; 177:313–325.6. Jahnke RW, Hart BL. Cervical stenosis, spondylosis, and herniated disc disease. Radiol Clin North Am. 1991; 29:777–791.7. Yousem DM, Atlas SW, Hackney DB. Cervical spine disk herniation: comparison of CT and 3DFT gradient echo MR scans. J Comput Assist Tomogr. 1992; 16:345–351.8. Ryan AG, Morrissey BM, Newcombe RG, Halpin SF, Hourihan MD. Are T1 weighted images helpful in MRI of cervical radiculopathy? Br J Radiol. 2004; 77:189–196.9. Bartlett RJ, Hill CR, Gardiner E. A comparison of T2 and gadolinium enhanced MRI with CT myelography in cervical radiculopathy. Br J Radiol. 1998; 71:11–19.10. Modic MT, Masaryk TJ, Ross JS, Mulopulos GP, Bundschuh CV, Bohlman H. Cervical radiculopathy: value of oblique MR imaging. Radiology. 1987; 163:227–231.11. Shim JH, Park CK, Lee JH, Choi JW, Lee DC, Kim DH, et al. A comparison of angled sagittal MRI and conventional MRI in the diagnosis of herniated disc and stenosis in the cervical foramen. Eur Spine J. 2009; 18:1109–1116.12. Park HJ, Kim SS, Lee SY, Park NH, Chung EC, Rho MH, et al. A practical MRI grading system for cervical foraminal stenosis based on oblique sagittal images. Br J Radiol. 2013; 86:20120515.13. Park HJ, Kim SS, Han CH, Lee SY, Chung EC, Kim MS, et al. The clinical correlation of a new practical MRI method for grading cervical neural foraminal stenosis based on oblique sagittal images. AJR Am J Roentgenol. 2014; 203:412–417.14. Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990; 72:1178–1184.15. Humphreys SC, Hodges SD, Patwardhan A, Eck JC, Covington LA, Sartori M. The natural history of the cervical foramen in symptomatic and asymptomatic individuals aged 20-60 years as measured by magnetic resonance imaging. A descriptive approach. Spine (Phila Pa 1976). 1998; 23:2180–2184.16. Lee MJ, Riew KD. The prevalence cervical facet arthrosis: an osseous study in a cadveric population. Spine J. 2009; 9:711–714.17. Tanaka N, Fujimoto Y, An HS, Ikuta Y, Yasuda M. The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine (Phila Pa 1976). 2000; 25:286–291.18. Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005; 85:257–268.19. Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003; 228:303–308.20. Kang Y, Lee JW, Koh YH, Hur S, Kim SJ, Chai JW, et al. New MRI grading system for the cervical canal stenosis. AJR Am J Roentgenol. 2011; 197:W134–W140.21. Park HJ, Kim SS, Lee YJ, Lee SY, Park NH, Choi YJ, et al. Clinical correlation of a new practical MRI method for assessing central lumbar spinal stenosis. Br J Radiol. 2013; 86:20120180.22. Rosner B. Fundamentals of Biostatistics. 7th ed. Canada: Cengage Learning;2010.23. Song KJ, Choi BW, Kim GH, Kim JR. Clinical usefulness of CT-myelogram comparing with the MRI in degenerative cervical spinal disorders: is CTM still useful for primary diagnostic tool? J Spinal Disord Tech. 2009; 22:353–357.24. Park MS, Moon SH, Lee HM, Kim TH, Oh JK, Lee SY, et al. Diagnostic value of oblique magnetic resonance images for evaluating cervical foraminal stenosis. Spine J. 2015; 15:607–611.25. Shin HY, Park JK, Park SK, Jung GS, Choi YS. Variations in Entrance of Vertebral Artery in Korean Cervical Spine: MDCT-based Analysis. Korean J Pain. 2014; 27:266–270.26. Bruneau M, Cornelius JF, Marneffe V, Triffaux M, George B. Anatomical variations of the V2 segment of the vertebral artery. Neurosurgery. 2006; 59:1 Suppl 1. ONS20–ONS24. discussion ONS20-ONS2427. Rawal JD, Jadav HR. Anatomical study of variation of vertebral artery entering the foramen transversarium of cervical vertebrae. Natl J Med Res. 2012; 2:199–201.28. Kitagawa T, Fujiwara A, Kobayashi N, Saiki K, Tamai K, Saotome K. Morphologic changes in the cervical neural foramen due to flexion and extension: in vivo imaging study. Spine (Phila Pa 1976). 2004; 29:2821–2825.29. Vitaz TW, Shields CB, Raque GH, Hushek SG, Moser R, Hoerter N, et al. Dynamic weight-bearing cervical magnetic resonance imaging: technical review and preliminary results. South Med J. 2004; 97:456–461.30. Jinkins JR, Dworkin JS, Damadian RV. Upright, weight-bearing, dynamic-kinetic MRI of the spine: initial results. Eur Radiol. 2005; 15:1815–1825.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging Grading Systems for Central Canal and Neural Foraminal Stenoses of the Lumbar and Cervical Spines With a Focus on the Lee Grading System
- Correlation between MRI Grading System and Surgical Findings for Lumbar Foraminal Stenosis
- Usefulness of Coronal MR Image in Diagnosis of Foraminal and Extraforaminal Disc Herniation
- Clinical Utility of Limited T2-Weighted-Only Lumbar Spine MRI in Pain Intervention Clinics
- MRI Findings of Central Nervous System Granulocytic Sarcoma (Chloroma)