J Korean Med Sci.
2015 Sep;30(9):1354-1360. 10.3346/jkms.2015.30.9.1354.
Epidemiological and Survival Trends of Pediatric Cardiac Arrests in Emergency Departments in Korea: A Cross-sectional, Nationwide Report
- Affiliations
-
- 1Department of Emergency Medicine, School of Medicine, Kyungpook National University, Daegu, Korea. emmam@knu.ac.kr
- 2Department of Emergency Medicine, Wonju College of Medicine, Yonsei University, Wonju, Korea.
- 3National Emergency Medical Center, Seoul, Korea.
- 4Department of Emergency Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 5The Korean Association of Cardiopulmonary Resuscitation, Seoul, Korea.
- KMID: 2344164
- DOI: http://doi.org/10.3346/jkms.2015.30.9.1354
Abstract
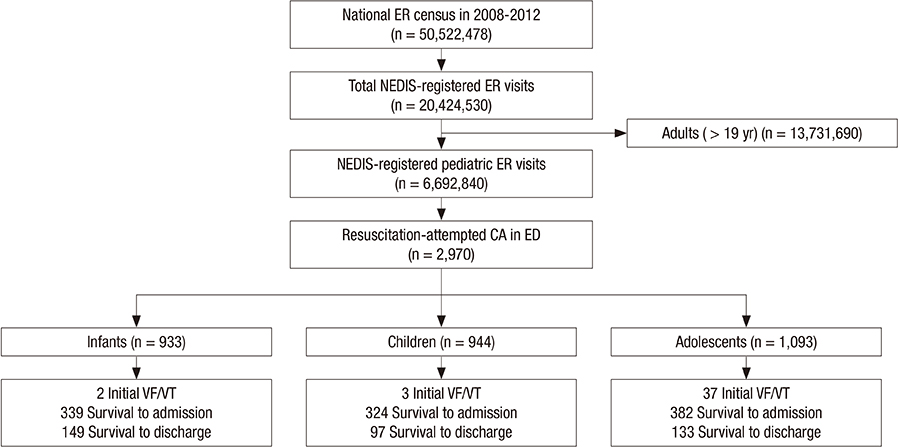
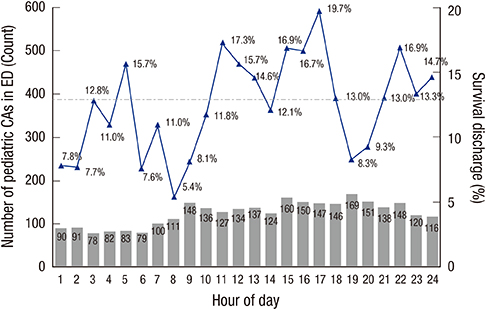
- Cardiac arrest (CA) in children is associated with high mortality rates. In Korea, cohort studies regarding the outcomes of pediatric CAs are lacking, especially in emergency departments (EDs) or in-hospital settings. This study was conducted to examine the trends in epidemiology and survival outcomes in children with resuscitation-attempted CAs using data from a cross-sectional, national, ED-based clinical registry. We extracted cases in which cardiopulmonary resuscitation and/or manual defibrillation were performed according to treatment codes using the National Emergency Department Information System (NEDIS) from 2008 to 2012. The total number of ED visits registered in the NEDIS during the 5-yr evaluation period was 20,424,530; among these, there were 2,970 resuscitation-attempted CAs in children. The annual rates of pediatric CAs per 1,000 ED visits showed an upward trend from 2.81 in 2009 to 3.62 in 2012 (P for trend = 0.045). The median number of estimated pediatric CAs at each ED was 7.8 (25th to 75th percentile, 4 to 13) per year. The overall rates for admission survival and discharge survival were 35.2% and 12.8%, respectively. The survival outcome of adults increased substantially over the past 5 yr (11.8% in 2008, 11.7% in 2010, and 13.6% in 2012; P for trend = 0.001); however, the results for children did not improve (13.6% in 2008, 11.4% in 2010, and 13.7% in 2012; P for trend = 0.870). Conclusively, we found that the overall incidence of pediatric CAs in EDs increased substantially over the past 5 yr, but without significantly higher survival outcomes.
MeSH Terms
-
Adolescent
Cardiopulmonary Resuscitation/*mortality
Child
Child, Preschool
Cross-Sectional Studies
Emergency Service, Hospital/*statistics & numerical data
Female
Heart Arrest/*epidemiology/*prevention & control
*Hospital Mortality
Humans
Incidence
Infant
Male
*Registries
Republic of Korea/epidemiology
Risk Factors
Survival Rate
Treatment Outcome
Young Adult
Figure
Reference
-
1. Woods WA. Pediatric resuscitation and cardiac arrest. Emerg Med Clin North Am. 2012; 30:153–168.2. Young KD, Gausche-Hill M, McClung CD, Lewis RJ. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics. 2004; 114:157–164.3. Herlitz J, Svensson L, Engdahl J, Gelberg J, Silfverstolpe J, Wisten A, Angquist KA, Holmberg S. Characteristics of cardiac arrest and resuscitation by age group: an analysis from the Swedish Cardiac Arrest Registry. Am J Emerg Med. 2007; 25:1025–1031.4. Meert KL, Donaldson A, Nadkarni V, Tieves KS, Schleien CL, Brilli RJ, Clark RS, Shaffner DH, Levy F, Statler K, et al. Pediatric Emergency Care Applied Research Network. Multicenter cohort study of in-hospital pediatric cardiac arrest. Pediatr Crit Care Med. 2009; 10:544–553.5. Park CB, Shin SD, Suh GJ, Ahn KO, Cha WC, Song KJ, Kim SJ, Lee EJ, Ong ME. Pediatric out-of-hospital cardiac arrest in Korea: A nationwide population-based study. Resuscitation. 2010; 81:512–517.6. Lee MJ. Incidence and outcome of cardiac arrest in Korea. J Korean Soc Emerg Med. 2012; 23:168–180.7. Kim WJ, Kim JJ, Jang JH, Hyun SY, Yang HJ, Lee G. Implementation of therapeutic hypothermia after pediatric out-of hospital cardiac arrest in one tertiary emergency center. Korean J Crit Care Med. 2013; 28:25–32.8. Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, et al. National Registry of Cardiopulmonary Resuscitation Investigators. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006; 295:50–57.9. Johnson NJ, Salhi RA, Abella BS, Neumar RW, Gaieski DF, Carr BG. Emergency department factors associated with survival after sudden cardiac arrest. Resuscitation. 2013; 84:292–297.10. Cho H, Moon S, Park SJ, Han G, Park JH, Lee H, Choi J, Hwang S, Bobrow BJ. Out-of-hospital cardiac arrest: incidence, process of care, and outcomes in an urban city, Korea. Clin Exp Emerg Med. 2014; 1:94–100.11. Kwak YH, Kim DK, Jang HY. Utilization of emergency department by children in Korea. J Korean Med Sci. 2012; 27:1222–1228.12. Tunstall-Pedoe H, Bailey L, Chamberlain DA, Marsden AK, Ward ME, Zideman DA. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): methods and overall results. BMJ. 1992; 304:1347–1351.13. Valderrama AL, Fang J, Merritt RK, Hong Y. Cardiac arrest patients in the emergency department-National Hospital Ambulatory Medical Care Survey, 2001-2007. Resuscitation. 2011; 82:1298–1301.14. Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, Meaney PA, Cen L, Nadkarni VM, Praestgaard AH, et al. National Registry of Cardiopulmonary Resuscitation Investigators. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008; 299:785–792.15. Ro YS, Shin SD, Song KJ, Lee EJ, Kim JY, Ahn KO, Chung SP, Kim YT, Hong SO, Choi JA, et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: a nationwide observational study from 2006 to 2010 in South Korea. Resuscitation. 2013; 84:547–557.16. Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009; 80:30–34.17. Nakanishi N, Nishizawa S, Kitamura Y, Nakamura T, Matsumuro A, Sawada T, Matsubara H. Circadian, weekly, and seasonal mortality variations in out-of-hospital cardiac arrest in Japan: analysis from AMI-Kyoto Multicenter Risk Study database. Am J Emerg Med. 2011; 29:1037–1043.18. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. American Heart Association Statistics Committee. Stroke Statistics Subcommittee. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013; 127:e6–e245.19. Kim HJ, Kim KI, Cho YS, Kang J, Park JJ, Oh IY, Yoon CH, Suh JW, Youn TJ, Chae IH, et al. The effect of admission at weekends on clinical outcomes in patients with non-ST-segment elevation acute coronary syndrome and its contributing factors. J Korean Med Sci. 2015; 30:414–425.20. Yang HJ, Kim GW, Kim H, Cho JS, Rho TH, Yoon HD, Lee MJ. NEDIS-CA Consortium. Epidemiology and outcomes in out-of-hospital cardiac arrest: a report from the NEDIS-based cardiac arrest registry in Korea. J Korean Med Sci. 2015; 30:95–103.21. Jayaram N, Spertus JA, Nadkarni V, Berg RA, Tang F, Raymond T, Guerguerian AM, Chan PS. American Heart Association's Get with the Guidelines-Resuscitation Investigators. Hospital variation in survival after pediatric in-hospital cardiac arrest. Circ Cardiovasc Qual Outcomes. 2014; 7:517–523.22. Zeng J, Qian S, Zheng M, Wang Y, Zhou G, Wang H. The epidemiology and resuscitation effects of cardiopulmonary arrest among hospitalized children and adolescents in Beijing: an observational study. Resuscitation. 2013; 84:1685–1690.23. Kayser RG, Ornato JP, Peberdy MA. American Heart Association National Registry of Cardiopulmonary Resuscitation. Cardiac arrest in the Emergency Department: a report from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2008; 78:151–160.24. Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS. American Heart Association Get With the Guidelines-Resuscitation Investigators. Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes. 2013; 6:42–49.25. Nagata T, Abe T, Noda E, Hasegawa M, Hashizume M, Hagihara A. Factors associated with the clinical outcomes of paediatric out-of-hospital cardiac arrest in Japan. BMJ Open. 2014; 4:e003481.26. Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RA. Resuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009; 119:1484–1491.27. Ro YS, Shin SD, Song KJ, Park CB, Lee EJ, Ahn KO, Cho SI. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low- and high-resuscitation case volume. Resuscitation. 2012; 83:855–861.28. López-Herce J, García C, Rodríguez-Núñez A, Domínguez P, Carrillo A, Calvo C, Delgado MA. Spanish Study Group of Cardiopulmonary Arrest in Children. Long-term outcome of paediatric cardiorespiratory arrest in Spain. Resuscitation. 2005; 64:79–85.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Out-of-hospital cardiac arrest: incidence, patient characteristics, outcomes, and trends over time between 2012 and 2018 in an urban city
- The comparisons of prehospital treatments in traumatic and non-traumatic out-of-hospital cardiac arrests
- Cardiac Arrest in the Operating Room
- First Survival Case of an Out-of-Hospital Cardiac Arrest Patient Shocked using a Public-Access Automated External Defibrillator in Korea
- Analysis of the factors associated with survival to hospital discharge in adult patients with cardiac arrest in the emergency department