J Korean Ophthalmol Soc.
2013 Oct;54(10):1610-1613.
A Case of Intravitreal Cysticercosis with Neovascular Glaucoma
- Affiliations
-
- 1Department of Ophthalmology, EYE and ENT Hospital, Severance Hospital, The Institute of Vision Research, Yonsei University College of Medicine, Seoul, Korea. shbyeon@yuhs.ac
- 2Siloam Eye Hospital, Seoul, Korea.
Abstract
- PURPOSE
To introduce a case of intravitreal cysticercosis presenting as neovascular glaucoma.
CASE SUMMARY
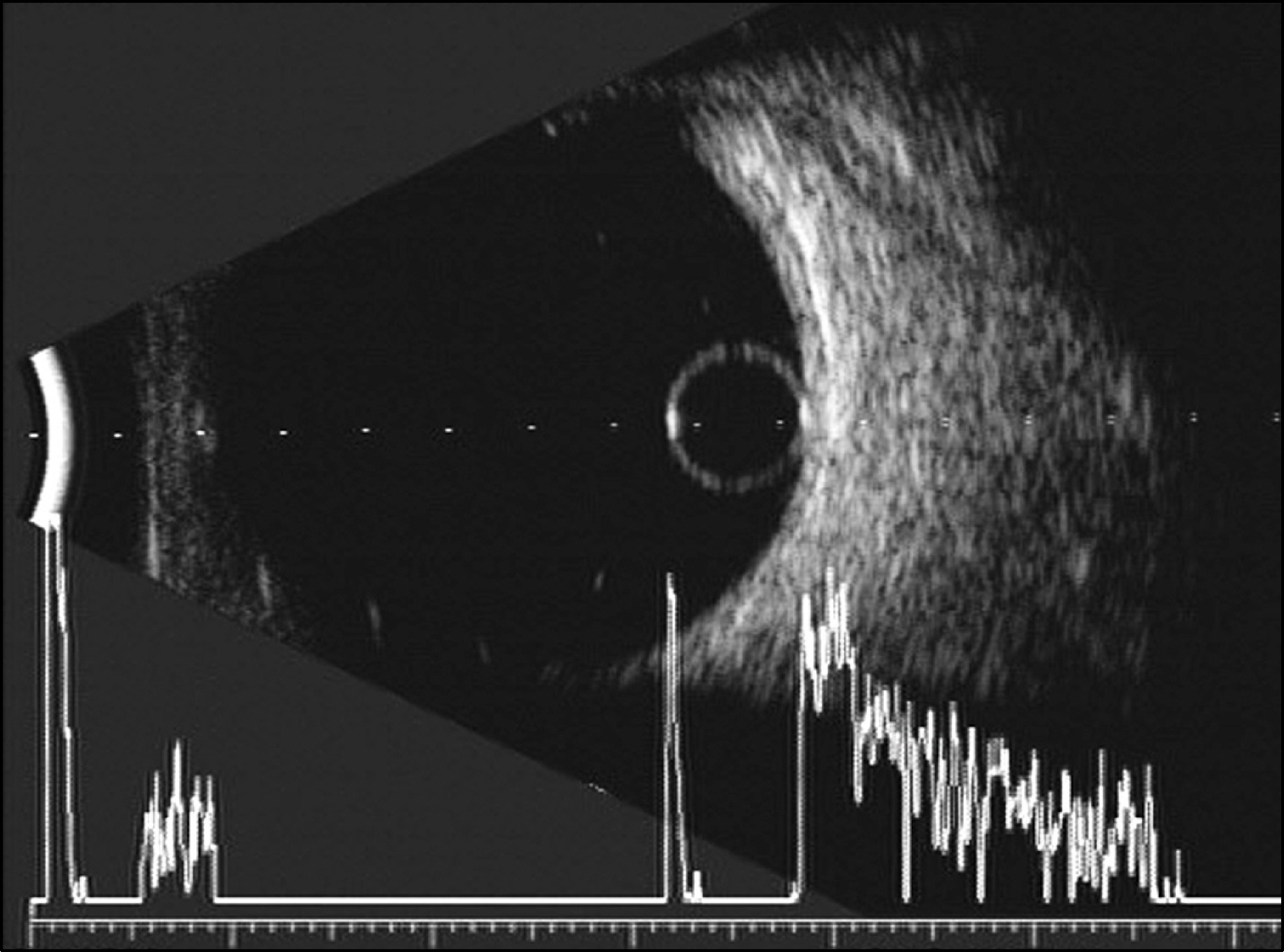
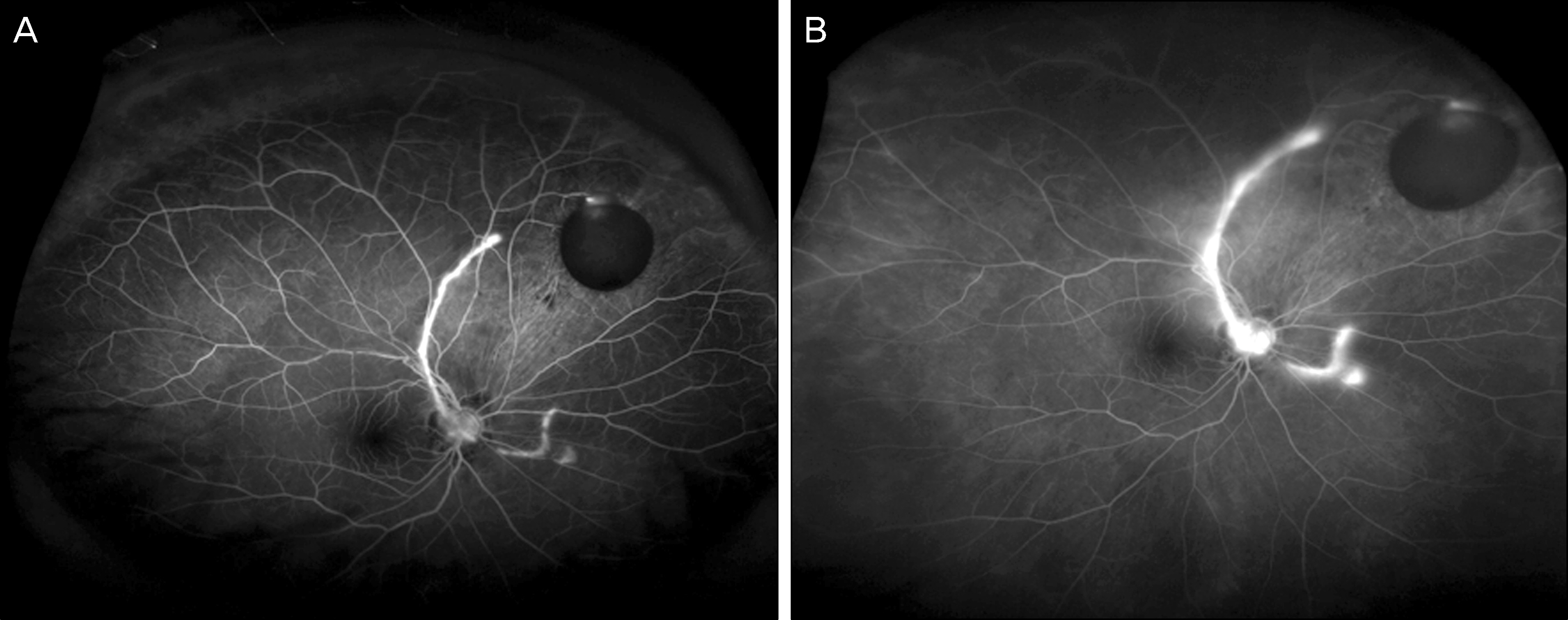
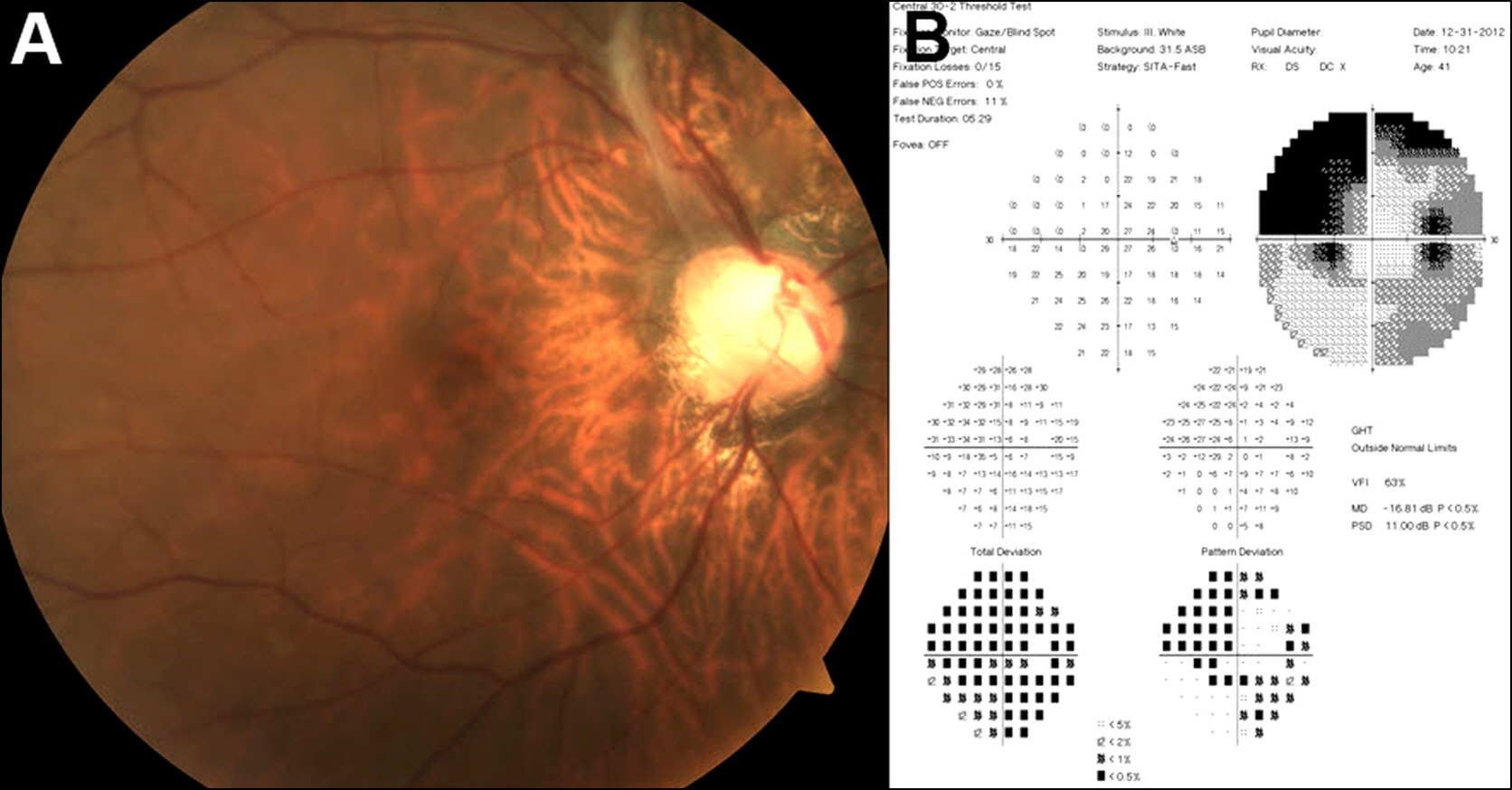
A 42-year-old female who lives in the Philippines visited our clinic complaining of reduced visual acuity and decreased visual field in her right eye. She was treated at another clinic for neovascular glaucoma and posterior uveitis. Initial best-corrected visual acuity was 0.7 and intraocular pressure was 13 mm Hg with Goldmann applanation tonometry. Slit lamp examination showed inflammatory cells in the anterior chamber and vitreous with florid new vessel on iris. On fundus examination, a cystic lesion without movement was observed in the superonasal vitreous as well as tractional band. As other retinal vascular diseases were not observed on fluorescein angiography, the patient was diagnosed with secondary neovascular glaucoma due to cysticercosis. After a single course of intravitreal bevacizumab injection and cyst removal with pars plana vitrectomy, the best-corrected visual acuity was 0.5 and intraocular pressure was 14 mm Hg without recurrence of iris neovascularization during the 3 months of follow-up.
MeSH Terms
-
Adult
Anterior Chamber
Antibodies, Monoclonal, Humanized
Cysticercosis*
Eye
Female
Fluorescein Angiography
Follow-Up Studies
Glaucoma, Neovascular*
Humans
Intraocular Pressure
Iris
Manometry
Philippines
Recurrence
Retinaldehyde
Traction
Uveitis, Posterior
Vascular Diseases
Visual Acuity
Visual Fields
Vitrectomy
Bevacizumab
Antibodies, Monoclonal, Humanized
Retinaldehyde
Figure
Reference
-
References
1. Sharma T, Sinha S, Shah N. . Intraocular cysticercosis: clinical characteristics and visual outcome after vitreoretinal surgery. Ophthalmology. 2003; 110:996–1004.
Article2. Pushker N, Bajaj MS, Chandra M. Neena. Ocular and orbital cysticercosis. Acta Ophthalmol Scand. 2001; 79:408–13.3. Chung YT. Two cases of cysticercosis in the vitreous body. J Korean Ophthalmol Soc. 1973; 14:383–6.4. Choi CS, Rhee JW. A case of subretinal cysticercosis. J Korean Ophthalmol Soc. 1966; 7:101–3.5. Sohn CK, Hong SH, Lee KC, Choe JK. A case of surgically extracted cysticercus cellulosae from the anterior chamber and three cases of subconjunctival cysticercosis cellulosae. J Korean Ophthalmol Soc. 1967; 8:25–9.6. Ahn BH, Lee JH, Lee JH. Intraocular cysticercosis. J Korean Ophthalmol Soc. 1975; 16:209–15.7. Seo MS, Woo JM, Park YG. Intravitreal cysticercosis. Korean J Ophthalmol. 1996; 10:55–9.
Article8. Kruger-Leite E, Jalkh AE, Quiroz H, Schepens CL. Intraocular cysticercosis. Am J Ophthalmol. 1985; 99:252–7.
Article9. Ratra D, Phogat C, Singh M, Choudhari NS. Intravitreal cys- ticercosis presenting as neovascular glaucoma. Indian J Ophthalmol. 2010; 58:70–3.10. Gartner S, Henkind P. Neovascularization of the iris (rubeosis iridis). Surv Ophthalmol. 1978; 22:291–312.
Article11. Luger M, Stilma JS, Ringens PJ, van Baarlen J. In-toto removal of a subretinal Cysticercus cellulosae by pars plana vitrectomy. Br J Ophthalmol. 1991; 75:561–3.
Article12. Davidorf FH, Mouser JG, Derick RJ. Rapid improvement of ru- beosis iridis from a single bevacizumab (Avastin) injection. Retina. 2006; 26:354–6.13. Wakabayashi T, Oshima Y, Sakaguchi H. . Intravitreal bevacizumab to treat iris neovascularization and neovascular glaucoma secondary to ischemic retinal diseases in 41 consecutive cases. Ophthalmology. 2008; 115:1571–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Exacerbation of Neovascular Glaucoma after Carotid Artery Stenting
- Intravitreal Bevacizumab for the Treatment of Neovascular Glaucoma Associated With Central Retinal Artery Occlusion
- Intraviteal Bevacizumab (Avastin(R)) Injection for the Treatment of Early-Stage Neovascular Glaucoma
- Effect of Simultaneous Intravitreal Bevacizumab and Retrobulbar Triamcinolone Injection in Refractory Neovascular Glaucoma
- Intravitreal Bevacizumab (Avastin) Treatment of Neovascular Glaucoma in Ocular Ischemic Syndrome