J Korean Ophthalmol Soc.
2013 Oct;54(10):1546-1553.
Risk Factors for Retinal Pigment Epithelium Tears after Anti-VEGF Agent Injection in Age-Related Macular Degeneration
- Affiliations
-
- 1Sungmo Eye Hospital, Busan, Korea. heesyoon@dreamwiz.com
Abstract
- PURPOSE
Intravitreal anti-vascular endothelial growth factor (VEGF) treatment has become an important part in the treatment of neovascular age-related macular degeneration (AMD). In the present study we describe the clinical feature of retinal pigment epithelium (RPE) tears after intravitreal injection of anti-VEGF agent and compared the tear group to the control group.
METHODS
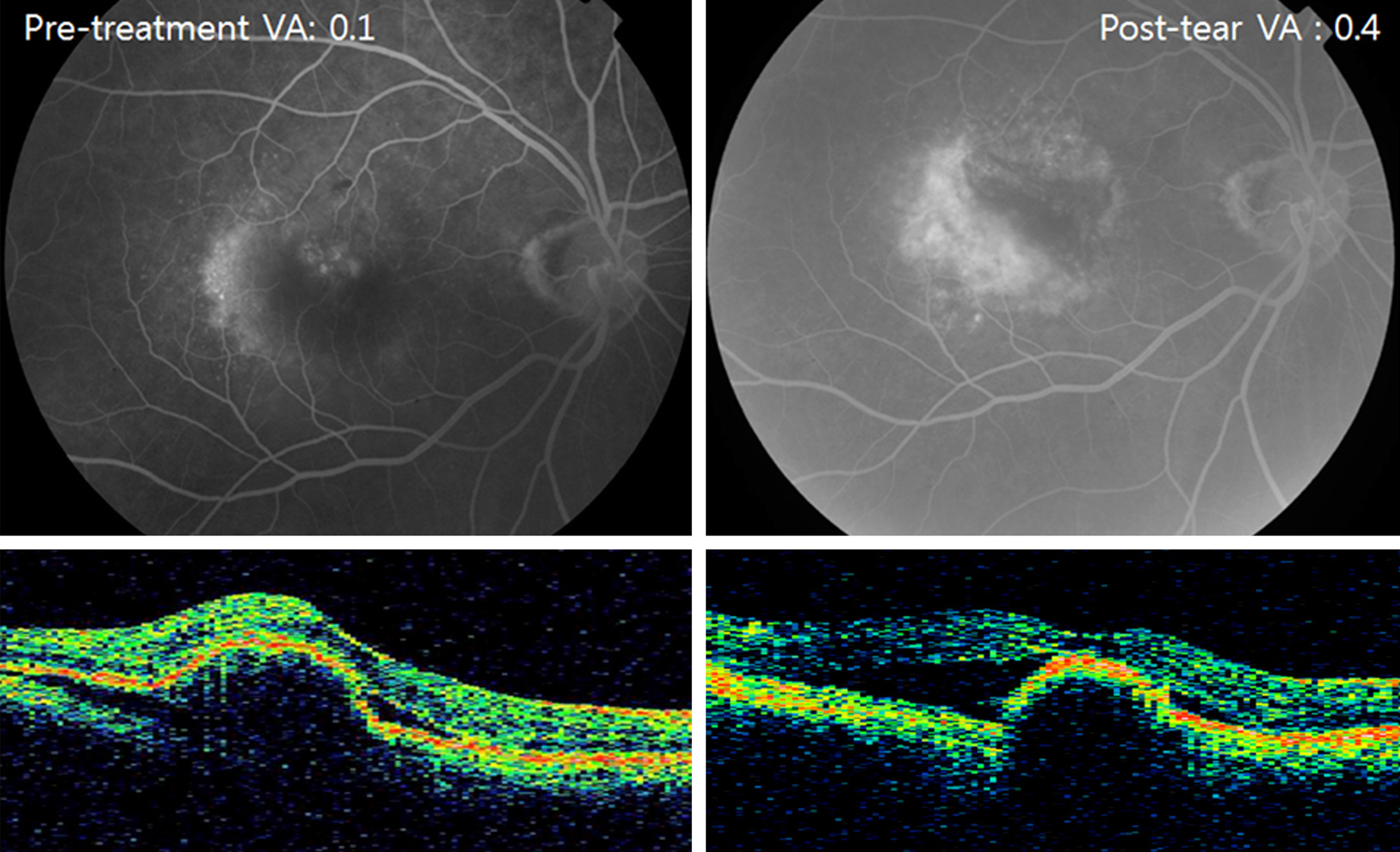
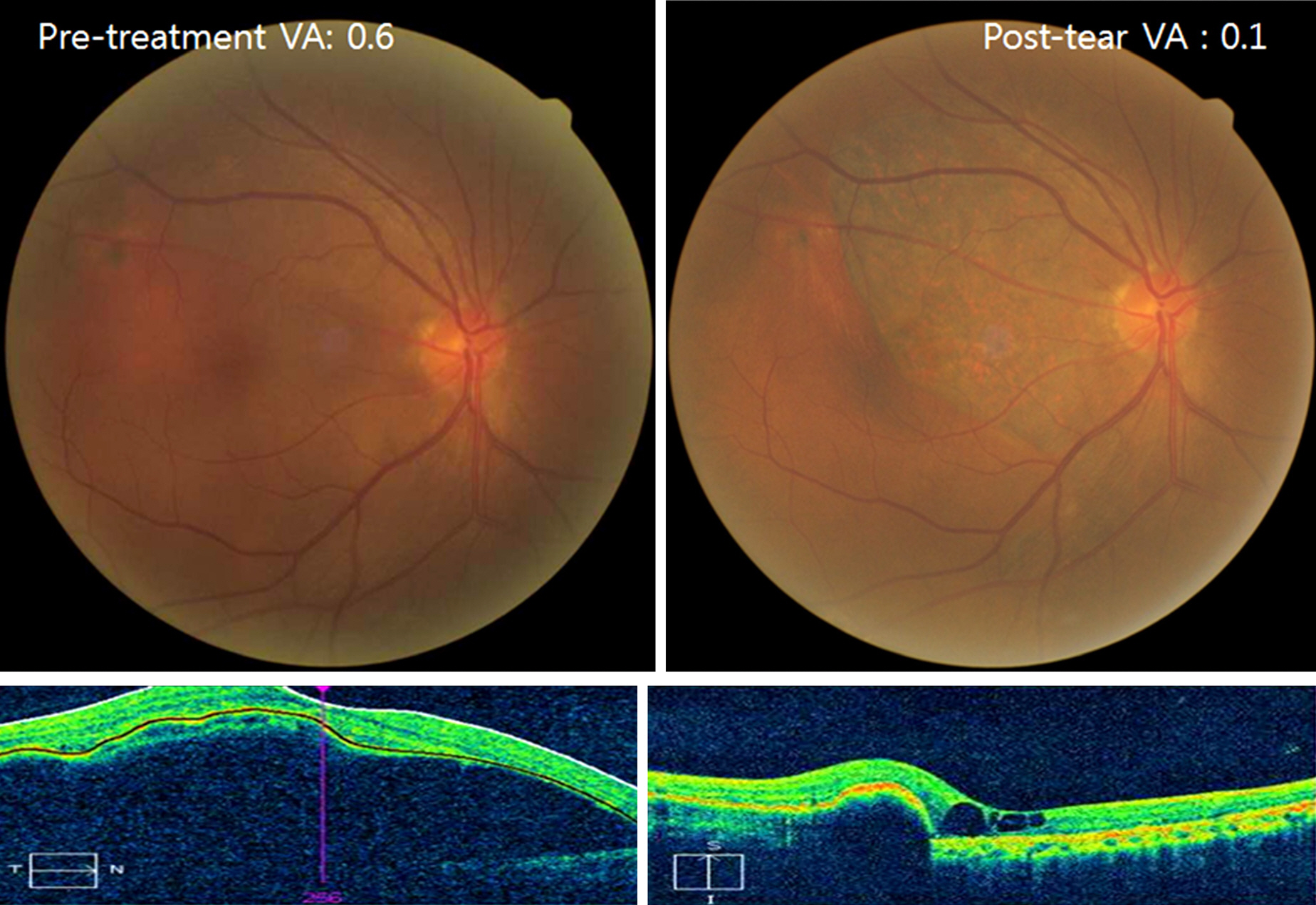
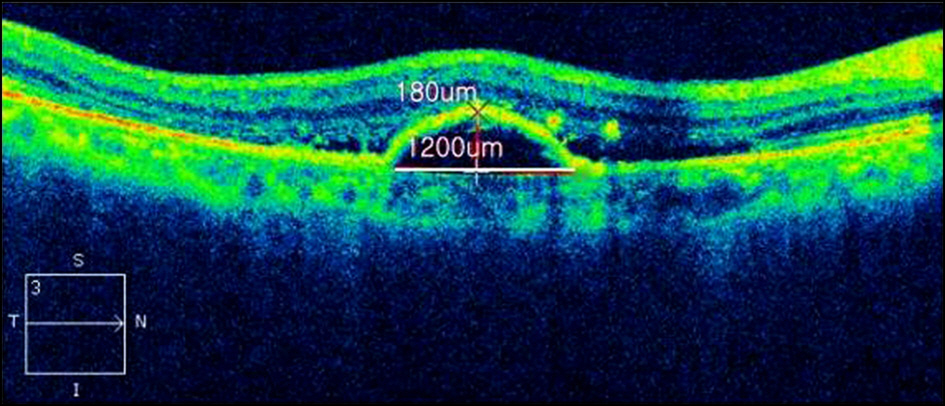
In this retrospective case series, data of 11 patients with eyes that developed RPE tears after intravitreal anti-VEGF injection (8 ranibizumab and 3 bevacizumab) were collected and analyzed. The tear group included 11 patients with eyes that developed RPE tears and the control group included 22 patients with no RPE tears after treatment. We investigated age, gender, bilaterality, duration from injection to tear, pigment epithelial detachment (PED) height and diameter, along with central retinal thickness (CMT) using optical coherence tomography (OCT), fluorescein angiography (FAG), and visual acuities before and after treatment.
RESULTS
The mean age of the tear group was 81.36 +/- 5.55 years which was significantly different from the control group's mean age of 74.82 +/- 5.28 years (p = 0.003). OCT findings showed PED greatest linear dimension (GLD) was 2978.45 +/- 947.69 microm in the tear group and 2250.23 +/- 988.49 microm in the control group (p = 0.027). PED height was 507.09 +/- 153.97 microm in the tear group and 353.23 +/- 199.42 microm in the control group (p = 0.010). CMT was 431.64 +/- 200.33 microm in the tear group and 289.95 +/- 61.27 microm in the control group (p = 0.005). There was no significant difference between groups according to gender, bilaterality, visual acuities, and subretinal fluid based on OCT and FAG findings. In the tear group, visual acuities before and after the tear were not significantly different.
CONCLUSIONS
Old age and eyes with high and wide PED appear to be more vulnerable to RPE tear. Further investigation with a larger number of patients is needed to further confirm these results.
Keyword
MeSH Terms
-
Antibodies, Monoclonal, Humanized
Endothelial Growth Factors
Eye
Fluorescein Angiography
Humans
Intravitreal Injections
Macular Degeneration*
Retinal Pigment Epithelium*
Retinaldehyde*
Retrospective Studies
Risk Factors*
Subretinal Fluid
Tomography, Optical Coherence
Visual Acuity
Bevacizumab
Ranibizumab
Antibodies, Monoclonal, Humanized
Endothelial Growth Factors
Retinaldehyde
Figure
Reference
-
References
1. Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Stydy. Ophthalmology. 1992; 99:933–43.2. Ferris FL 3rd, Fine SL, Hyman L. Age-related macular degeneration and blindness due to neovascular maculopathy. Arch Ophthalmol. 1984; 102:1640–2.
Article3. Adamis AP, Shima DT. The role of vascular endothelial growth factor in ocular health and disease. Retina. 2005; 25:111–8.
Article4. Ferrara N, Damico L, Shams N. . Development of ranibizumab, an anti-vascular endothelial growth factor antigen binding fragment, as therapy for neovascular age-related macular degeneration. Retina. 2006; 26:859–70.
Article5. Song MH, Kim JY, Roh YJ. Short-term efficacy of intravitreal ranibizumab for myopic choroidal neovascularization. J Korean Ophthalmol Soc. 2009; 50:1027–34.
Article6. Bashshur ZF, Haddad ZA, Schakal A. . Intravitreal bevacizumab for treatment of neovascular age-related macular degeneration: a one-year prospective study. Am J Ophthalmol. 2008; 145:249–56.
Article7. Mozayan A, Farah S. Acute anterior uveitis following intravitreal injection of bevacizumab. Ophthalmic Surg Lasers Imaging Retina. 2013; 44:25–7.
Article8. Skalicky SE, Ho I, Agar A, Bank A. Glaucoma filtration surgery following sustained elevation of intraocular pressure secondary to intravitreal anti-VEGF injections. Ophthalmic Surg Lasers Imaging. 2012; 43:328–34.
Article9. Jamrozy-Witkowska A, Kowalska K, Jankowska-Lech I. . [Complications of intravitreal injections–own experience]. Klin Oczna. 2011; 113(4-6):127–31.10. Hoskin A, Bird AC, Sehmi K. Tears of detached retinal pigment epithelium. Br J Ophthalmol. 1981; 65:417–22.
Article11. Meyer CH, Toth CA. Retinal pigment epithelial tear with vitre- omacular attachment: a novel pathogenic feature. Graefes Arch Clin Exp Ophthalmol. 2001; 239:325–33.12. Gamulescu MA, Framme C, Sachs H. RPE-rip after intravitreal bevacizumab (Avastin) treatment for vascularised PED secondary to AMD. Graefes Arch Clin Exp Ophthalmol. 2007; 245:1037–40.
Article13. Hartnett ME, Lappas A, Darland D. . Retinal pigment epithelium and endothelial cell interaction causes retinal pigment epithelial barrier dysfunction via a soluble VEGF-dependent mechanism. Exp Eye Res. 2003; 77:593–9.
Article14. Krishan NR, Chandra SR, Stevens TS. Diagnosis and pathogenesis of retinal pigment epithelial tears. Am J Ophthalmol. 1985; 100:698–707.
Article15. Cantrill HL, Ramsay RC, Knobloch WH. Rips in the pigment epithelium. Arch Ophthalmol. 1983; 101:1074–9.
Article16. Gass JD. Retinal pigment epithelial rip during krypton red laser photocoagulation. Am J Ophthalmol. 1984; 98:700–6.17. Yeo JH, Marcus S, Murphy RP. Retinal pigment epithelial tears. Patterns and prognosis. Ophthalmology. 1988; 95:8–13.18. Decker WL, Sanborn GE, Ridley M. . Retinal pigment epithelial tears. Ophthalmology. 1983; 90:507–12.
Article19. Gass JD. Pathogenesis of tears of the retinal pigment epithelium. Br J Ophthalmol. 1984; 68:513–9.
Article20. Gass JD. Serous retinal pigment epithelial detachment with a notch. A sign of occult choroidal neovascularization. Retina. 1984; 4:205–20.21. Chang LK, Sarraf D. Tears of the retinal pigment epithelium: an old problem in a new era. Retina. 2007; 27:523–34.22. Gass JD. Idiopathic central serous chorioretinopathy. Stereoscopic atlas of macular diseases: diagnosis and treatment. St. Louis: Mosby;1997. p. 52–70.23. Schoeppner G, Chuang EL, Bird AC. The risk of fellow eye visual loss with unilateral retinal pigment epithelial tears. Am J Ophthalmol. 1989; 108:683–5.
Article24. Chuang EL, Bird AC. Bilaterality of tears of the retinal pigment epithelium. Br J Ophthalmol. 1988; 72:918–20.
Article25. Chan CK, Meyer CH, Gross JG. . Retinal pigment epithelial tears after intravitreal bevacizumab injection for neovascular age-related macular degeneration. Retina. 2007; 27:541–51.
Article26. Cunningham ET Jr, Feiner L, Chung C. . Incidence of retinal pigment epithelial tears after intravitreal ranibizumab injection for neovascular age-related macular degeneration. Ophthalmology. 2011; 118:2447–52.
Article27. Casswell AG, Kohen D, Bird AC. Retinal pigment epithelial detachments in the elderly: classification and outcome. Br J Ophthalmol. 1985; 69:397–403.
Article28. Pauleikhoff D, Löffert D, Spital G. . Pigment epithelial detachment in the elderly. Clinical differentiation, natural course and pathogenetic implications. Graefes Arch Clin Exp Ophthalmol. 2002; 240:533–8.29. McLaughlin S, Lockington D, Mansfield D. The importance of informed consent in patients with wet age-related macular degeneration considering intravitreal anti-vascular endothelial growth factor treatments. Scott Med J. 2012; 57:48–9.
Article30. Lesniak SP, Fine HF, Prenner JL, Roth DB. Long-term follow-up of spontaneous retinal pigment epithelium tears in age-related macular degeneration treated with anti-VEGF therapy. Eur J Ophthalmol. 2011; 21:73–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Observation of Retinal Pigment Epithelial Tear after Anti-VEGF Treatment for Age-Related Macular Degeneration
- Predictors of Retinal Pigment Epithelial Tears in Exudative Macular Degeneration with High Pigment Epithelial Detachment
- Anatomical Characteristics of End-stage Exudative Age-related Macular Degeneration Refractory to Intravitreal Anti-vascular Endothelial Growth Factor Injection
- Clinical Manifestation of Retinal Pigment Epithelial Tear after Treatment of Age-Related Macular Degeneration
- Culture of Bovine Retinal Pigment Epithelium: Topographical Differences of Morphology and Growth Rate in Vitro