J Korean Ophthalmol Soc.
2013 Aug;54(8):1293-1297.
Retinitis Pigmentosa Complicated by Vitreous Hemorrhage in a Young Patient: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea. parkjm@gnu.ac.kr
- 2Institute of Health Science, Gyeongsang National University, Jinju, Korea.
Abstract
- PURPOSE
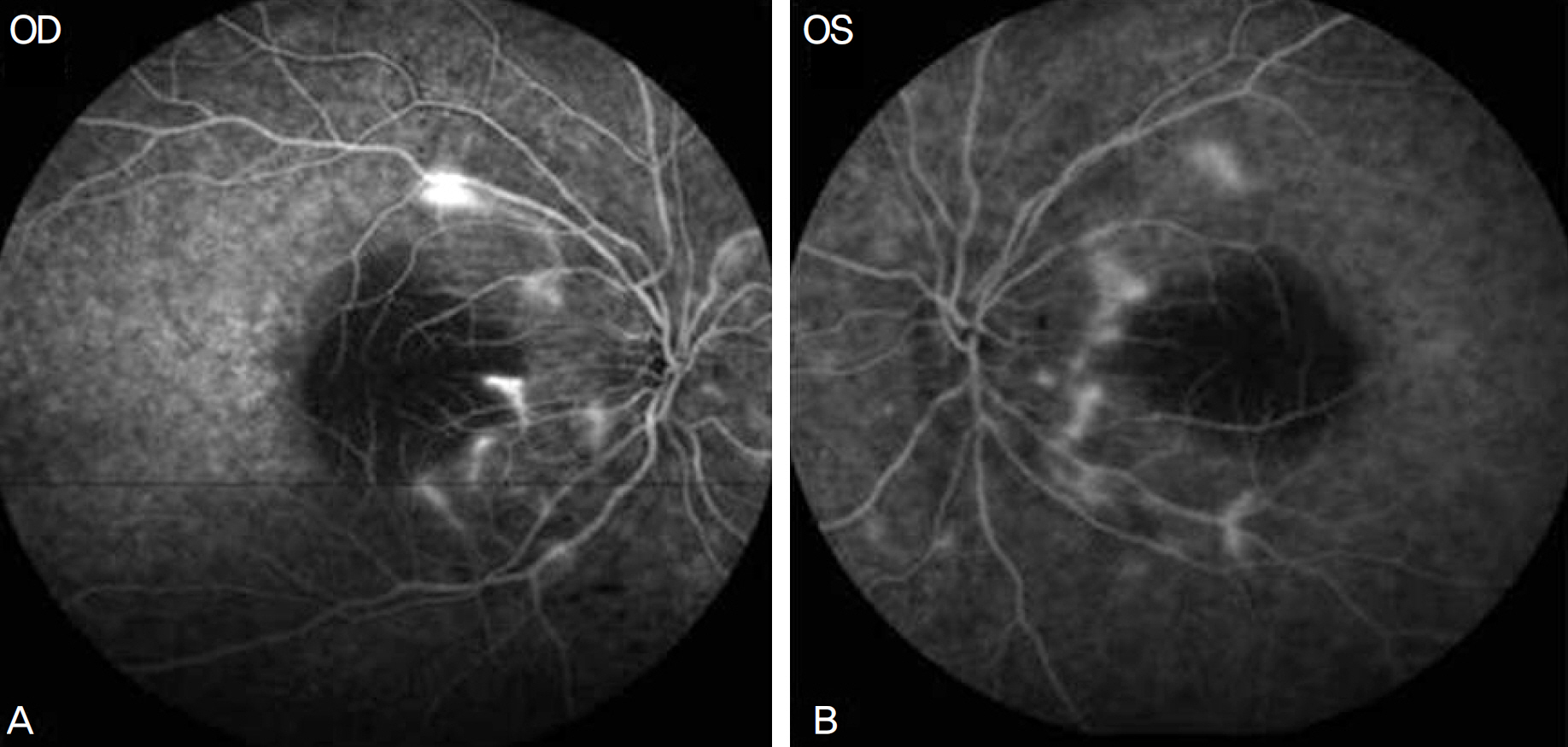
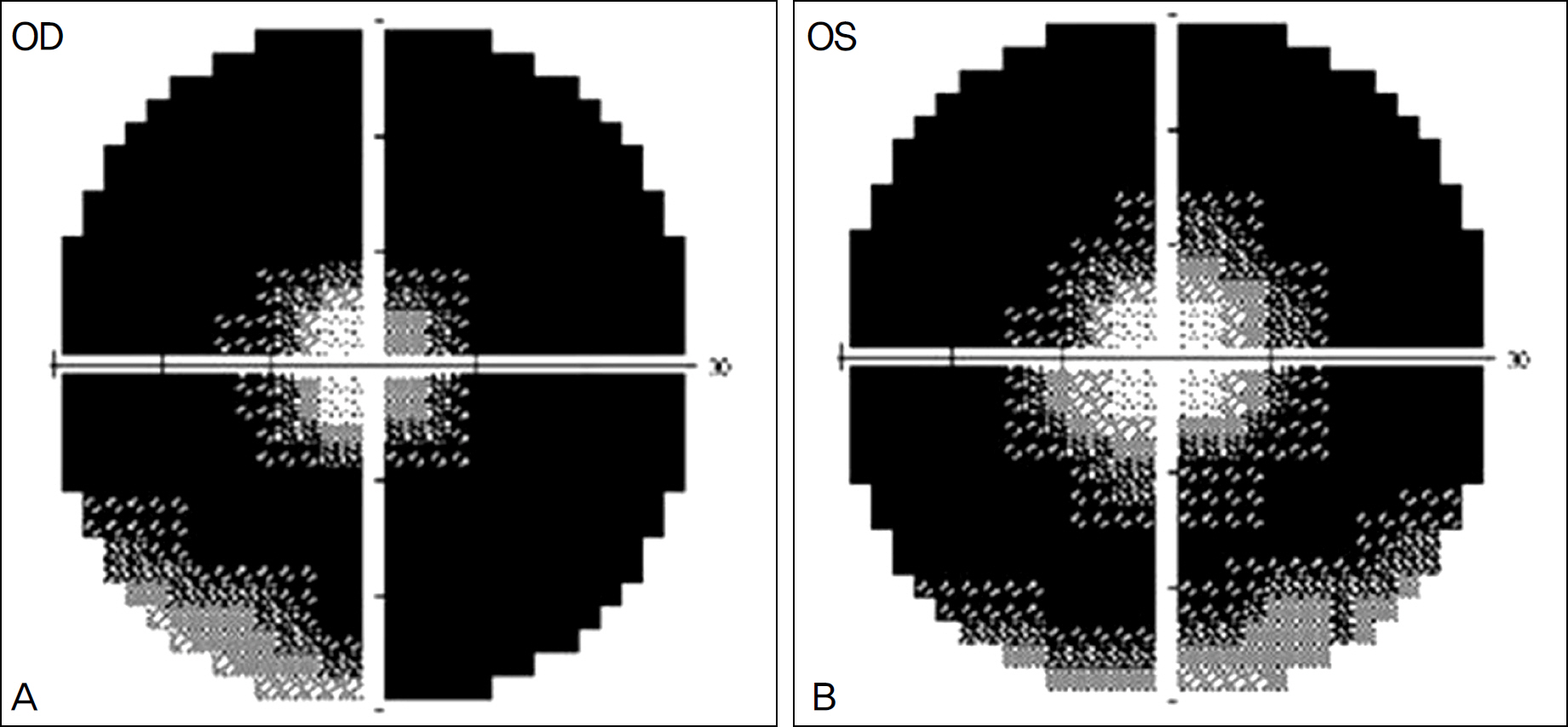
To report a case of a young male patient with retinitis pigmentosa (RP) accompanied by vitritis and neovascularization of the optic disk in both eyes who underwent unilateral vitrectomy for the treatment of vitreous hemorrhage in the right eye.
CASE SUMMARY
An 8-year-old boy visited our clinic with a complaint of night blindness. Both eyes showed inflammatory cells in the anterior vitreous and neovascularization of the optic disk confirmed by fluorescein angiography. Extensive vitreous hemorrhage developed in his right eye and he underwent unilateral vitrectomy. His final visual acuity was 0.6 in both eyes.
CONCLUSIONS
Vitreous hemorrhage may be related to chronic inflammation in the vitreous and is a very rare RP complication. Vitrectomy can be an effective treatment option for RP complicated by vitreous hemorrhage.
MeSH Terms
Figure
Reference
-
References
1. Wong P, Borst DE, Farber D. . Increased TRPM-2/clusterin mRNA levels during the time of retinal degeneration in mouse models of retinitis pigmentosa. Biochem Cell Biol. 1994; 72:(9-10). 439–46.
Article2. Cotran PR, Bruns GA, Berson EL, Dryja TP. Genetic analysis of patients with retinitis pigmentosa using a cloned cDNA probe for the human gamma subunit of cyclic GMP phosphodiesterase. Exp Eye Res. 1991; 53:557–64.
Article3. Uliss AE, Gregor ZJ, Bird AC. Retinitis pigmentosa and retinal neovascularization. Ophthalmology. 1986; 93:1599–603.
Article4. Newsome DA, Michels RG. Detection of lymphocytes in the vitre-ous gel of patients with retinitis pigmentosa. Am J Ophthalmol. 1988; 105:596–602.
Article5. Yoshida N, Ikeda Y, Notomi S. . Clinical evidence of sustained chronic inflammatory reaction in retinitis pigmentosa. Ophthalmology. 2013; 120:100–5.
Article6. Nao-i N, Fukiyama J, Sawada A. Retinitis pigmentosa with re-current vitreous hemorrhage. Acta Ophthalmol Scand. 1996; 74:509–12.
Article7. Bressler NM, Graqoudas ES. Neovascularization of the optic disk associated with atypical retinitis pigmentosa. Am J Ophthalmol. 1985; 100:431–3.
Article8. Henkind P. Ocular neovascularization. The Krill memorial lecture. Am J Ophthalmol. 1978; 85:287–301.
Article