J Korean Ophthalmol Soc.
2012 Jun;53(6):819-824.
Clinical Characteristics of Intermittent Exotropia Patients who Have Improved due to Corrected Refractive Errors
- Affiliations
-
- 1Department of Ophthalmology, Bundang CHA Medical Center, CHA University, Seongnam, Korea. eye@cha.ac.kr
Abstract
- PURPOSE
To evaluate clinical features of patients who have experienced decreased exodeviation after refractive error correction.
METHODS
Thirty-four patients who experienced decreased exodeviation after refractive error correction between 2003 and 2010 were evaluated. Visual acuity, refractive errors, reported age at onset, duration of wearing glasses, stereopsis, and function of fusion were evaluated.
RESULTS
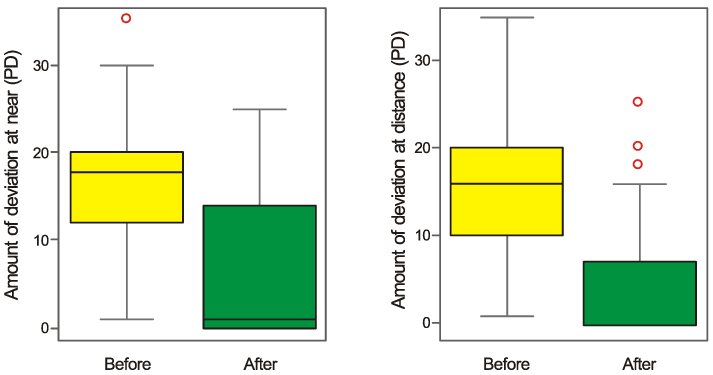
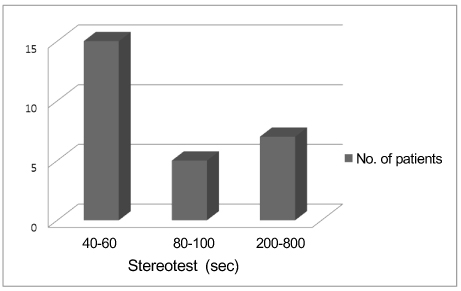
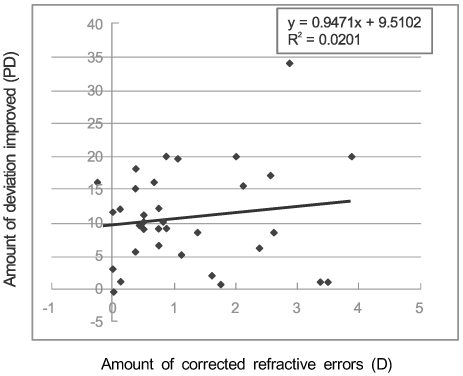
The present study included 34 patients with intermittent exotropia. Before correcting refractive errors, the mean visual acuity was 0.34 +/- 0.27 for the right eye and 0.37 +/- 0.27 for the left eye according to log MAR. After refractive error correction, mean visual acuity improved to 0.12 +/- 0.11 for the right eye and 0.11 +/- 0.11 for the left eye according to log MAR. Before correcting refractive errors, the amount of deviation was 18.1 +/- 7.4 PD at near and 13.5 +/- 8.4 PD at far. However, after correcting refractive errors, the amount of deviation decreased to 5.8 +/- 8.6 PD at near and 4.5 +/- 7.6 PD at far (p < 0.05).
CONCLUSIONS
The clinical characteristics of children who have decreased exodeviation after correcting refractive errors is shown by a greater amount of deviation at near than at distance and good fusional vergence and stereoacuity. Because correcting refractive errors by wearing appropriate glasses can decrease exodeviation, the authors of the present study recommend correcting refractive errors as the initial management for exotropia.
Keyword
MeSH Terms
Figure
Reference
-
1. Govindan M, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood exotropia: a population-based study. Ophthalmology. 2005. 112:104–108.2. Chia A, Roy L, Seenyen L. Comitant horizontal strabismus: an Asian perspective. Br J Ophthalmol. 2007. 91:1337–1340.3. Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. The development of myopia among children with intermittent exotropia. Am J Ophthalmol. 2010. 149:503–507.4. Kim MS, Koo BS. Preschool vision screening for 3 to 6-year old children in Korea. J Korean Ophthalmol Soc. 2003. 44:971–981.5. Gwiazda J, Marsh-Tootle WL, Hyman L, et al. Baseline refractive and ocular component measures of children enrolled in the correction of myopia evaluation trial(COMET). Invest Ophthalmol Vis Sci. 2002. 43:314–321.6. Ingram RM. Refraction as a basis for screening children for squint and amblyopia. Br J Ophthalmol. 1977. 61:8–15.7. Ingram RM, Gill LE, Lambert TW. Emmetropisation in normal and strabismic children and the associated changes of anisometropia. Strabismus. 2003. 11:71–84.8. Ip JM, Robaei D, Kifley A, et al. Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology. 2008. 115:678–685.9. Sohn HJ, Paik HJ. Clinical features of refractive accommodative esotropia according to the age of onset. J Korean Ophthalmol Soc. 2006. 47:941–946.10. Park KA, Kim SA, Oh SY. Effect of age wearing prescription glasses on changes of refractive error in accommodative esotropia. J Korean Ophthalmol Soc. 2009. 50:247–252.11. Rowe FJ, Noonan CP, Freeman G, DeBell J. Intervention for intermittent distance exotropia with overcorrecting minus lenses. Eye (Lond). 2009. 23:320–325.12. Jin HC, Park JH, Lee SY. Changes of deviation after the patch and +3.00 diopter spherical lens test in basic intermittent exotropia. J Korean Ophthalmol Soc. 2010. 51:1620–1624.13. Shim WS, Shim DM. A epidemiologic survey and clinical analysis of strabismus in children. J Korean Ophthalmol Soc. 1981. 22:847–854.14. Rah SH, Jun HS, Kim SH. An epidemiologic survey of strabismus among school - children in Korea. J Korean Ophthalmol Soc. 1997. 38:2195–2199.15. Hiles DA, Davies GT, Costenbader FD. Long-term observations on unoperated intermittent exotropia. Arch Ophthalmol. 1968. 80:436–442.16. Von Noorden GK, Campos EC. Binocular vision and ocular motility. Exodeviation. 2002. Vol. 1:6th ed. St. Louis: Mosby;chap. 17.17. Jung MS, Choi MY. The natural course in children with intermittent exotropia. J Korean Ophthalmol Soc. 2003. 44:1572–1577.18. Kim HY, Chang BL. Clinical evaluation of exotropia combined with amblyopia in children. J Korean Ophthalmol Soc. 1996. 37:662–668.19. Lee SH, Lew H, Yun YS. Spontaneous regression of exodeviation in intermittent exotropia. J Korean Ophthalmol Soc. 2006. 47:1306–1310.20. Caltrider N, Jampolsky A. Overcorrecting minus lens therapy for treatment of intermittent exotropia. Ophthalmology. 1983. 90:1160–1165.21. Kennedy JR. The correction of divergent with concave lenses. Am J Optom Arch Am Acad Optom. 1954. 31:605–614.22. The Korean Strabismus and Pediatric Ophthalmological Society. Current Concepts in Strabismus. 2004. 1st ed. Seoul: Naewae Haksool;58–67.23. Chung YR, Yang H, Lew HM, et al. The assessment of stereoacuity in patients with strabismus. J Korean Ophthalmol Soc. 2008. 49:1309–1316.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Surgical Outcomes in Patients with Small Refractive Error and Intermittent Exotropia
- Amblyopia and Sensory Fusional Anomaly in Intermittent Exotropia
- Refractive Errors and Strabismus in Down's Syndrome in Korea
- The Assessment of Stereoacuity in Patients with Strabismus
- Clinical Characteristics and Related Factors of Surgical Outcome in Patient who Underwent LR Recession After the age of 10 years