J Korean Ophthalmol Soc.
2011 Apr;52(4):385-391.
Clinical Correlation of Lacrimal Sac Pathologic Findings of Lacrimal Sac from Dacryocystorhinostomy
- Affiliations
-
- 1Department of Ophthalmology, Dong-A University College of Medicine, Busan, Korea. hbahn@dau.ac.kr
- 2Department of Pathology, Dong-A University College of Medicine, Busan, Korea.
Abstract
- PURPOSE
To determine the correlation of the clinical characteristics and histopathologic findings of lacrimal sac after external dacyrocystorhinostomy (DCR).
METHODS
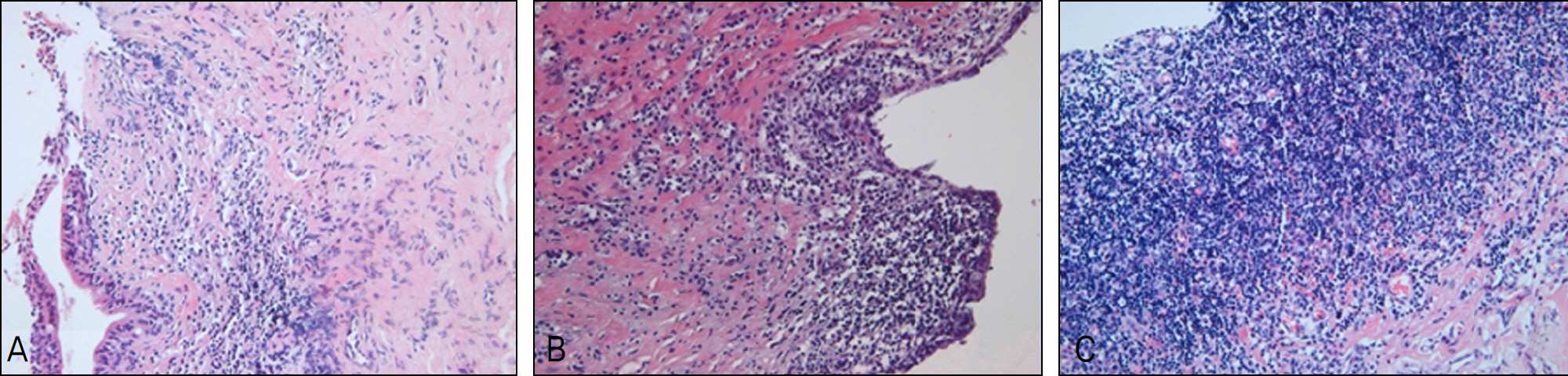
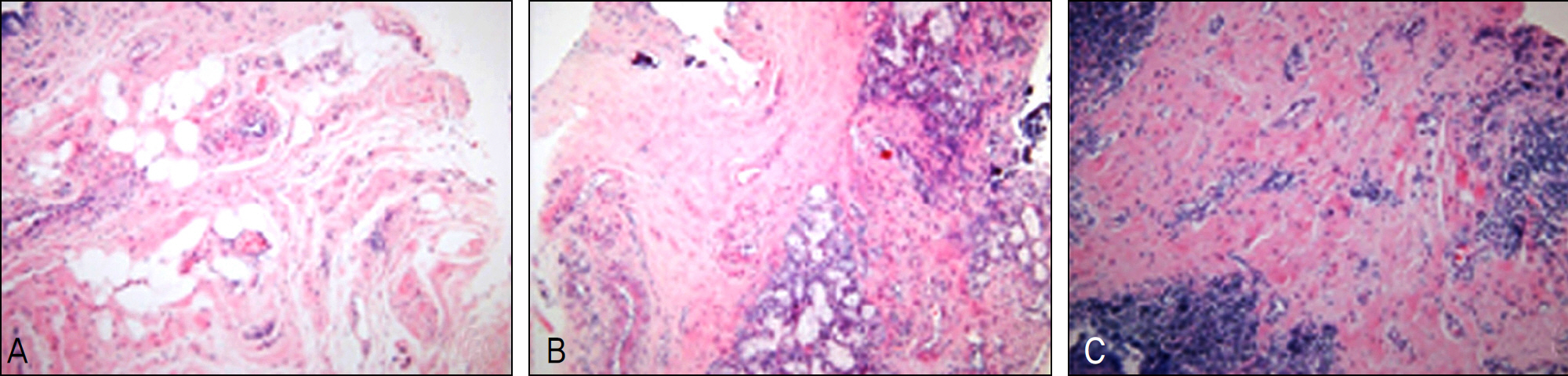
From March 2008 to June 2009, 49 lacrimal sac tissues of 47 patients were obtained after external DCR and divided according to fibrosis and inflammatory findings. The correlation of preoperative duration of symptoms with NLD obstruction, symptoms of recurrence and outcomes of the operation to the histopathologic findings were retrospectively evaluated.
RESULTS
The mean age of the patients was 58.83 +/- 11.49 years and the mean duration of preoperative symptoms was 65.2 +/- 69.05 months. Forty-three cases (88%) maintained good openings and 30 cases (61%) had no recurring symptoms over 6 months after the operation. Among the significant symptoms, severe subepithelial inflammations were observed more frequently at shorter duration. However, the fibrosis showed a positive relation with the preoperative duration of symptoms (Spearman correlation test, p<0.05). Most failures were found in the severe inflammation and fibrosis groups and were recovered with anti-inflammatory treatment.
CONCLUSIONS
Inflammation and fibrosis of the lacrimal sac could be an important prognostic and predictive factor of outcomes of DCR.
Figure
Reference
-
References
1. Sahlin S, Rose GE. Lacrimal drainage capacity and symptomatic improvement after dacryocystorhinostomy in adults presenting with patent lacrimal drainage systems. Orbit. 2001; 20:173–9.
Article2. Seider N, Kaplan N, Gilboa M, et al. Effect of timing of external dacryocystorhinostomy on surgical outcome. Ophthal Plast Reconstr Surg. 2007; 23:183–6.
Article3. McLachlan DL, Shannon GM, Flanagan JC. Results of dacryocystorhinostomy: analysis of the reoperations. Ophthalmic Surg. 1980; 11:427–30.4. Tarbet KJ, Custer PL. External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology. 1995; 102:1065–70.5. Lee HG, Lee YJ. Nasolacrimal ostium after external dacryocystorhinostomy. J Korean Ophthalmol Soc. 2006; 47:343–8.6. Picó G. A modified technique of external dacryocystorhinostomy. Am J Ophthalmol. 1971; 72:679–90.
Article7. Ha TS, Na KS, Chi NC. Effectiveness of washing nasolacrimal duct as an additional therapy after dacryocystorhinostomy. J Korean Ophthalmol Soc. 2000; 41:2308–12.8. Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986; 93:1055–63.9. Tucker N, Chow D, Stockl F, et al. Clinically suspected primary acquired nasolacrimal duct obstruction: clinicopathologic review of 150 patients. Ophthalmology. 1997; 104:1882–6.10. Mauriello JA Jr, Palydowycz S, DeLuca J. Clinicopathologic study of lacrimal sac and nasal mucosa in 44 patients with complete acquired nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 1992; 8:13–21.
Article11. Lee SH, Lew H, Sim JY. Pathologic features of lacrimal sac mucosa in primary acquired nasolacrimal duct obstruction patients. J Korean Ophthalmol Soc. 2004; 45:173–9.12. Hong JH, Chung WS. The surgical efficacy of external dacryocystorrhinostomy. J Korean Ophthalmol Soc. 2001; 42:547–52.13. Smith BC. Acquired lacrimal disorder. Nesi FA, Lisman RD, Levine MR, editors. Ophthalmic Plastic and Reconstructive Surgery. 2nd ed.St. Louise: Mosby;1998. p. 665–9.14. Heindl LM, Junemann A, Holbach LM. A clinicopathologic study of nasal mucosa in 350 patients with external dacryocystorhinostomy. Orbit. 2009; 28:7–11.
Article15. DeAngelis D, Hurwitz J, Oestreicher J, Howarth D. The pathogenesis and treatment of lacrimal obstruction: The value of lacrimal sac and bone analysis. Orbit. 2001; 20:163–72.
Article16. Ma YR, Jeong SK. The study of chronic dacryocystitis: identi-fication of pathogenic organism and histopathological findings. J Korean Ophthalmol Soc. 1999; 40:652–6.17. Kwak JJ, Lee DH, Lew HM. Endoscopic dacryocystorhinostomy with Mitomycin-C application. J Korean Ophthalmol Soc. 1998; 39:2211–7.18. Lee TS, Rhee KC. The effect of Mitomycin-C eyedrop on prevention of internal ostium obstruction after endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 1998; 39:1915–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Correlation between Organisms Cultured from the Lacrimal Sac and Lacrimal Punctum in Dacryocystitis
- The Study of Chronic Dacryocystitis: Identification of Pathogenic Organism and Histopathological Findings
- Primary Rhabdomyosarcoma of the Lacrimal Sac in a 68-year-old Woman
- Microorganisms in Conjunctival Sac, Lacrimal Sac and Nasal Cavity
- Pathologic Features of Lacrimal Sac Mucosa in Primary Acquired Nasolacrimal Duct Obstruction Patients