J Korean Ophthalmol Soc.
2010 Oct;51(10):1305-1311.
The Influence of Factors Before Wearing Reverse-Geometry Lens on Visual Acuity After Wearing Reverse-Geometry Lens
- Affiliations
-
- 1Department of Ophthalmology, Catholic Eye Clinic (Siji), Daegu, Korea. sh-kim15@hanmail.net
- 2Department of Ophthalmology, Catholic Eye Clinic (Seongseo), Daegu, Korea.
Abstract
- PURPOSE
To determine whether patient factors (pre-fitting patient's data) before reverse-geometry lens (RGL) use could be predicting factors for the increase in visual acuity after RGL use.
METHODS
The authors reviewed out patient records of 805 eyes of 423 patients wearing RGLs from March 2003 to May 2009. The relationship between patient factors on UVA before wearing a RGL examined at follow-ups and the IVA after wearing a RGL were analyzed.
RESULTS
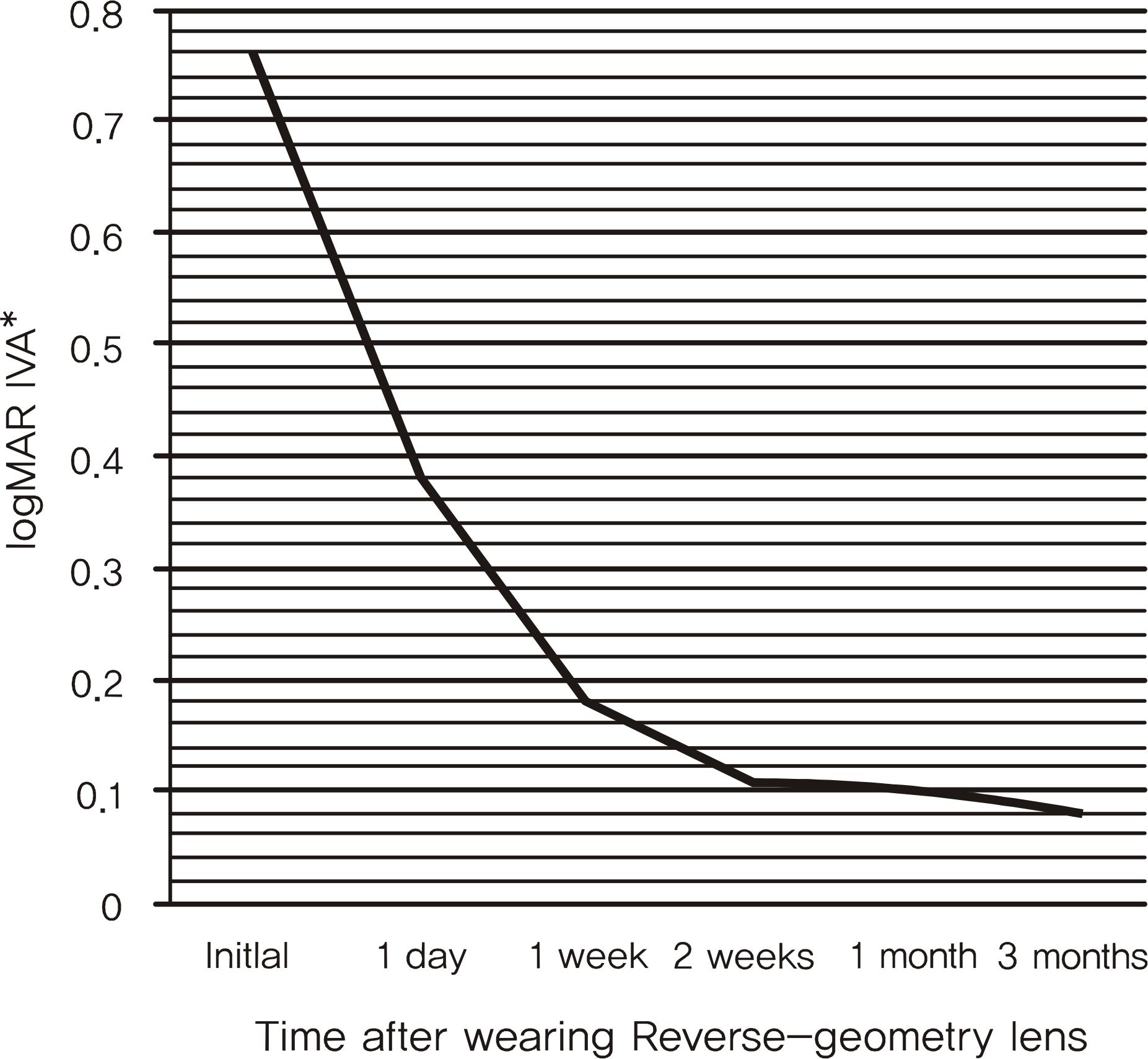
The spherical refractive errors and the cylindrical refractive errors showed statistically significant results (p < 0.05). The lower was the refractive error, the greater were the UVA and IVA results. Correlations existed between the corneal astigmatism and UVA or IVA at three months (p < 0.05). The lower was the corneal astigmatism, the greater were the UVA and IVA results. Correlations were observed between the initial visual acuity and IVA, although the initial visual acuity cannot be a predictor. The other factors evaluated did not show statistically significant results (p > 0.05).
CONCLUSIONS
The refractive error and the corneal astigmatism may be strong predictors of UVA and IVA after RGL use.
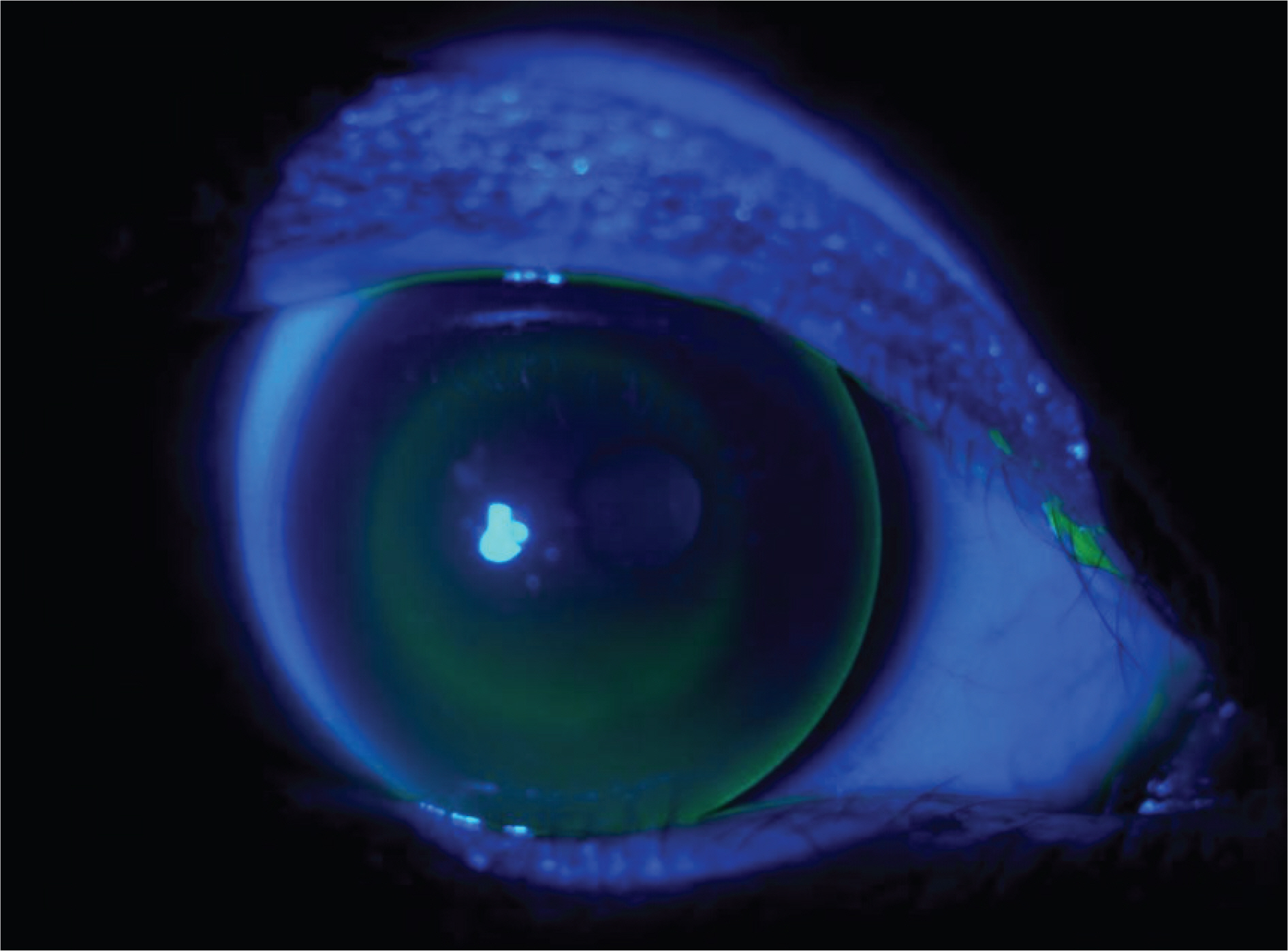
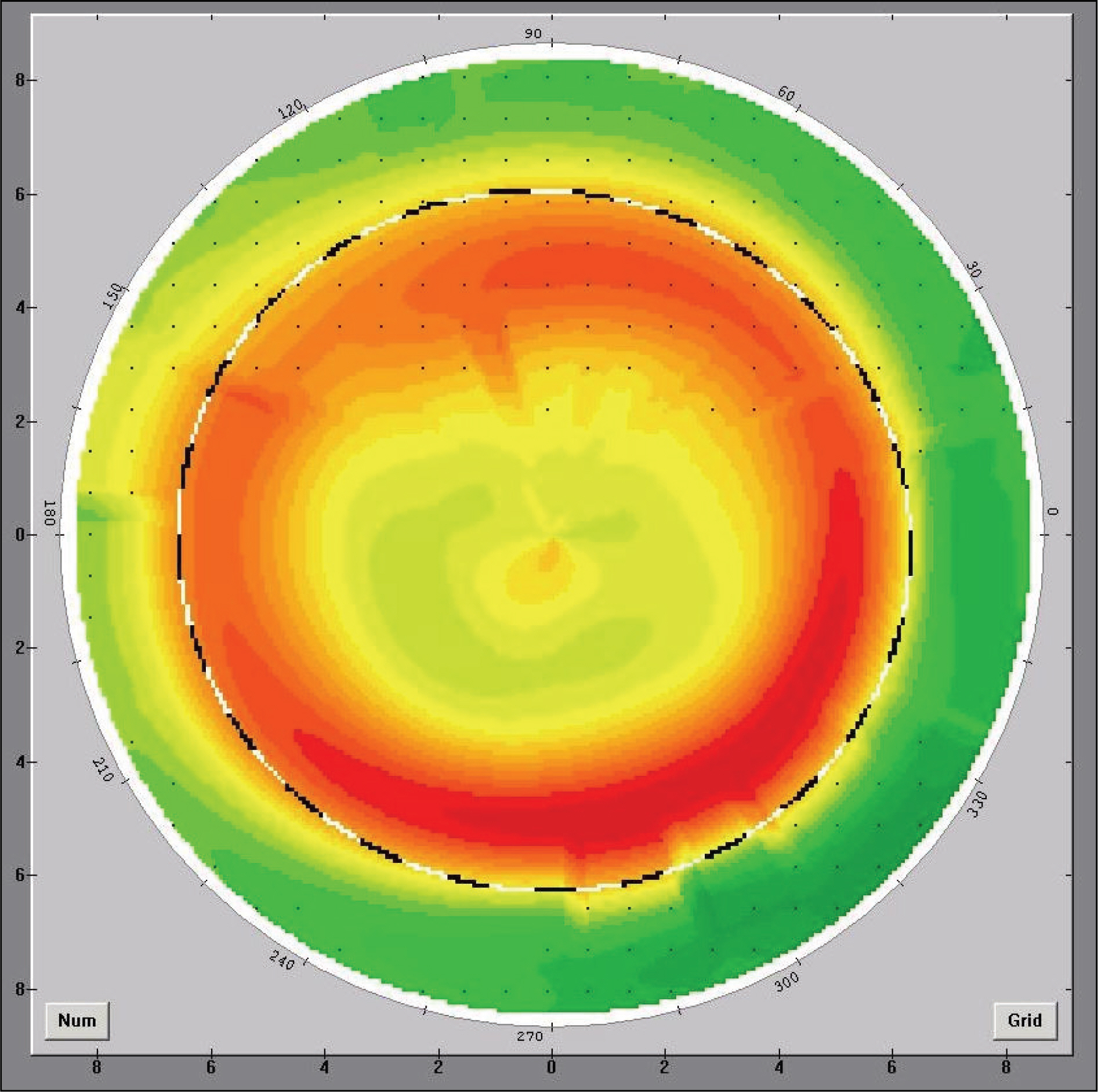
Figure
Reference
-
References
1. Carney LG. The basis for corneal shape change during contact lens wear. Am J Optom Physiol Opt. 1975; 52:445–54.
Article2. Dave T, Ruston D. Current trends in modern orthokeratology. Ophthalmic Physiol Opt. 1998; 18:224–33.
Article3. Brungardt TF. Orthokeratology: An Analysis. Int Contact Lens Clin. 1976; 3:56–8.4. Jessen G. Orthofocus techniques. Contacto. 1962; 6:200–4.5. Jeandervin M, Barr J. Comparison of repeat videokeratography: repeatability and accuracy. Optom Vis Sci. 1998; 75:663–9.
Article6. Szczotka LB, Aronsky M. Contact lenses after LASIK. J Am Optom Assoc. 1998; 69:775–84.7. Alio JL, Belda JI, Artola A, et al. Contact lens fitting to correct irregular astigmatism after corneal refractory surgery. J Cataract Refract Surg. 2002; 28:1750–7.8. Villa-Collar C, Gonzalez-Meijome JM, Gutierrez-Ortega R. Objective evaluation of the visual benefit in contact lens fitting after complicated LASIK. J Refract Surg. 2009; 25:591–8.
Article9. Martin R, Rodriguez G. Reverse geometry contact lens fitting after corneal refractive surgery. J Refract Surg. 2005; 21:753–6.
Article10. Liu J, Leach NE, Bergmanson JP. Reverse-geometry gas-permeable lens design for pellucid marginal degeneration. Eye Contact Lens. 2005; 31:127–9.
Article11. Wlodyga RJ, Bryla C. Corneal molding; the easy way. Contact Lens Spectrum. 1989; 4:14–6.12. Shin DB, Yang KM, Lee SB, et al. Effect of Reverse Geometry Lens on Correction of Moderate-degree Myopia and Cornea. J Korean Ophthalmol Soc. 2003; 44:1748–56.13. Chang JW, Choi TH, Lee HB. The Efficacy and Safety of Reverse Geometry Lenses. J Korean Ophthalmol Soc. 2004; 45:908–12.14. Carkeet NL, Mountford JA, Carney LG. Predicting success with orthokeratology lens wear: A retrospective analysis of ocular characteristics. Optom Vis Sci. 1995; 72:892–8.
Article15. Binder PS, May CH, Grant SC. An evaluation of orthokeratology. Ophthalmology. 1980; 87:729–44.
Article16. Kerns RL. Research in orthokeratology. Part I: Introduction and background. J Am Optom Assoc. 1976; 47:1047–51.17. Kerns RL. Research in orthokeratology. Part II: Experimental design, protocol and method. J Am Optom Assoc. 1976; 47:1275–85.18. Kerns RL. Research in orthokeratology. Part III: Results and observations. J Am Optom Assoc. 1976; 47:1505–15.19. Kerns RL. Research in orthokeratology. Part IV: Results and observations. J Am Optom Assoc. 1977; 48:227–38.20. Kerns RL. Research in orthokeratology. Part VI: Statistical and clinical analyses. J Am Optom Assoc. 1977; 48:1134–47.21. Kerns RL. Research in orthokeratology. Part VII: Examination of techniques, procedures and control. J Am Optom Assoc. 1977; 48:1541–53.22. Kerns RL. Research in orthokeratology. Part VIII: Results, conclusions and discussion of techniques. J Am Optom Assoc. 1978; 49:308–14.23. Jee DH, Hong ME, Kim MS. The efficacy and safety of Ortho-K LK(TM) lens. J Korean Ophthalmol Soc. 2003; 44:706–11.24. Wie HW, Lee DH, Kim JM. The efficacy and safety Dream LensTM in school children. J Korean Ophthalmol Soc. 2004; 45:913–9.25. Chang JW, Choi TH, Lee HB. The efficacy and safety of reverse geometry lenses. J Korean Ophthalmol Soc. 2004; 45:908–12.26. Mountford J. Retention and regression of orthokeratology with time. Int Contact Lens Clin. 1998; 25:59–64.
Article27. Soni PS, Horner DG. Orthokeratology. Bennett ES, Weissman BA, editors. Clinical contact lens practice. Philadelphia: JB Lippincott;1993. chap. 49.28. Soni PS, Nguyen TT, Bonanno JA. Overnight orthokeratology: visual and corneal changes. Eye Contact Lens. 2003; 29:137–45.29. Nichols JJ, Marsich MM, Nguyen M, et al. Overnight orthokeratology. Optom Vis Sci. 2000; 77:252–9.
Article30. Na JH, Choi JH, Yang JW, et al. The Relationship Between Asphericity and Visual Acuity After Wearing Reverse-Geometry Lens. J Korean Ophthalmol Soc. 2009; 50:670–6.
Article31. Mountford J. An Analysis of the changes in corneal shape and refractive error induced by accelerated orthokeratology. Int Contact Lens Clin. 1997; 24:128–44.
Article32. Joe JJ, Marsden HJ, Edrington TB. The relationships between corneal eccentricity and improvement in visual acuity with orthokeratology. J Am Optom Assoc. 1996; 67:87–97.33. Jayakumar J, Swarbrick HA. The effect of age on short-term orthokeratology. Optom Vis Sci. 2005; 82:505–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship Between Asphericity and Visual Acuity After Wearing Reverse-Geometry Lens
- An Analysis of Correlation with Visual Acuity, Refractive Error and Corneal Astigmatism after Wearing of Reverse Geometry Lenses
- Major Complications of Overnight Orthokeratology Lens for Myopic Correction
- The Efficacy and Safety of Reverse Geometry Lenses
- The Effect of RGP Lens and Reverse Geometry Lens on Apoptosis in Rabbit Cornea