J Korean Ophthalmol Soc.
2009 May;50(5):670-676. 10.3341/jkos.2009.50.5.670.
The Relationship Between Asphericity and Visual Acuity After Wearing Reverse-Geometry Lens
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, College of Medicine, The Catholic University of Korea, Seoul, Korea. cassiopeia@catholic.ac.kr
- KMID: 2212296
- DOI: http://doi.org/10.3341/jkos.2009.50.5.670
Abstract
-
PURPOSE:To report the change of corneal asphericity and the relationship between asphericity and visual acuity after wearing the reverse-geometry lens.
METHODS
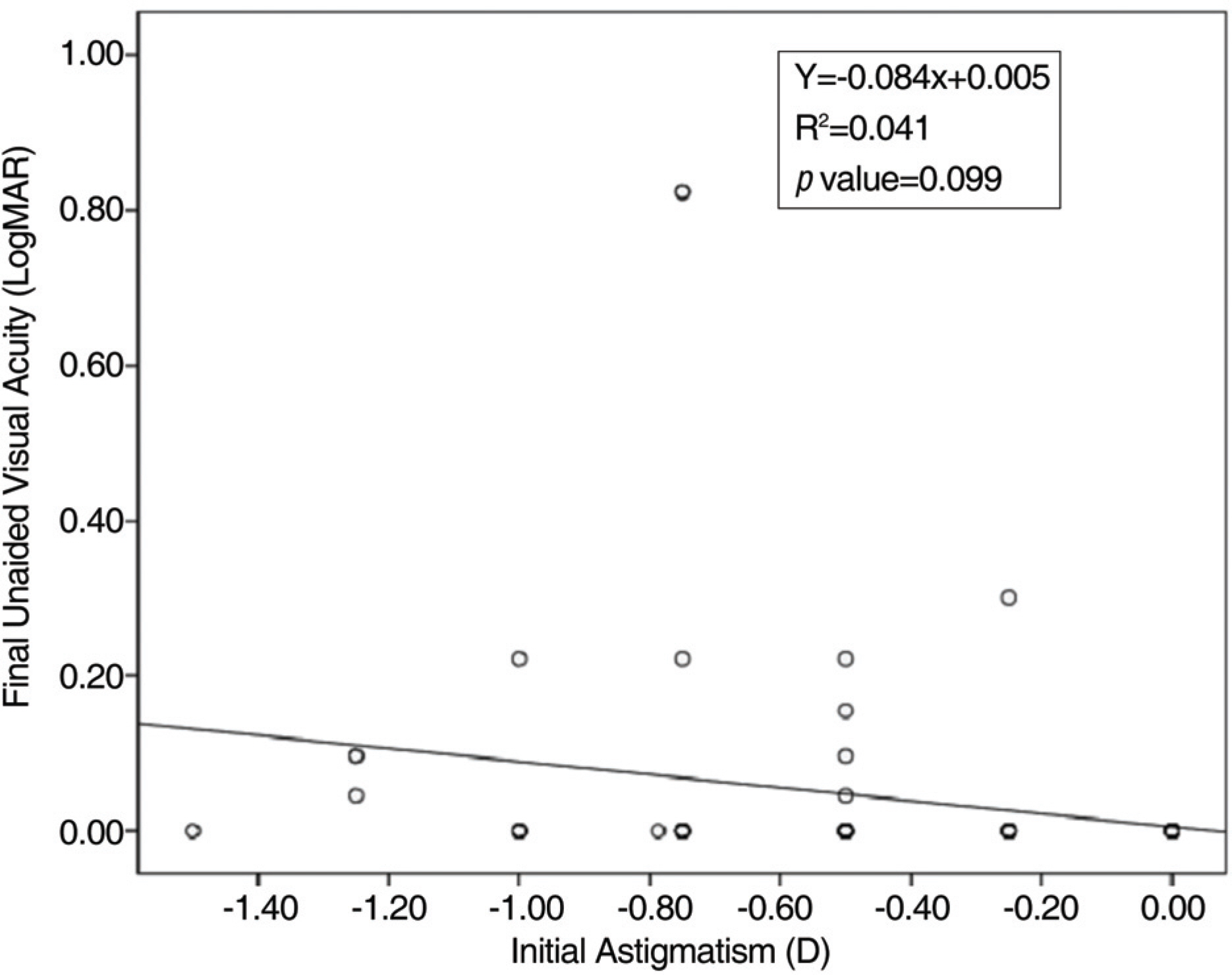
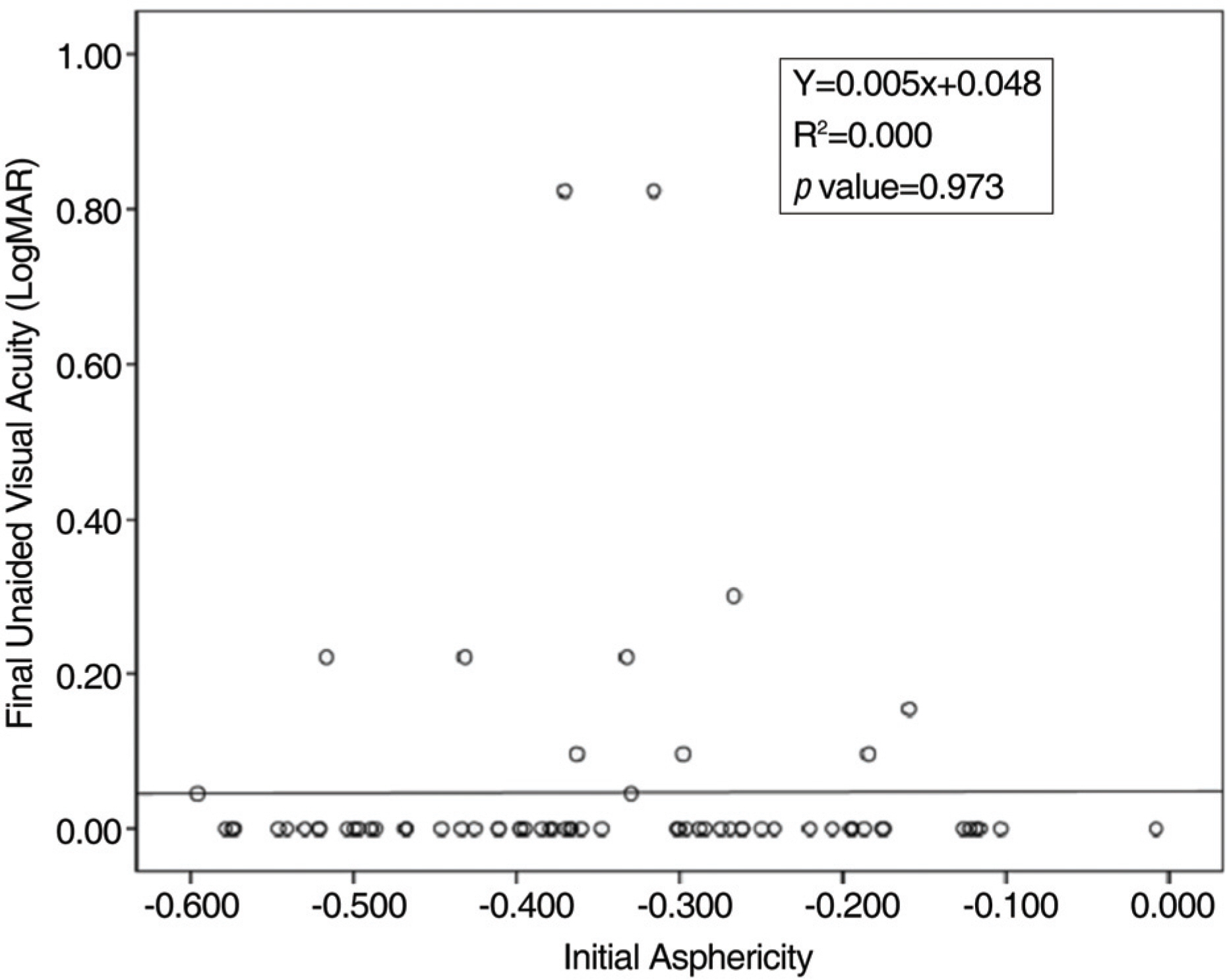
The authors reviewed out-patient records of 37 consecutive patients wearing reverse-geometry lenses. The patients were followed up from July 2004 to December 2007. The unaided visual acuity (VA), spherical equivalent (SE) and asphericity before and after wearing the lens were compared. The relationship of SE and final VA, initial astigmatism and final VA, and asphericity and final VA was also analyzed. In addition, the relationship between the increment of VA and asphericity was determined.
RESULTS
VA and SE improved and the asphericity decreased after wearing the lens (p<0.05). There was high correlation between the spherical equivalent and final visual acuity (p<0.001), and no correlation between asphericity and final visual acuity (p=0.358) was observed. However, the lower the initial asphericity, the greater the increment of visual acuity observed (p=0.048).
CONCLUSIONS
Initial corneal asphericity can be a predictor of increment of VA after wearing reverse-geometry lenses.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Influence of Factors Before Wearing Reverse-Geometry Lens on Visual Acuity After Wearing Reverse-Geometry Lens
Sung Hoon Kim, Jung Hoon Lee, Chun Sik Kim
J Korean Ophthalmol Soc. 2010;51(10):1305-1311. doi: 10.3341/jkos.2010.51.10.1305.
Reference
-
References
1. Brungardt TF. Orthokeratology: An Analysis. Int Contact Lens Clin. 1976; 3:56–8.2. Joe JJ, Marsden HJ, Edrington TB. The relationships between corneal eccentricity and improvement in visual acuity with orthokeratology. J Am Optom Assoc. 1996; 67:87–97.3. Choi JH, Ryu JW, Lee YC, Kim HS. An Analysis of Correlation with Visual Acuity, Refractive Error and Corneal Astigmatism after Wearing of Reverse Geometry Lenses. J Korean Ophthalmol Soc. 2006; 47:1266–73.4. Cheung SW, Cho P. Subjective and Objective assessments of the effect of orthokeratology. Curr Eye Res. 2004; 28:127–7.5. Nichols JJ, Marsich MM, Nguyen M, et al. Overnight orthokeratology. Optom Vis Sci. 2000; 77:252–9.
Article6. Liou HL, Brennan NA. Anatomically accurate, finite model eye for optical modeling. J Opt Soc Am A. 1997; 14:1684–95.
Article7. Kiely PM, Smith G, Carney LG. Meridional variations of corneal shape. Am J Optom Physiol Opt. 1984; 61:619–26.
Article8. Davis WR, Raasch TW, Mitchell GL, et al. Corneal Asphericity and Apical Curvature in Children: A Cross-sectional and Longitudinal evaluation. Invest Ophthalmol Vis Sci. 2005; 46:1899–906.
Article9. Horner DG, Soni PS, Vyas N, Himebaugh NL. Longitudinal Changes in Corneal Asphericity in Myopia. Optom Vis Sci. 2000; 77:198–203.
Article10. Lee HJ, Won CH, Song YY, Mah KC. Correlations between Refractive Error and Corneal Shape. Korean Journal of Vision Science. 2002; 4:11–8.11. Shin DB, Yang KM, Lee SB, et al. Effect of Reverse Geometry Lens on Correction of Moderate-degree Myopia and Cornea. J Korean Ophthalmol Soc. 2003; 44:1748–56.12. Chang JW, Choi TH, Lee HB. The Efficacy and Safety of Reverse Geometry Lenses. J Korean Ophthalmol Soc. 2004; 45:908–12.13. Carkeet NL, Mountford JA, Carney LG. Predicting success with orthokeratology lens wear: a retrospective analysis of ocular characteristics. Optom Vis Sci. 1995; 72:892–8.
Article14. Polse KA, Brand RJ, Schwalbe JS, et al. The Berkalay orthokeratology study. Part II: Efficacy and duration. Am J Optom Physiol Opt. 1983; 60:187–98.15. Mountford JA. Analysis of the changes in corneal shape and refractive error inducedby accelerated orthokeratoìogy. ICLC. 1997; 24:128–44.16. Careek A, Luo HD, Tong L, et al. Refractive error and monochromatic aberrations in Singaporean children. Vision Res. 2002; 42:1809–24.17. Jayakumar J, Swarbrick HA. The effect of age on short-term orthokeratology. Optom Vis Sci. 2005; 82:505–11.
Article18. Jee DH, Hong ME, Kim MS. The efficacy and safety of Ortho-K LKTM lens. J Korean Ophthalmol Soc. 2003; 44:706–11.19. Schein OD, Glynn RJ, Poggio EC, Sedden JM. The relative risk of ulcerative keratitis among users of daily-wear and extended-wear contact lenses. N Engl J Med. 1989; 321:779–83.20. Kang SY, Kim BK, Byun YJ. Sustainability of orthokeratology as demonstrated by corneal topography. Korean J Ophthalmol. 2007; 21:74–8.
Article21. Yun YM, Kim MK, Lee JL. Change of corneal parameters after removing reverse geometry lens in moderate degree myopia. J Korean Ophthalmol Soc. 2005; 46:1478–85.22. Swarbrick HA, Wong G, O'Leary DJ. Corneal response to orthokeratology. Optom Vis Sci. 1998; 75:791–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of Factors Before Wearing Reverse-Geometry Lens on Visual Acuity After Wearing Reverse-Geometry Lens
- An Analysis of Correlation with Visual Acuity, Refractive Error and Corneal Astigmatism after Wearing of Reverse Geometry Lenses
- The Efficacy and Safety of Reverse Geometry Lenses
- Clinical Observations on Hyper II(R) Soft Contact Lens
- Major Complications of Overnight Orthokeratology Lens for Myopic Correction