J Korean Orthop Assoc.
2010 Aug;45(4):301-306.
Body Mass Index in Patients with Early Posterior Tibial Tendon Dysfunction in Korea
- Affiliations
-
- 1Department of Orthopedic Surgery, Haeundae Paik Hospital, Inje University School of Medicine, Busan, Korea.
- 2Department of Orthopedic Surgery, Ilsan Paik Hospital, College of Medicine, Inje University, Koyang, Korea. sjs0506@paik.ac.kr
Abstract
- PURPOSE
Posterior tibial tendon dysfunction (PTTD) is known as the most common cause of adult acquired flatfoot syndrome and is common in middle-aged obese women. The purpose of this study was to describe the relationship between BMI (body mass index) and early stage PTTD in Korea. MATERIALS AND
METHODS
Between May 2005 and June 2006 we evaluated 42 patients (58 feet) who were diagnosed and treated for early stage PTTD. We analyzed demographic data such as sex, age, BMI, physical findings, radiologic findings and clinical results.
RESULTS
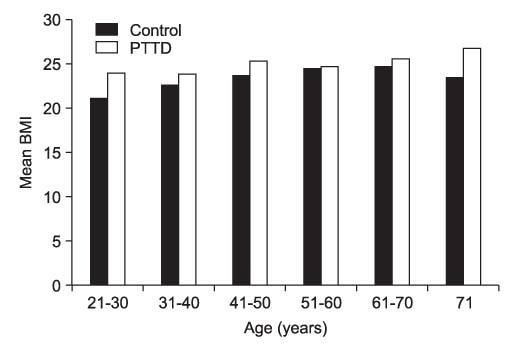
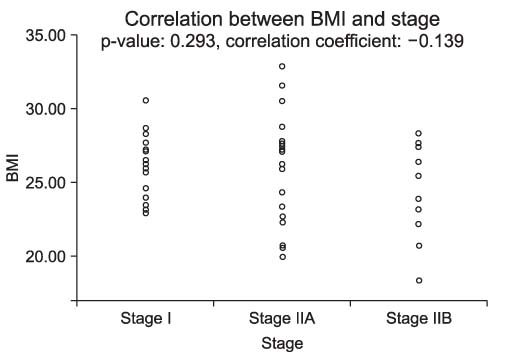
All 42 patients were women; their mean age was 52.6 years. Of the 42, 77% were middle aged (40-69). Increased BMI was detected in 75% of the 42 patients. There was no statistical significance in age-matched comparisons of BMI in Korea (p>0.05), or in the correlation between BMI and progression (p=0.293). Non-obese patients had superior clinical results (p=0.017).
CONCLUSION
Overweight and obesity are commonly seen in patients with early stage PTTD in Korea but there do not appear to be any significant correlation between obesity and early stage PTTD and also no significant correlation between obesity and progression to later stages.
MeSH Terms
Figure
Reference
-
1. Blake RL, Anderson K, Ferguson H. Posterior tibial tendinitis. A literature review with case reports. J Am Podiatr Med Assoc. 1994. 84:141–149.
Article2. Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res. 1989. 239:196–206.
Article3. Pinney SJ, Lin SS. Current concept review: acquired adult flatfoot deformity. Foot Ankle Int. 2006. 27:66–75.
Article4. Pomeroy GC, Pike RH, Beals TC, Manoli A 2nd. Acquired flatfoot in adults due to dysfunction of the posterior tibial tendon. J Bone Joint Surg Am. 1999. 81:1173–1182.
Article5. Trnka HJ. Dysfunction of the tendon of tibialis posterior. J Bone Joint Surg Br. 2004. 86:939–946.
Article6. Holmes GB Jr, Mann RA. Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle. 1992. 13:70–79.
Article7. Saltzman CL, el-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995. 16:572–576.
Article8. Alvares RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006. 27:2–8.9. Jeong TH, Oh JK, Lee HJ, Yang YJ, Nha KW, Suh JS. The effect of the combined stretching and strengthening exercise on the clinical symptoms in posterior tibial tendon dysfunction patient. J Korean Foot Ankle Soc. 2008. 12:47–54.10. Marcus RE, Pfister ME. The enigmatic diagnosis of posterior tibialis tendon rupture. Iowa Orthop J. 1993. 13:171–177.11. Frey C, Shereff M, Greenidge N. Vascularity of the posterior tibial tendon. J Bone Joint Surg Am. 1990. 72:884–888.
Article12. Fujii T, Uchuyama E, Kitaoka HB, Luo ZP, Zhao KD, An KN. The influence of flatfoot deformity on the gliding resistance of tendons about the ankle. Foot Ankle Int. 2009. 30:1107–1110.
Article13. Myerson M, Solomon G, Shereff M. Posterior tibial tendon dysfunction: its association with seronegative inflammatory disease. Foot Ankle. 1989. 9:219–225.
Article14. Deland JT. The adult acquired flatfoot and spring ligament complex. Pathology and implications for treatment. Foot Ankle Clin. 2001. 6:129–135.
Article15. Deland JT, de Asla RJ, Sung IH, Ernberg LA, Potter HG. Posterior tibial tendon insufficiency: which ligaments are involved? Foot Ankle Int. 2005. 26:427–435.
Article16. Greisberg J, Hansen ST Jr, Sangeorzan B. Deformity and degeneration in the hindfoot and midfoot joints of the adult acquired flatfoot. Foot Ankle Int. 2003. 24:530–534.
Article17. Friedman MA, Draganich LF, Toolan B, Brage ME. The effects of adult acquired flatfoot deformity on tibiotalar joint contact characteristics. Foot Ankle Int. 2001. 22:241–246.
Article18. Moon DH, Park HK, Choi ES, Kim DG, Kim MJ. Posterior tibialis tendon dysfunction: preliminary report. J Korean Orthop Assoc. 2008. 43:799–807.
Article19. Lin JL, Balbas J, Richardson EG. Results of non-surgical treatment of stage II posterior tibial tendon dysfunction: a 7- to 10-year followup. Foot Ankle Int. 2008. 29:781–786.
Article20. Kulig K, Lederhaus ES, Reischl S, Arya S, Bashford G. Effect of eccentric exercise program for early tibialis posterior tendinopathy. Foot Ankle Int. 2009. 30:877–885.
Article21. Niki H, Ching RP, Kiser P, Sangeorzan BJ. The effect of posterior tibial tendon dysfunction on hindfoot kinematics. Foot Ankle Int. 2001. 22:292–300.
Article22. Yeap JS, Singh D, Birch R. Tibialis posterior tendon dysfunction: a primary or secondary problem? Foot Ankle Int. 2001. 22:51–55.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acquired Adult Flatfoot: Pathophysiology, Diagnosis, and Nonoperative Treatment
- A Clinical Analysis on Split Posterior Tibial Tendon Transfers for Spastic Equinovarus Deformity in Cerebral Palsy
- Acquired Flat Foot due to Rupture of Posterior Tibial Tendon: Two case reports
- Diagnosis of Flatfoot Deformity
- Treatment of Flatfoot Deformity