J Korean Rheum Assoc.
2010 Sep;17(3):326-330.
A Case of Recurrent Bowel Perforation in a Patient with Churg-Strauss Syndrome
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Wonkwang University, Iksan, Korea. ckhlms@hanmail.net
- 2Department of Plastic Surgery, College of Medicine, Wonkwang University, Iksan, Korea.
- 3Department of Neurosurgery, College of Medicine, Wonkwang University, Iksan, Korea.
- 4Department of Emergency Medicine, Wonkwang University Sanbon Hospital, Gunpo, Korea.
Abstract
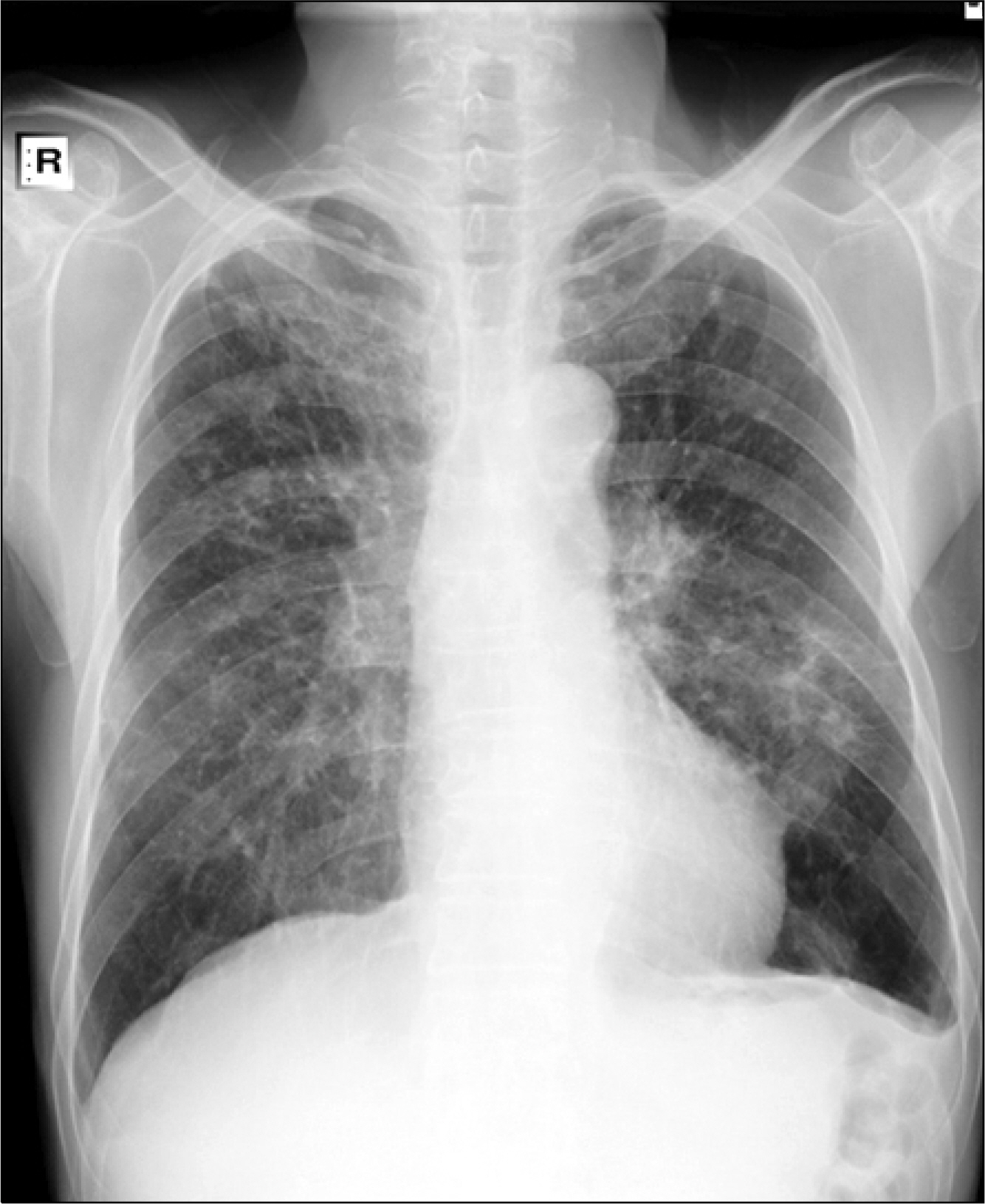
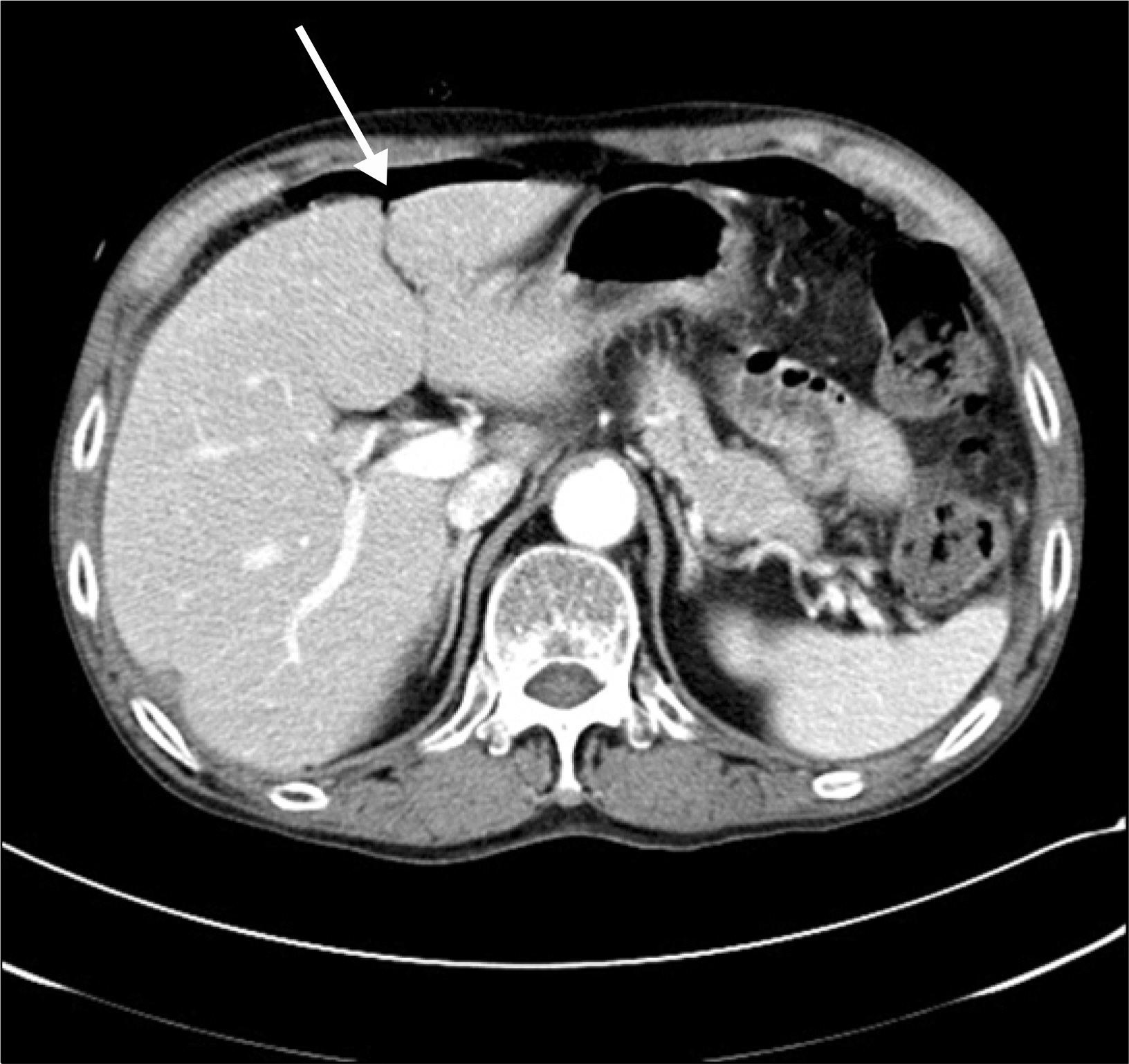
- Churg-Strauss syndrome is a rare systemic disorder characterized by asthma, eosionphilia and necrotizing vasculitis affecting small-to-medium-sized vessels. Although it is frequently associated with gastrointestinal mucosal lesions, recurrent bowel perforation is rare and potentially life threatening. We report a case of a 66-year-old man with Churg-Strauss syndrome, who presented with recurrent small bowel perforation. He was admitted with abdominal pain developed previous night, who had a previous small bowel perforation history treated with laparoscopic closure 5 months ago. Laboratory data showed remarkable eosinophilia. Physical examination indicated positive signs of peritoneal irritation in the entire abdomen, and abdominal computed tomography scanning showed edematous small bowel with intra-abdominal free air, suggesting intestinal perforation. He underwent laparoscopic small bowel closure and was treated with steroid.
MeSH Terms
Figure
Reference
-
1). Churg J., Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol. 1951. 27:277–301.2). Chumbley LC., Harrison EG Jr., DeRemee RA. Allergic granulomatosis and angiitis (Churg-strauss syndrome). Report and analysis of 30 cases. Mayo Clin Proc. 1977. 52:477–84.3). Guillevin L., Lhote F., Gayraud M., Cohen P., Jarrousse B., Lortholary O, et al. Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome. A prospective study in 342 patients. Medicine (Baltimore). 1996. 75:17–28.
Article4). Harper L., Savage CO. Pathogenesis of ANCA-associated systemic vasculitis. J Pathol. 2000. 190:349–59.
Article5). Vaglio A., Martorana D., Maggiore U., Grasselli C., Zanetti A., Pesci A, et al. HLA-DRB4 as a genetic risk factor for Churg-Strauss syndrome. Arthritis Rheum. 2007. 56:3159–66.
Article6). Sinico RA., Di Toma L., Maggiore U., Bottero P., Radice A., Tosoni C, et al. Prevalence and clinical significance of antineutrophil cytoplasmic antibodies in Churg-Strauss syndrome. Arthritis Rheum. 2005. 52:2926–35.
Article7). Lanham JG., Elkon KB., Pusey CD., Hughes GR. Systemic vasculitis with asthma and eosinophilia: a clinical approach to the Churg-Strauss syndrome. Medicine (Baltimore). 1984. 63:65–81.8). Sharma MC., Safaya R., Sidhu BS. Perforation of small intestine caused by Churg-Strauss syndrome. J Clin Gastroenterol. 1996. 23:232–5.
Article9). Murakami S., Misumi M., Sakata H., Hirayama R., Kubojima Y., Nomura K, et al. Churg-Strauss syndrome manifesting as perforation of the small intestine: report of a case. Surg Today. 2004. 34:788–92.
Article10). Park JH., Jung YS., Kim YK., Lee YM., Hwang JH., Kim KU, et al. A case of Churg-Strauss syndrome with Interstinal Perforation. Tuberc Respir Dis. 2009. 66:374–9.
Article11). Sinico RA., Bottero P. Churg-Strauss angiitis. Best Pract Res Clin Rheumatol. 2009. 23:355–66.
Article12). Nakamura Y., Sakurai Y., Matsubara T., Nagai T., Fukaya S., Imazu H, et al. Multiple perforated ulcers of the small intestine associated with allergic granulomatous angiitis: report of a case. Surg Today. 2002. 32:541–6.
Article13). Cottin V., Cordier JF. Churg-Strauss syndrome. Allergy. 1999. 54:535–51.
Article14). Taniguchi M., Tsurikisawa N., Higashi N., Saito H., Mita H., Mori A, et al. Treatment for Churg-Strauss syndrome: induction of remission and efficacy of intravenous immunoglobulin therapy. Allergol Int. 2007. 56:97–103.
Article15). Gayraud M., Guillevin L., le Toumelin P., Cohen P., Lhote F., Casassus P, et al. Long-term followup of polyarteritis nodosa, microscopic polyangiitis, and Churg-Strauss syndrome: analysis of four prospective trials including 278 patients. Arthritis Rheum. 2001. 44:666–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Chrug-Strauss Syndrome Complicated with Intestinal Perforation
- A Case of Churg-Strauss Syndrome Associated with Small Bowel Perforationfollowing High Dose Systemic Steroid Intravenous Injection
- A case of Churg-Strauss syndrome that underwent endoscopic sinus surgery under total intravenous anesthesia: A case report
- A Case of Churg-Strauss Syndrome with Endomyocardial Fibrosis
- A case of intestinal perforation in Churg-Strauss syndrome patient