J Korean Assoc Oral Maxillofac Surg.
2013 Oct;39(5):246-250.
Importance of immediate surgical intervention and antifungal treatment for rhinocerebral mucormycosis: a case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Yonsei University, Seoul, Korea. omsnam@yuhs.ac
Abstract
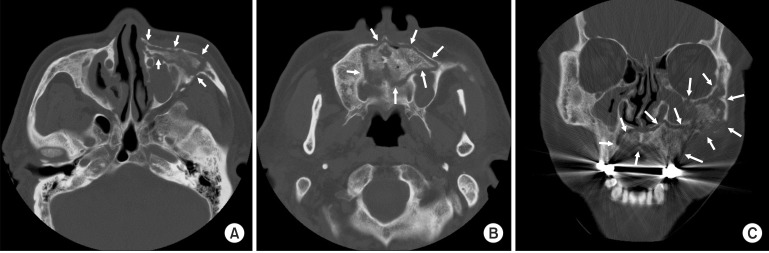
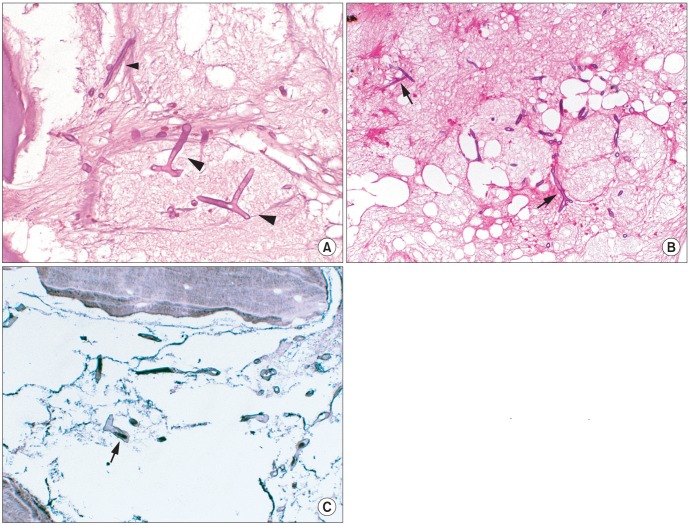
- Rhinocerebral mucormycosis (RCM) is an opportunistic, potentially life-threatening fungal disease. This infective disease invades not only the facial sinuses, but also the maxilla, zygoma, and rhino-cerebral structures with a massive destruction of the facial skeletons and soft tissue. This disease progresses within various underlying diseases, such as diabetes mellitus, hematologic malignancy, renal failure, and systemic immunodepression. The relationship between mucormycosis and these underlying conditions have been discussed extensively in the literature. The authors studied 6 cases of RCM diagnosed by a tissue biopsy and treated at the department of oral and maxillofacial surgery, from 1997 to 2012. Patients were treated with several kinds of surgical interventions and antifungal agents, and their clinical & radiological signs, underlying conditions, surgical methods, and outcomes were analyzed.
Keyword
MeSH Terms
Figure
Reference
-
1. Abu El-Naaj I, Leiser Y, Wolff A, Peled M. The surgical management of rhinocerebral mucormycosis. J Craniomaxillofac Surg. 2013; 41:291–295. PMID: 23058177.
Article2. Mantadakis E, Samonis G. Clinical presentation of zygomycosis. Clin Microbiol Infect. 2009; 15(Suppl 5):15–20. PMID: 19754751.
Article3. Dhiwakar M, Thakar A, Bahadur S. Improving outcomes in rhinocerebral mucormycosis--early diagnostic pointers and prognostic factors. J Laryngol Otol. 2003; 117:861–865. PMID: 14670145.4. Bitar D, Van Cauteren D, Lanternier F, Dannaoui E, Che D, Dromer F, et al. Increasing incidence of zygomycosis (mucormycosis), France, 1997-2006. Emerg Infect Dis. 2009; 15:1395–1401. PMID: 19788806.
Article5. Rammaert B, Lanternier F, Poirée S, Kania R, Lortholary O. Diabetes and mucormycosis: a complex interplay. Diabetes Metab. 2012; 38:193–204. PMID: 22386924.
Article6. Chinn RY, Diamond RD. Generation of chemotactic factors by Rhizopus oryzae in the presence and absence of serum: relationship to hyphal damage mediated by human neutrophils and effects of hyperglycemia and ketoacidosis. Infect Immun. 1982; 38:1123–1129. PMID: 6818145.
Article7. Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005; 41:634–653. PMID: 16080086.
Article8. Chakrabarti A, Das A, Mandal J, Shivaprakash MR, George VK, Tarai B, et al. The rising trend of invasive zygomycosis in patients with uncontrolled diabetes mellitus. Med Mycol. 2006; 44:335–342. PMID: 16772227.
Article9. Spellberg B, Kontoyiannis DP, Fredricks D, Morris MI, Perfect JR, Chin-Hong PV, et al. Risk factors for mortality in patients with mucormycosis. Med Mycol. 2012; 50:611–618. PMID: 22435877.
Article10. Llorente A, Perez-Valero I, García E, Heras I, Fraile V, García P, et al. Mortality risk factors in patients with zygomycosis: a retrospective and multicentre study of 25 cases. Enferm Infecc Microbiol Clin. 2011; 29:263–268. PMID: 21330008.
Article11. Pagano L, Offidani M, Fianchi L, Nosari A, Candoni A, Piccardi M, et al. GIMEMA (Gruppo Italiano Malattie EMatologiche dell'Adulto) Infection Program. Mucormycosis in hematologic patients. Haematologica. 2004; 89:207–214. PMID: 15003897.12. Chamilos G, Lewis RE, Kontoyiannis DP. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clin Infect Dis. 2008; 47:503–509. PMID: 18611163.
Article13. Rapidis AD. Orbitomaxillary mucormycosis (zygomycosis) and the surgical approach to treatment: perspectives from a maxillofacial surgeon. Clin Microbiol Infect. 2009; 15(Suppl 5):98–102. PMID: 19754767.
Article14. Gamaletsou MN, Sipsas NV, Roilides E, Walsh TJ. Rhino-orbital-cerebral mucormycosis. Curr Infect Dis Rep. 2012; 14:423–434. PMID: 22684277.
Article15. Groll AH, Giri N, Petraitis V, Petraitiene R, Candelario M, Bacher JS, et al. Comparative efficacy and distribution of lipid formulations of amphotericin B in experimental Candida albicans infection of the central nervous system. J Infect Dis. 2000; 182:274–282. PMID: 10882607.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rhinocerebral mucormycosis: a case report
- Massive Cerebral Infarction Due to Rhinocerebral Mucormycosis
- Clinical Study of Rhinocerebral Mucormycosis
- A Case of Rhinocerebral Mucormycosis Misdiagnosed as Herpes Zoster
- A case of successful posaconazole salvage therapy for rhinocerebral mucormycosis after failure of amphotericin B